Abstract
Purpose
This study was to determine factors associated with individuals presenting late with advanced glaucomatous optic nerve damage.
Methods
A case–control study recruiting 123 patients with early features of primary open angle glaucoma (control) and 93 patients with advanced glaucoma (cases) was carried out for risk-factor analysis. Exposures of interest included those already established as major risk factors for glaucoma. These were initial intraocular pressure (IOP), age, and family history. In addition, occupation, ethnic origin, history of diagnosis of diabetes mellitus, hypertension, sickle cell disease, and previous eye examination were of interest.
Results
Univariate analysis showed that initial IOP>31?mmHg, age of >?60years, absence of family history of glaucoma, occupational grouping, ethnicity, and male sex were associated with advanced glaucoma at presentation. Adjusted odds ratio or by multiple logistic regression model showed that initial IOP>31?mmHg in a patient was more likely to present with advanced glaucoma (OR 2.66, 95% confidence interval (CI) 1.45, 4.91; P-value 0.0017) than lower pressures. Patients aged 60–69 years (OR 2.53, 95% CI 1.01, 6.31; P-value 0.0473) and 70–90 years (OR 5.16, 95% CI 1.97, 13.51; P-value 0.0008) were more likely to present with advanced glaucoma than younger ones
Conclusions
Subjects with initial IOP>31?mmHg were nearly three times more likely to present with advanced glaucoma than those with IOP<32?mmHg. Subjects over the age of 60 years were more than two times likely to present with advanced glaucoma than younger subjects.
Similar content being viewed by others
Introduction
Primary open angle glaucoma (POAG) causes permanent blindness. There is progressive optic nerve damage over several years. The last nerve fibres destroyed are those responsible for central vision. The glaucoma patient's vision becomes impaired and eventually he/she becomes totally blind if the condition is not well controlled. Visual impairment therefore comes late in the course of POAG.
In developed countries, most individuals with glaucoma receive treatment in time to preserve their vision. However, in Ghana (as in most developing countries) diagnosis is late, treatment is less available,1 and glaucoma ranks as the leading cause of permanent blindness.2 Studies from Ghana and the West African subregion indicate that glaucoma is common and competes with cataract as the major cause of blindness.3, 4, 5, 6, 7 A hospital-based study showed that POAG was responsible for about one-third of blindness in Southern Ghana.2
Quigley's8 review of the world literature showed that in developed countries, fewer than 50% of those with glaucoma are aware of their disease and in the developing world, the rate of known disease is even lower. Glaucoma patients present with various stages of the disease at the time of diagnosis. Unfortunately, some present with advanced disease involving central vision and/or total blindness. There is significant evidence that late presentation of glaucoma is an important risk for glaucoma blindness.1 However, there is a paucity of literature on why some people have early stages of POAG and others advanced disease at diagnosis. It is possible that factors other than chronology (ie late presentation of long standing disease) are responsible for advanced features of POAG at diagnosis. Identification of such factors may help in planning strategies to reduce visual loss and blindness from glaucoma. Two recent studies have sought to address this issue.9, 10 These studies estimated that in England, factors associated with late presentation of glaucoma were the initial intraocular pressure (IOP), family history of glaucoma, and lower socioeconomic status. They also found that persons of African-Carribean origin were more likely to attend with advanced glaucoma compared to white patients. No previous attempts have been made to identify factors associated with late presentation of glaucoma in an African-African population. This study evaluates factors in the Ghanaian African that may be associated with increased risk of visual field loss from glaucoma (ie advanced glaucoma) at diagnosis. Exposures of interest included those already established as major risk factors for glaucoma including IOP increasing age, and family history. In addition, occupation, ethnicity (tribe), diagnosis of diabetes mellitus, hypertension, and sickle cell disease, as well as previous eye examination and treatment were evaluated.
Materials and methods
The study was of case–control design recruiting
-
1)
Individuals newly diagnosed with POAG in the Akwapim South district Population-based Glaucoma Prevalence Survey11 and
-
2)
newly diagnosed patients with POAG in two hospitals in Accra.
The study was undertaken over a 12-month period from August 2000 to July 2001. After the diagnosis of POAG was made patients were recruited if they satisfied the criteria for a case or control, and gave consent to be included in the study. None of the eligible subjects declined inclusion in the study. Any patients with previous history of glaucoma, ocular hypertension, or suspected glaucoma were excluded from the study. All the patients were assessed by the same investigator (CTNA) to ensure consistency of case definition. The criteria for a case were patients had to have a typicalglaucomatous cupping appearance of the optic nerve head with cup/disc (c/d) ratio >0.8 in one or both eyes and repeatable extensive visual field loss including absolute scotoma(s) within 5° of fixation in the same eye. The criteria for a control were patients with c/d ratio of 0.5 or greater in one or both eyes or a difference of 0.2 or more between c/d, and no absolute scotomas within 20° of fixation of the visual field in either eye.
Background demographic information, personal and family, general medical, and ocular history was taken by three of the authors (RKE, REK and ENC) who were involved in recruiting the subjects and was crosschecked by the principal author. Information including age, sex, family history of glaucoma, medical history including diagnosis and treatment of diabetes, hypertension, and sickle cell disease, as well as previous ocular history (last eye test or examination and by whom) and occupational classification were obtained. Patient's occupational group was initially determined using the Standard Occupational Classification.12 Where the patient was retired, unemployed, or suffered a long illness the occupation longest undertaken was entered. However, it became obvious that it was sometimes difficult to distinguish between some of the different occupational categories. A two band occupational grouping of higher (comprising I–IIIN) and lower (comprising IIIM–V) socioeconomic classification was adopted. Examination included IOP measurement by Goldmann's applanation tonometry, visual fields (Humphrey 24-2) recording, and fundus biomicroscopy with detailed optic disc assessment with a 78?D lens. Resources could not support investigations for diagnosing diabetes, sickle cell disease, and hypertension. A patient was recorded as diabetic, therefore, if there was a positive history of diabetes and the patient is on treatment including diet, tablets, and or insulin. Similarly, he was considered hypertensive if there was a positive history of current treatment for hypertension and to have sickle cell disease if there was a positive history of sickle cell disease confirmed by haemoglobin electrophoresis. The ethics of the study protocol was approved by the University of Ghana Graduate Studies Board and complied with the Declaration of Helsinki on human subjects.
Statistical analysis
A determined sample size of 220 (consisting of 110 cases and 110 controls) would give an 80% chance of detecting as statistically significant at the 5% level a doubling in the odds of advanced glaucoma in a risk factor present among 10% of the controls. The associations between risk factors for advanced glaucoma were assessed by calculating odds ratios (ORs), for each factor, of late presentation (or advanced glaucoma) by univariate analysis and adjusted OR (with 95% confidence intervals (CI)) by multiple logistic regression model of factors including age, sex, family history, IOP, occupational grouping, and tribe.
Results
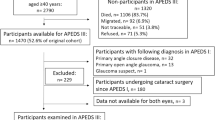
In all, 216 subjects were recruited for this study: 93 cases (24 population survey, 69 hospital) and 123 controls (29 population survey, 94 hospital). There was no significant difference between case/control mixture from the population and that from the hospital (x2 test P-value: 0.71). A total of 16 patients, consisting of five cases and 11 controls, had juvenile POAG (JPOAG). In all, 200 patients, consisting of 88 cases and 112 controls, had adult POAG (APOAG). There were 66 female and 57 male controls. The cases included 44 female and 49 male subjects. The age group and gender distribution of the sample are shown in Table 1. No significant difference in sex distribution was found between the two groups using x2-test (P-value 0.8). The mean age at diagnosis of glaucoma was 54 years (median 56 years and SD 14.8). For the control group, the mean age was 54 years (median 53 years and SD 15.2) while the mean age of diagnosis for the cases was 57 years (median age 61 years and SD 14.8). In all, 15.3% (33 patients) had normal tension glaucoma (NTG), and 79.6% (172 patients) high tension glaucoma (HTG). The remaining 5.1% (11 patients) had poor cooperation during IOP measurement or incomplete IOP data entry and were excluded from the IOP analysis.
There were only three eyes in two patients with myopia worse than −5.00?DS. Positive history of existing systemic disease was obtained in 10 patients. These included four hypertensives, two diabetics and two with both diabetes and hypertension, and two asthmatics.
The question designed to find the time interval between the last eye examination by an eye care personnel and recruitment into this study was abandoned because the validity of the responses were low. Most patients recruited into the study could not distinguish between eye care workers, other healthcare staff, and people with no formal training who sold spectacles. Table 2 summarises the frequency of studied factors among cases and controls.
Table 3 shows the univariate analysis and the adjusted ORs of glaucoma by multiple logistic regression model. IOP of >31?mmHg was significantly associated with late attendance with advanced glaucoma. Patients with IOP >31?mmHg were about three times more likely to present late with advanced glaucoma than those with lower IOP. Absent family history, lower occupational groups, and non-Akan tribe were other independent variables that appeared to be associated with late presentation of glaucoma in the univariate analysis; however, these were not statistically significant. An individual without a family history of glaucoma appeared about twice more likely to present with advanced glaucoma than one with a family history. This was especially so in vertical (parent–child) relations. When adjusted ORs for glaucoma associations by the multiple logistic regression model were analysed, only the IOP and age at presentation were found to be significant. An IOP>31?mmHg at presentation was about 3 times more likely to be associated with advanced glaucoma than IOP of 31?mmHg or less (OR 2.66, P = 0.0017, 95% CI 1.45, 4.91). Patients in the seventh decade of life were 2.5 times more likely (OR 2.53, 95% CI 1.01, 6.31, P = 0.0473), while those in the eighth decade or older were 5 times more likely (OR 5.16, 95% CI 1.97, 13.51, P = 0.0008) to present advanced than those in the fourth decade. Other associations at the univariate analysis were not significant in the multiple regression model.
Discussion
Several previous studies have shown that patients with advanced glaucoma have an increased risk of blindness13, 14, 15, 16, 17 and that late attendance is a significant risk for subsequent blindness.9, 11 The present study attempts to elucidate the risk factors associated with late presentation in a Ghanaian population. The patients were chosen with standard criteria irrespective of the source and the inclusion of approximate numbers of cases and controls from the different sources would remove any bias. Furthermore, since standard criteria were used to determine cases and controls the use of different distinct centres may actually provide a more representive cohort. Referrals to the hospital eye service in Ghana are usually from the mass screening exercises of ophthalmic nurses and a few practising optometrists in addition to direct presentation by symptomatic patients. It is, however, possible that there may be some bias associated with the community selected cases since NTG is generally underdiagnosed in hospital practice compared to screening programs.
This study shows the effect of high IOP on visual field loss in Ghanaian individuals with glaucoma. Our findings are consistent with results of previous studies from other communities that showed that higher IOPs result in more rapid visual field loss and are associated with an increased likelihood of late presentation.9, 18, 19, 20, 21 A significant clinical implication of this finding is that it provides a measure of relative urgency required in managing patients with IOP's higher than 31?mmHg because they stand a three times more chance of developing rapid optic nerve damage compared to those with IOP of 31?mmHg or less. However, this relative risk assessment does not apply to patients with NTG, since by definition, their IOPs will be in the normal range. The IOP data used in this study are one-off measurements obtained at the initial hospital examination, by the nature of the study. It may be that prolonged follow-up would have found that some of the patients with NTG converted to high tension POAG at a later date.9 It is also possible that the IOP rises gradually in the early course of POAG, but as the pressure rises the optic nerve damage and field defect may accelerate. It has been suggested that as the optic nerve damage increases the remaining nerve fibres may become more vulnerable to damage.17
Increasing age from the seventh decade was significantly associated with glaucoma visual field loss. This finding is not surprising because the incidence and prevalence of glaucoma increase with age. Fraser et al 9, 10 also showed a general trend of increasing risk of late presentation with age, although their results did not show a significant association between late presentation and increasing age. Our study shows a steeper increased risk of advanced glaucoma with increasing age at both the independent and adjusted levels. This rising trend for advanced disease with age is steeper in the present study than previously reported.9, 10 Jay and Murdoch17suggested that the difference in average age at presentation for the early stage of glaucoma (comparable to our controls) and the late stage (comparable to our advanced disease ie cases) may provide an estimate of the average rate of progression of field loss before diagnosis and treatment.17 If this hypothesis is true, then the small difference of 3 years between the mean ages for the controls and cases may indicate that the rate of progression of field loss is rapid in our study group. This viewpoint supports the general conception that POAG in people of African origin runs a more aggressive course than in the Caucasian. Put in the right perspective, a Ghanaian-African patient of 60 years or older age with an IOP>31?mmHg is more likely to progress to an advanced or end-stage glaucoma than patients of non-African origin.
Family history is a major risk factor for glaucoma and there is a growing body of evidence that glaucoma is a familial disease.9, 22, 23, 24, 25 It is interesting that a positive family history of glaucoma, in this study, appears to cut down the risk of late presentation by half in the univariate analysis. However, this association does not reach significance levels in the multiple regression model. It is most likely that family history is protective against late presentation of glaucoma because the increased awareness among family members encourages them to take up screening (glaucoma patients are advised to bring their family members for screening). It is possible that persons with a family history of glaucoma appreciate the need for regular eye tests because information may be passed on from other family members. However, it is probable that the family history data in the present study are incomplete since some of the patients may be unaware of their family history of glaucoma. Although some patients reported multiple family members being affected by glaucoma, over 80% of the positive responses were of a vertical pattern (i.e. children, parents, and grandparents). This observation is contrary to the findings from other studies where the chances of other siblings being affected is higher than that of children.25 The very low count for positive family history among second, degree relatives may not represent the true situation. In light of Ghanaian sociocultural behaviour, this phenomenon is, however, not surprising as the average Ghanaian does not like other relations knowing about their medical history. They find it more difficult to inform siblings and relations other than parent/child of their medical condition.
Since impaired optic nerve perfusion may be responsible for glaucomatous optic nerve damage, it would be important to determine the role of systemic vasculopathies as risk factors in advanced glaucomatous damage. Unfortunately, many of the study participants did not know their blood pressure, or diabetes mellitus, and sickle cell status. The resources available for this study also could not support rigorous investigation for diabetes (fasting blood sugar), sickle cell disease (Hb electrophoresis), and blood pressure monitoring in all cases. The information on these vasculopathies as risk factors in glaucoma optic nerve damage is therefore limited.
One reason for people presenting late with glaucoma is the infrequency of eye examinations.9 This was considered a possible reason for the greater risk of late presentation of Afro-Carribeans with glaucoma in the UK although socioeconomic status was also thought to be important.9, 10 Unfortunately, we were unable to investigate this phenomenon satisfactorily in this present study. One of the objectives of this study was to determine the calibre of eye care personnel who offered the eye care services to the subjects. This would have helped ascertain whether a particular service provider was capable of glaucoma detection or not, since screening for glaucoma requires special skills. In Ghana, some individuals without any formal training sell spectacles, and some nonophthalmic medical and nursing staff without any specialised training in eye care attend to patients with eye problems. Some patients even consult chemical sellers (chemical sellers are persons registered to sell drugs which do not require prescription.) as ‘doctors’ or ophthalmic experts for their eye problems because they may be unaware of the differences between the various service providers. Unfortunately, it was impossible for most participants to indicate as to which category of eye care worker provided their previous eye examination. It was, therefore, impossible to make any meaningful evaluation of the different eye care personnel or the frequency of eye examinations and late presentation of glaucoma. In the UK where similar work was carried out, the driving force behind the presentation is self-initiated visits to the optometrist.9, 10 A previous study has shown that 90% of patients with glaucoma are referred to the hospitals on the basis of abnormal findings by optometrists.26 Most people would require change of spectacles or reading glasses from about the age of 40 years, which incidentally is also about the age glaucoma incidence appears significant. In the UK, the optometrist plays an important role in glaucoma detection, while in Ghana there are only few optometrists and their role in glaucoma referrals at the present time is fairly limited.In both Korle-Bu Teaching and Trust Hospitals referrals are usually from mass screening exercises by ophthalmic nurses providing outreach services or attached to other hospitals and clinics where there are no ophthalmologists, and also employers for routine medical examination.1 These nurses use schiotz tonometer while for the population survey Perkin's applanation tonometer was used for screening. However, the same Goldmann applanation tonometer, regularly calibrated, was used in examining all patients included in this study. Patients who present to the hospital normally would have more advanced stage of the disease compared to those from regular mass screening programme. However, if such screening programme are ad hoc, especially in areas that are underprovided with ophthalmic services, more advanced cases of POAG will be diagnosed.
Socioeconomic status is well known to influence access to as well as compliance with medical treatment and probably determines the frequency of eye tests.9, 27 Similarly, the Baltimore Eye Study found that individuals with lower socioeconomic (occupational) status had higher rates of visual impairment.28, 29 This phenomenon was observed in our study showing the lower occupational groups, at the univariate level, have a higher risk of presenting with advanced glaucoma. It is also possible that the increased awareness associated with higher education (by implication higher socioeconomic status) may explain the reduction in risk of advanced glaucoma in the higher occupational groups. This increased risk may also be explained, at least partly, by differences in frequency of sight tests and the category/calibre of eye care service provider used by the individual, if they exist.
From this study, we conclude that high levels of pretreatment IOP of >31?mmHg and the age of 60 years and above are the most important factors associated with glaucomatous optic neuropathy in the Ghanaian African. Other factors including male sex, absent family history of glaucoma, lower levels of occupation, and ethnicity showed weak associations that did not reach significant levels. Patients with IOP more than 31?mmHg and or older than 60 years, therefore, need more aggressive medical intervention to prevent blindness.
References
Ntim-Amponsah CT . Visual loss in chronic glaucoma patients. Trop Doc 2002; 32: 1–3.
Adu-Darko M . Common causes of blindness in Southern Ghana as seen in Komfo Anokye teaching hospital in Kumasi. Ghana Med J 1991; 25: 280–284.
Akafo S K, Hagan M . Causes of childhood blindness in Southern Ghana—a blind school Survey. Ghana Med J 1990; 24: 113–119.
Wormald R, Foster A . Clinical and pathological features of chronic glaucoma in North-East Ghana. Eye 1990; 4: 107–114.
Verrey JD, Foster A, Wormald R, Akuamoa C . Chronic glaucoma in Northern Ghana A retrospective study of 397 patients. Eye 1990; 4: 115–120.
Olurin O . Causes of blindness in Nigeria—a study of 1,000 hospital patients. West Afr Med J 1973; 22: 97–107.
Stilma JS . Causes and prevalence of blindness in the Northern province of Sierra Leone. Doc Ophthalmol 1983; 56: 115–122.
Quigley HA . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Fraser S, Bunce C, Wormald R . Risk factors for late presentation in chronic glaucoma. Invest Ophthalmol Vis Sci 1999; 40: 2251–2257.
Fraser S, Bunce C, Wormald R . Retrospective analysis of risk factors for late presentation of chronic glaucoma. Br J Ophthalmol 1999; 83: 24–28.
Ntim-Amponsah CT, Amoaku WMK, Ewusi RK, Idirisuriya-Khair R, Nyatepe-Coo E, Ofosu-Amaah S et al. Prevalence of glaucoma in an African population. Eye 2004; 18(5: 491–497.
Office of population Census and Surveys. Standard Occupational Classification Vol 3. Govt Statistical Service, HMSO: London, 1991.
Sommer A, Quigley HA, Robin AL, Miller NR, Katz J, Arkell S . Evaluation of nerve fibre layer assessment. Arch Ophthalmol 1984; 102: 1766–1771.
Grant WM, Burke JF . Why do some people go blind from glaucoma? Ophthalmology 1982; 89: 991–998.
Armaly MF, Krueger DE, Maunder L, Becker B, Hetherington Jr J, Kolker AE et al. Biostatistical analysis of the Collaborative Glaucoma Study I Summary report of the risk factors for glaucomatous visual field defects. Arch Ophthalmol 1980; 98: 2163–2171.
David R, Zangwill L, Stone D, Yassur Y . Epidemiology of intraocular pressure in a population screened for glaucoma. Br J Ophthalmol 1987; 71: 766–780.
Jay JL, Murdoch JR . The rate of visual field loss in untreated primary open angle glaucoma. Br J Ophthalmol 1993; 77: 176–178.
Fruhauf A, Muller F, Sismuth M . Otersuchungen zur Prognose des Glaukoms. Klin Monatbl Augenheikd 1967; 151: 477–485.
Hart WM, Yablonski M, Kas MA, Becker B . Multivariate analysis of risk of glaucomatous visual field loss. Arch Ophthalmol 1979; 97: 1455–1458.
Weih LM, Nanjan M, McCarty CA, Taylor HR . Prevalence and predictors of open-angle Glaucoma. Ophthalmology 2001; 108: 1966–1972.
Leske CM, Connell AMS, Schachat AP, Hyman L . The Barbados Eye Study. Arch Ophthalmol 1994; 112: 821–829.
Stone EM, Fingert JH, Alward WLM, Nguyen TD, Polansky JR, Sunden SLF et al. Identification of a gene that causes primary open angle glaucoma. Science 1997; 275: 668–670.
Craig JE, Mackey DA . Glaucoma genetics: where are we? Where will we go? Curr Opin Ophthalmol 1999; 10: 12–13.
Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt HC . Family history and risk of open angle glaucoma The Baltimore Eye Survey. Arch Ophthalmol 1994; 112: 69–73.
Kanski JJ . Clinical Ophthalmology, 5th Ed. Butterworth-Heinemann: Glasgow, 2003.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR . An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol 1994; 1: 31–38.
Leske MC, Rosenthal J . Epidemiological aspects of open angle glaucoma. Am J Epidemiol 1979; 109: 250–272.
Tielsch JM, Sommer A, Katz J, Royal RM, Quigley HA, Javitt J . Racial variations in the prevalence of primary open angle glaucoma: the Baltimore Eye Survey. JAMA 1991; 266: 369–374.
Tieslch JM, Sommer A, Katz J, Quigley HA, Ezrine S . Socioeconomic status and visual impairment among urban Americans. Arch Ophthalmol 1991; 109: 638–641.
Acknowledgements
Sussie Eshun and Dorothy Fiadoyor plotted the visual fields. James Ntim Amponsah and Alcon/Paracelsus Pharmacy provided financial support. James Ntim Amponsah and Professor Shicheng Yu helped with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ntim-Amponsah, C., Amoaku, W., Ewusi, R. et al. Evaluation of risk factors for advanced glaucoma in Ghanaian patients. Eye 19, 528–534 (2005). https://doi.org/10.1038/sj.eye.6701533
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701533