Abstract
Purpose Although systemic or eyelid involvement by ocular adnexal lymphoma carries a worse prognosis, there have been few reports of the outcome in relation to clinical presentation. The outcome of malignant ocular adnexal lymphoma was, therefore, related to presenting clinical symptoms and signs.
Design and Methods A retrospective, noncomparative case-note review of 326 patients treated in the Orbital Clinic at Moorfields Eye Hospital. The associations between presenting symptoms or signs and three outcome measures (v.i.) were assessed by univariate and multiple variable regression together with Kaplan–Meier analysis.
Main Outcome Measures (i) Presence of extra-orbital disease at the time of presentation; (ii) development of systemic lymphoma after new presentation with solely ocular adnexal disease; and (iii) death attributable to widespread lymphoma.
Results Presentation with disseminated disease was rarer with over 1 year's ophthalmic symptoms (odds ratio (OR) 0.7; 95% CI 0.5–0.9) and much more frequent with bilateral adnexal disease (OR 5.8; 95% CI 3.0–11.2). With solely adnexal disease at presentation, subsequent extra-orbital lymphoma was more frequent and earlier with lacrimal gland disease (as compared to those without; hazard ratio (HR) 1.9; 95% CI 1.2–4.5) or with eyelid disease (compared to those without; HR 2.4; 95% CI 1.2–4.5), or with bilateral disease (compared to unilateral disease; HR 2.6; 95% CI 1.4–5.2).
Prior or concurrent systemic disease was the most significant predictive factor for lymphoma-related death (HR 6.8; 95% CI 4.3–10.9), but tumour-related death was also commoner and earlier with bilateral disease (HR 2.4; 95% CI 1.4–4.0) or where a relative afferent papillary defect was present (HR 2.8; 95% CI 1.6–4.9). Similarly, the rate of tumour-related death was slightly less where symptoms had been present for more than a year (HR 0.8; 95% CI 0.7–1.0) and slightly greater in the elderly (HR 1.03; 95% CI 1.01–1.05). Conjunctival lymphoma had the lowest rate of extra-orbital spread and lymphoma-related death, the rate of these two events being sequentially greater for patients with predominantly deep orbital lymphoma, lacrimal gland lymphoma, or eyelid lymphoma.
Conclusion These data suggest that presenting symptoms and signs of patients with ocular adnexal lymphoma are significantly associated with the risk of systemic disease at orbital presentation, the rate of subsequent spread, and the rate of lymphoma-related death.
Similar content being viewed by others
Introduction
The prognosis for ocular adnexal lymphoma is closely related to histological type1,2 and is considerably worse for patients with high-grade tumours. 1,2,3,4 Likewise, outcome is related to clinical stage at presentation, patients with disseminated disease (stage IVE) having a worse prognosis than localised disease (stage IE).1,2,3 Prognosis is also related to the primary location of the adnexal disease,2,5 eyelid lymphomas having a more aggressive course than orbital or conjunctival disease2,3,4 conjunctival lymphomas having a good prognosis, and patients with conjunctival and deep orbital disease having similar survival.4,5,6,7,8,9 Although not observed in larger studies,2,4,8 a recent small series suggested that lacrimal gland lymphoma presents a greater risk of subsequent systemic disease than orbital disease.10 Survival after unilateral or bilateral adnexal disease is similar,2,4,8,9,10 and there may be an association between bilateral orbital disease and systemic involvement at diagnosis.3 Other clinical features (such as symptom duration, inflammatory symptoms and signs, proptosis, visual function or eye movements) have not been examined in these relatively limited series, the largest having reviewed 112 patients.3
We have analysed the presenting symptoms and signs of 369 patients with adnexal lymphoma, relating these to the extent of disease at presentation and long-term outcome. This analysis is solely designed to guide the clinician when first assessing a patient with a likely diagnosis of ocular adnexal lymphoma, prior to biopsy of the lesion; the histological type of adnexal lymphoma still remaining the most influential determinant of outcome.1
Methods
The associations between several clinical parameters (‘independent’ variables or ‘determinants’; Table 1) and three variables were assessed using logistic regression and Cox proportional hazards. The variables were (i) presence of systemic lymphoma at diagnosis (SLAD), (ii) rate of systemic spread of lymphoma (SSOL) in patients newly presenting with solely adnexal disease, and (iii) rate of lymphoma-related death (LRD).
Various clinical details (Table 1) were gathered by a retrospective review of the case records for 369 patients with a histological diagnosis of lymphoma, presenting to the Orbital Clinic at Moorfields Eye Hospital between 1980 and 1994. Any relative afferent pupillary defect (RAPD) or decreased acuity (two or more Snellen lines) was considered relevant only where it was due to tumour mass. Uniocular ductions were estimated on a scale of 0 – 100 for each of the four cardinal directions, giving a total ‘motility score’ (for uniocular lymphoma) between 0 and 400.
Staging for systemic disease and long-term outcome were determined from notes at Moorfields and the two oncology units to whom patients were referred, and from the patient's general practitioner. Death from lymphoma was confirmed from death certification, hospital records and information from cancer registration agencies and the Office for National Statistics.
Site of disease
The area of predominant adnexal involvement was categorised into deep orbit, lacrimal gland, eyelid or conjunctiva. Disease was considered ‘lacrimal gland’ where it was centred on the gland, even if involving neighbouring areas. ‘Deep orbital’ was considered where the total duction score was 300 or less, or where the globe was displaced in the sagittal or coronal plane by 2 mm or more. Distinct subcutaneous masses in the eyelid (but without deep orbital disease) were classified as ‘eyelid’ lymphoma, as were localised caruncular or lacrimal sac tumours. ‘Conjunctival’ lymphoma was considered where the mass was centred on the pre-equatorial subconjunctival space.
Disseminated lymphoma discovered within 3 months of orbital biopsy was regarded as concurrent ‘SLAD’.
Statistical procedures
SPSS™ software was used to assess the relation between each clinical variable (determinant) and the three dependent variables (Table 1); prior to inclusion, continuous variables were checked for Gaussian normality and, to stabilise its variance, the natural logarithm of ‘symptom duration’ was used. Five variables (age at presentation, symptom duration, proptosis, ptosis, motility restriction) were treated as continuous data.
Those variables occurring in over 10% of patients, and bearing a significant (P<0.01) univariate relationship to any of the three outcome parameters, were retained for multiple regression analysis (Table 2). The relationship of the independent variables to SLAD was examined by logistic regression, whereas the relationship to time-dependent outcome data ‘SSOL’ or ‘LRD’ was examined by Cox modelling and Kaplan–Meier analysis. For all survival models where the confidence interval for the hazard ratio excludes the unity of nonassociation, Schoenfeld residuals were examined. All time-dependent data were related to the time of orbital biopsy.
The whole statistical analysis was conducted to generate hypotheses regarding clinical signs and patient outcome and, with the large number of tests conducted, the results should be treated cautiously.
Results
Of 369 patients with lymphoma, adequate clinical data were available in 326 (88%), this latter study group having a mean age at diagnosis of 66 years (range 3–90) and a median follow-up of 55. 5 months (range 0–434). The frequency of each clinical parameter, and association with the three ‘dependent’ variables are shown in Tables 1 and 2.
Although there are only small numbers later in the follow-up, the Kaplan–Meier survival curves stabilise at about 14 years following biopsy (Figures 1 and 2) and a half of the patients get orbital disease by 5 years after diagnosis and 19% have suffered LRD by this time (Figure 1; Table 3).
Cumulative proportion of patients without extra-orbital lymphoma (SSOL) or without a lymphoma-related death (LRD) for 326 patients presenting with ocular adnexal lymphoma. Patients with no extra-orbital disease at the last follow-up (SSOL line) or who had died without lymphoma (LRD line) are censored. The figures under the graph represent the number of patients alive without extra-orbital lymphoma (SSOL data) or alive at a given time after biopsy (LRD data).
Univariate analysis (Table 1)
No association was found between sex, smoking, or the presence of autoimmune diseases and the three outcome variables although, of no practical significance, there was a marginally greater risk of LRD with age (hazard ratio (HR) 1.03).
Where symptoms are present for more than a year (72/326 cases; 22%), there was a significantly lower rate of SLAD (odds ratio (OR) 0.4) and a lower rate of LRD (HR 0.5). The commonest symptoms were a ‘lump’ or ‘swelling’ (60% of patients, and not associated with any survival parameters) and diplopia (27%), the latter symptom carrying an increased risk of SLAD (OR 2.1).
Pain, not occurring with conjunctival lymphoma, was strongly associated with LRD (HR 3.2). Of the 16 patients with a painful orbital lesion, 10 died of lymphoma, in contrast to one-sixth with painful lacrimal gland lymphoma and none of the two with painful eyelid lymphoma. Although pain was significantly (HR 2.0) associated with the risk of systemic disease at some stage of the disease (known as ‘prior, concurrent or future’ (PCF) spread), there was no association between pain and the individual parameters of spread (SLAD or SSOL).
One-sixth of the group presented with bilateral adnexal disease, this being associated with a significantly increased risk of SLAD (OR 5.2), rate of SSOL (HR 2.4), and rate of LRD (HR 2.2).
A total of 44 patients presented with an RAPD, this being associated with increased rate of LRD (HR 2.6). Of the 44 patients, 39 (87%) had decreased acuity, 20 (45%) had papilloedema, 16 (36%) had marked (>6 mm) displacement of the globe, and 10 (23%) had pain. Although limitation of movement was associated with LRD (Table 1), it was not included in multiple regression analysis because of the strong association with the presence of an RAPD, the latter being a much more reliable sign. Moreover, for ‘limitation of movement’, there is a suggestion that the proportional hazards assumption was not adhered to, with evidence that the hazards ratio increased with time.
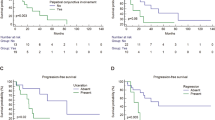
Subcutaneous involvement, associated with a significantly higher rate of SSOL (HR 2.4) and LRD (HR 1.7), was present in 53 (16%; Table 1) patients: 30/53 adnexal tumours were purely in the eyelid and they had a markedly worse prognosis than 23 patients with deep orbital tumours extending into the preseptal tissues (Figure 3). In contrast, the prognosis for 93 patients with subconjunctival lymphoma (Table 1) was relatively good, whether including (Table 1) or excluding (Table 3, Figure 4) deep orbital involvement.
Multiple regression analysis (Table 2)
The risk of SLAD was greater with a shorter duration of symptoms (OR 0.7). or with bilateral disease (OR 5.8). For patients newly presenting with solely adnexal lymphoma, the presence of bilateral disease (HR 2.6), an eyelid mass (HR 2.4), or a lacrimal gland mass (HR 1.9) is associated with a significantly greater rate of SSOL. The rate of LRD is greater with bilateral disease (HR 2.4) and weakly related to symptom duration and age (Table 2).
When included in multiple regression analysis, adnexal presentation with stage IVE disease (ie prior or concurrent disseminated lymphoma) was a more powerful determinant of LRD than bilaterality: the estimated HR for LRD (adjusted for age and RAPD) in such patients with stage IVE disease was 6.8 (95% CI 4.3–10.9).
Site of predominant adnexal disease and sites of extra-orbital spread (Tables 3 & 4)
The frequency of SSOL (Figure 5) and LRD (Figure 6) increased progressively through anatomical categories—from ‘conjunctival’ lymphoma, to ‘deep orbital’, to ‘lacrimal gland’, to purely ‘eyelid’ lymphoma. A similar progressive increase in morbidity and mortality across these anatomical categories was also observed for the subgroup of patients newly presenting with solely adnexal disease (Figure 7).
Patients with conjunctival lymphoma had the lowest incidence of prior lymphoma (1%) or future spread (21%), these lymphomas most often spreading to lymph nodes (24%) and only rarely (3%) showing direct extra-orbital invasion. Deep orbital lymphomas were mainly unilateral (91%) and had the lowest incidence (13%) of SLAD, but tend to invade locally (13%) with 7% involvement of paranasal sinuses. In contrast, lacrimal gland lymphomas rarely invaded locally (5%) and most commonly spread to lymph nodes (43%). Eyelid lymphoma has the highest rate of prior lymphoma (14%), rate of concurrent local extension (10%—usually to the cheek, forehead, or temporalis fossa), and rate of SLAD (34%).
The rate of LRD for patients with deep orbital lymphoma is greatest where there is painful optic neuropathy, less in cases of painless optic neuropathy and least where there is neither pain nor an RAPD (Figure 8). Involvement of paranasal sinuses or temporalis fossa was present at the time of diagnosis in 11/33 patients with orbital lymphoma and an RAPD.
Proportion of patients presenting with deep orbital lymphoma (not involving conjunctiva or lacrimal gland) who remain without lymphoma-related death (‘LRD’). Patients were divided into (A) those who complained of pain, (B) those with a relative afferent papillary defect but no pain, and (C) those without pain or a relative afferent pupillary defect.
Discussion
Histological type is predictive for outcome in patients with ocular adnexal lymphoma,1,2,3,4 but clearly clinical signs also provide a useful guide to the probability of systemic disease, disease relapse, and mortality as a result of lymphoma.
Risk of systemic involvement
Concurrent SLAD or prior lymphoma
Extra-orbital disease, the presence or absence of which significantly alters the choice of treatment for adnexal lymphoma, was detected in 19% at the time of ophthalmic presentation. Patients with symptoms for a year or more were half as likely to have SLAD and were less likely to suffer LRD (Table 1), suggesting that such patients have a lymphoma of relatively benign phenotype.
Of patients with bilateral disease, 46% had SLAD—compared to 14% where signs were unilateral (OR 5.2; Table 1)—this being in contradistinction to the widely held view that unilateral and bilateral diseases are clinically similar.2,4,8,9,10,11 Logically, bilateral disease must either be extra-orbital lymphoma that has spread to both orbits, or ‘primary’ adnexal tumour that has spread to the opposite side, and the two scenarios may be represented by bilateral eyelid lymphoma (with 3/7 patients having prior lymphoma) and conjunctival disease (with none of 16 patients having a prior history). Conjunctival lymphoma might display similar properties to some cutaneous lymphomas, which can occur at symmetrical sites,12 possibly as a result of a ‘homing’ of neoplastic B lymphocytes onto specific adhesion molecules in these tissues.13,14
In all 23 (7%) patients had a history of prior lymphoma, often presenting with a caruncular2 or superotemporal10 mass—clinical presentations also associated with SSOL (Table 1).
Future systemic disease (SSOL) in patients presenting with solely adnexal disease
The patient presenting with bilateral solely ophthalmic disease is more likely to develop SSOL (HR 2.3), this suggesting that these patients may already have occult systemic spread (or a tumour of occult systemic origin). The phenotypic heterogeneity of ocular adnexal lymphoma is displayed by the greater risk of SSOL with lacrimal gland or eyelid tumours, compared with conjunctival disease (Figure 4).
Prior, concurrent, and future (PCF) spread
As in other studies,4,8,9,10 extra-orbital disease occurred at some stage (PCF spread) in about half of the patients but, in contrast to other studies, we found a significant association between bilateral disease and PCF spread (HR 2.9, 95% CI 2.0–4.2).
PCF spread is rarest with conjunctival lymphoma but, compared with deep orbital disease, there are only minor differences—as noted in previous studies.4,8,9 Previously observed,8,9 but only recently confirmed statistically,10 PCF spread of lacrimal gland lymphoma is more frequent than deep orbital lymphoma (Table 3) or nonlacrimal adnexal lymphomas (HR 1.6, 95% CI 1.1–2.2).
Risk of LRD
A quarter of this series' patients had LRD, comparable with other published mortalities of 7.4 and 23%,3,14 and the 5-year mortality was 19% and the 10-year mortality was 33% (Table 3).
Clinical parameters at presentation associated with LRD were duration of symptoms, age, and the presence of bilateral disease or optic neuropathy (as manifested by an RAPD) (Table 2). Increasing age (of poor prognosis for other B-cell lymphomas15) was predictive for LRD in the present study. Likewise, many of the 44 patients with optic neuropathy had high-grade lymphomas or involvement of the paranasal sinuses. Painful optic neuropathy, associated with a poor prognosis (Tables 1 and 2), has not previously been reported and—while pain is more typical of inflammatory disease16—it may be an important marker of aggressive orbital lymphoma (Figure 7).
Patients with solely lid disease had a worse prognosis than those with lid and orbital involvement (Figure 4), whereas conjunctival lymphomas with or without deep orbital involvement had a similar prognosis.
The present study confirmed the significant association between LRD and the clinical stage at diagnosis (reported by some,2,4,8 but not all,9 workers) but, after adjustment for stage, only age and the presence of optic neuropathy remained predictive for reduced patient survival. The rate of LRD is similar in patients with bilateral solely adnexal disease and unilateral involvement and so, while some may have occult systemic disease, it is reasonable to continue treating these patients as stage IE disease.
In conclusion, the symptoms and signs of patients with ocular adnexal lymphoma were good indicators of clinical course: patients presenting with symptoms for more than a year prior to biopsy were less likely to have widely disseminated disease at diagnosis or to subsequently die of lymphoma. Bilateral disease is associated with a higher frequency of disseminated lymphoma and, indirectly therefore, of LRD. Likewise, patients with lacrimal gland or eyelid lymphoma have a higher risk of systemic disease and LRD, as compared with those having conjunctival or deep orbital disease. Finally, patients presenting with optic neuropathy (13% of the study population) or with pain had a higher risk of LRD.
References
Jenkins C, Rose GE, Bunce C et al. Histological features of ocular adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Brit J Ophthalmol 2000; 84: 907–913.
Coupland SE, Krause L, Delecluse HJ et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology 1998; 105: 1430–1441.
Bessell EM, Henk JM, Wright JE et al. Orbital and conjunctival lymphoma treatment and prognosis. Radiother Oncol 1988; 13: 237–244.
Knowles DM, Jakobiec FA, McNally L et al. Lymphoid hyperplasia and malignant lymphoma occurring in the ocular adnexa (orbit, conjunctiva, and eyelids): a prospective multiparametric analysis of 108 cases during 1977 to 1987. Hum Pathol 1990; 21: 959–973.
McGavic JS . Lymphomatoid diseases involving the eye and its adnexa. Arch Ophthalmol 1943; 30: 179–193.
Zimmerman LE . Lymphoid tumors. In: Boniuk M (ed). Ocular and Adnexal Tumors: New and Controversial Aspects. CV Mosby Co: St Louis; 1964, pp 429–458.
Sigelman J, Jakobiec FA . Lymphoid lesions of the conjunctiva: relation of histopathology to clinical outcome. Ophthalmology 1978; 85: 818–843.
Ellis JH, Banks PM, Campbell RJ et al. Lymphoid tumors of the ocular adnexa. Clinical correlation with the working formulation classification and immunoperoxidase staining of paraffin sections. Ophthalmology 1985; 92: 1311–1324.
Medeiros LJ, Harmon DC, Linggood RM et al. Immunohistologic features predict clinical behavior of orbital and conjunctival lymphoid infiltrates. Blood 1989; 74: 2121–2129.
White VA, Gascoyne RD, McNeil BK et al. Histopathologic findings and frequency of clonality detected by the polymerase chain reaction in ocular adnexal lymphoproliferative lesions. Mod Pathol 1996; 9: 1052–1061.
White WL, Ferry JA, Harris NL et al. Ocular adnexal lymphoma: a clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology 1995; 102: 1994–2006.
Goudie RB, Soukop M, Dagg JH et al. Hypothesis: symmetrical cutaneous lymphoma. Lancet 1990; 335: 316–318.
Roos E . Adhesion molecules in lymphoma metastasis. Semin Cancer Biol 1993; 4: 285–292.
Berlin C, Berg EL, Briskin MJ et al. Alpha 4 beta 7 integrin mediates lymphocyte binding to the mucosal vascular addressin MAdCAM-1. Cell 1993; 74: 185–195.
Berger F, Felman P, Sonet A et al. Nonfollicular small B-cell lymphomas: a heterogeneous group of patients with distinct clinical features and outcome. Blood 1994; 83: 2829–2835.
Orcutt JC, Garner A, Henk JM et al. Treatment of idiopathic inflammatory orbital pseudotumours by radiotherapy. Brit J Ophthalmol 1983; 67: 570–574.
Acknowledgements
We are most grateful for the advice and assistance given by Dr JM Henk FRCR, Professor Susan Lightman FRCP, and Mr Garry Davis FRACO. Mr Christopher Jenkins received support, during this work, with a research grant from Guide Dogs for the Blind.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenkins, C., Rose, G., Bunce, C. et al. Clinical features associated with survival of patients with lymphoma of the ocular adnexa. Eye 17, 809–820 (2003). https://doi.org/10.1038/sj.eye.6700379
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700379
Keywords
This article is cited by
-
Ocular lymphoma: overcoming a diagnostic challenge with an endoscopic sinus approach
Irish Journal of Medical Science (1971 -) (2024)
-
Orbital and ocular adnexal lymphoma: a review of epidemiology and prognostic factors in Taiwan
Eye (2021)
-
Ocular adnexal lymphoma: long-term outcome, patterns of failure and prognostic factors in 174 patients
Journal of Hematopathology (2021)
-
Malignant Orbital Tumors: Current Approach to Diagnosis and Management
Current Ophthalmology Reports (2021)
-
Augenbefall und Systemerkrankung – periokuläre und intraokuläre Lymphome
Der Onkologe (2020)