Abstract
Objective:
To acquire information about nutritional problems and factors associated with them in all nursing homes in Helsinki, Finland.
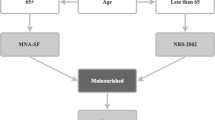
Design:
Descriptive, cross-sectional study. The residents were assessed by the Mini Nutritional Assessment test (MNA) and information was gathered about residents' backgrounds, functional status, diseases and about daily routines in institutions providing nutritional care.
Setting:
All nursing homes in Helsinki community, the capital of Finland.
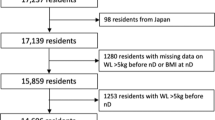
Subjects:
Of 2424 eligible subjects, 2114 (87%) aged residents, mean age 82 y, were examined.
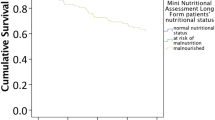
Results:
One-third (29%) of the studied residents suffered from malnutrition (MNA<17), and 60% were at risk (MNA 17–23.5). Malnutrition was associated with the female gender, a longer stay in the nursing home, functional impairment, dementia, stroke, constipation and difficulties in swallowing. In addition, eating less than half of the offered food portion, not eating snacks and resident's weight control at long intervals were associated with malnutrition. In logistic regression analysis mainly patient-related factors predicted malnutrition: impaired functioning (OR 3.71, 95% CI 2.76–4.99), swallowing difficulties (OR 3.03, 95% CI 2.10–4.37), dementia (OR 2.06, 95% CI 1.45–2.93), constipation (OR 1.84, 95% CI 1.38–2.47), but also eating less than half of the offered food portion (OR 3.03, 95% CI 2.21–4.15).
Conclusions:
Although internal factors explain most about the poor nutritional status of aged residents in nursing homes, the factors related to nutritional care need further investigation to clarify their role in maintaining the nutritional status of aged residents.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abbasi AA & Rudman D (1994): Undernutrition in the nursing home: prevalence, consequences, causes and prevention. Nutr. Rev. 52, 113–122.
Abbasi AA & Rudman D (1993): Observations on the prevalence of protein–calorie undernutrition in VA nursing homes. J. Am. Geriatr. Soc. 41, 117–121.
Barret-Connor E (1996): Weight loss precedes dementia. J. Am. Geriatr. Soc. 44, 1147–1152.
Blandford G, Watkins LB, Mulvihill MN & Taylor B (1998): Assessing abnormal feeding behavior in dementia: A taxonomy and initial findings. In: Weight Loss & Eating Behaviour in Alzheimer's Patients. Research and Practice in AD, eds Vellas B, Riviere S, Fitten J. New York: Serdi Publishing Company.
Christensson L, Unosson M & Ek AC (2002): Evaluation of nutritional assessment techniques in elderly people newly admitted to municipal care. Eur. J. Clin. Nutr. 56, 810–818.
Compan B, di Castri A, Plaze JM & Arnaud-Battandier F (1999): Epidemiological study of malnutrition in elderly patients in acute, sub-acute and long-term care using MNA. J. Nutr. Health Aging 3, 146–151.
Crogan NL & Pasvogel A (2003): The influence of protein–calorie malnutrition on quality of life in nursing homes. J. Gerontol. A. Biol. Sci. Med. Sci. 58, 159–164.
Cronin-Stubbs D, Beckett LA, Scherr PA, Field TS, Chown MJ, Pilgrim DM, Bennett DA & Evans DA (1997): Weight loss in people with Alzheimer's disease: a prospective population based analysis. BMJ 314, 178–179.
Dey DK, Rothenberg E, Sundh V, Bosaeus I & Steen B (2001): Body mass index, weight change and mortality in the elderly. A 15 y longitudinal population study of 70 y olds. Eur. J. Clin. Nutr. 55, 482–492.
Gerber V, Krieg MA, Cornuz J, Guigoz Y & Burckhardt P (2003): Nutritional status using the Mini Nutritional Assessment questionnaire and its relationship with bone quality in a population of institutionalized elderly women. J. Nutr. Health Aging 7, 140–145.
Gil Gregorio P, Ramirez Diaz SP, Ribera Casado JM & DEMENU Group (2003): Dementia and nutrition. Intervention study in institutionalized patients with Alzheimer disease. J. Nutr. Health Aging 7, 304–308.
Guigoz Y, Lauque S & Vellas BJ (2002): Identifying the elderly at risk for malnutrition the Mini Nutritional Assessment. Clin. Geriatr. Med. 18, 737–757.
Hildebrandt GH, Dominguez LB, Schork MA & Loesche WJ (1997): Functional units, chewing, swallowing, and food avoidance among the elderly. J. Prosthet. Dent. 77, 588–595.
Lamy M, Mojon P, Kalykakis G, Legrand R & Butz-Jorgensen E (1999): Oral status and nutrition in the institutionalized elderly. J. Dent. 27, 443–448.
Lauque S, Arnaud-Battandier F, Mansourian R, Guigoz Y, Paintin M, Nourhashemi F & Vellas B (2000): Protein–energy oral supplementation in malnourished nursing-home residents. A controlled trial. Age Ageing 29, 51–56.
Lesourd BM (1997): Nutrition and immunity in the elderly: modification of immune responses with nutritional treatments. Am. J. Clin. Nutr. 66, 478S–484S.
Magri F, Borza A, del Vecchio S, Chytiris S, Cuzzoni G, Busconi L, Rebesco A & Ferrari E (2003): Nutritional assessment of demented patients: a descriptive study. Aging Clin. Exp. Res. 15, 148–153.
Milne AC, Potter J & Avenell A (2002): Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst. Rev. (3), CD003288.
Mojon P, Budtz-Jörgensen E & Rapin CH (1999): Relationship between oral health and nutrition in very old people. Age Ageing 28, 463–468.
Morley JE (2001): Decreased food intake with aging. J. Gerontol. A. Biol. Sci. Med. Sci. 56, 81–88.
Morley JE & Silver AJ (1995): Nutritional issues in nursing home care. Ann. Intern. Med. 123, 850–859.
Morris JN, Fries BE & Morris SA (1999): Scaling ADLs within the MDS. J. Gerontol. A Biol. Sci. Med. Sci. 54, M546–M553.
Odlund Olin A, Armyr I, Soop M, Jerstrom S, Classon I, Cederholm T, Ljungren G & Ljungqvist O (2003): Energy-dense meals improve energy intake in elderly residents in a nursing home. Clin. Nutr. 22, 125–131.
Pokrywka HS, Koffler KH, Remsburg R, Bennett RG, Roth J, Tayback M & Wright JE (1997): Accuracy of patient care staff in estimating and documenting meal intake of nursing home residents. J. Am. Geriatr. Soc. 45, 1223–1227.
Potter JM (2001): Oral supplements in the elderly. Curr. Opin. Clin. Nutr. Metab. Care 4, 21–28.
Potter J, Langhorne P & Roberts M (1998): Routine protein supplementation in adults: systematic review. BMJ 317, 495–501.
Saletti A, Lindgren EY, Johansson L & Cederholm T (2000): Nutritional status according to mini nutritional assessment in an institutionalized elderly population in Sweden. Gerontology 46, 139–145.
Simmons SF & Reuben D (2000): Nutritional intake monitoring for nursing home residents: a comparison of staff documentation, direct observation, and photography methods. J. Am. Geriatr. Soc. 48, 209–213.
Singer P (2002): Nutrition care to prevent and heal pressure ulcers. Isr. Med. Assoc. J. 4, 713–716.
Snowden M, McCormick W, Russo J, Srebnik D, Comtois K, Bowen J, Teri L & Larson EB (1999): Validity and responsiveness of the minimum data set. J. Am. Geriatr. Soc. 47, 1000–1004.
Suominen M, Laine T, Routasalo P, Pitkala KH & Rasanen L (2004): Nutrient content of served food, nutrient intake and nutritional status of residents with dementia in a finnish nursing home. J. Nutr. Health Aging 8, 234–238.
Takala JK, Mattila KJ & Ryynanen OP (1994): Overweight, underweight and mortality among the aged. Scand. J. Prim. Health Care 12, 244–248.
Van Nes MC, Herrmann FR, Gold G, Michel JP & Rizzoli R (2001): Does the mini nutritional assessment predict hospitalization outcomes in older people? Age Ageing 30, 221–226.
Vellas BJ, Guigoz Y & Garry PJ (1997): Facts Research and Intervention in Geriatrics: Nutrition in the Elderly. The Mini Nutritional Assessment (MNA) 3rd Edition. Paris: Serdi Publishing.
Wells JL, Seabrook JA, Stolee P, Borrie MJ & Knoefel F (2003): State of the art in geriatric rehabilitation. Part II: clinical challenges. Arch. Phys. Med. Rehabil. 84, 898–903.
Wendland BE, Greenwood CE, Weinberg I & Young KW (2003): Malnutrition in institutionalized seniors: the iatrogenic component. J. Am. Geriatr. Soc. 51, 85–90.
Acknowledgements
This study is part of a larger study, which the City of Helsinki has organized in order to develop the nutritional care of the elderly nursing home residents. Great thanks to the personnel in the nursing homes for their cooperation during the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantor: KH Pitkala.
Contributors: MS, SM, PR, HS, IS-U, AP, HF-S and KP have all participated in planning and organizing the study and writing the article. KP analyzed the data.
Rights and permissions
About this article
Cite this article
Suominen, M., Muurinen, S., Routasalo, P. et al. Malnutrition and associated factors among aged residents in all nursing homes in Helsinki. Eur J Clin Nutr 59, 578–583 (2005). https://doi.org/10.1038/sj.ejcn.1602111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602111
Keywords
This article is cited by
-
What about the fundamentals of nursing—its interventions and its continuity among older people in need of home- or facility-based care: a scoping review
BMC Nursing (2024)
-
Oropharyngeal dysphagia and associated factors among individuals living in nursing homes in northern Sweden in 2007 and 2013
BMC Geriatrics (2022)
-
Dietary fat intake and quality in long-term care residents in two cohorts assessed 10 years apart
BMC Nutrition (2022)
-
Swallowing disorders and associated factors in older adults living in nursing homes
European Archives of Oto-Rhino-Laryngology (2022)
-
Effects of an individualised nutritional intervention to tackle malnutrition in nursing homes: a pre-post study
European Geriatric Medicine (2022)