Abstract
Data sources
Cochrane Effective Practice and Organisation of Care (EPOC) Group's Specialised Register; Cochrane Oral Health Group's Specialised Register; the Cochrane Central Register of Controlled Trials Medline; Embase; CINAHL; Cochrane Database of Systematic Reviews; Database of Abstracts of Reviews of Effectiveness; five other databases and two trial registries. A number of dental journals were hand-searched and a grey literature search preformed.
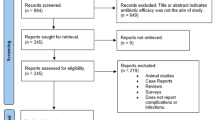
Study selection
Randomised controlled trials (RCTs), non-randomised controlled trials (NRCTs), controlled before and after studies (CBAs) and interrupted time series (ITSs) were considered. Selection was conducted independently by two reviewers.
Data extraction and synthesis
Three reviewers extracted data and assessed risk of bias. Meta-analysis was not possible so a narrative summary was presented.
Results
Four studies evaluated sealant placement; three found no evidence of a difference in retention rates of those placed by dental auxiliaries and dentists over a range of follow-up periods (six to 24 months). One study found that sealants placed by a dental auxiliary had lower retention rates than ones placed by a dentist after 48 months (9.0% with auxiliary versus 29.1% with dentist); but the net reduction in the number of teeth exhibiting caries was lower for teeth treated by the dental auxiliary than the dentist (three with auxiliary versus 60 with dentist, P value < 0.001). One study showed no evidence of a difference in dental decay after treatment with fissure sealants between groups. One study comparing the effectiveness of dental auxiliaries and dentists performing ART reported no difference in survival rates of the restorations (fillings) after 12 months.
Conclusions
We only identified five studies for inclusion in this review, all of which were at high risk of bias, and four were published more than 20 years ago, highlighting the paucity of high-quality evaluations of the relative effectiveness, cost-effectiveness and safety of dental auxiliaries compared with dentists in performing clinical tasks. No firm conclusions could be drawn from the present review about the relative effectiveness of dental auxiliaries and dentists.
Similar content being viewed by others
Commentary
Inequitable or limited access to oral health services is seen in a wide range of countries whether they are considered to be high-, middle-, or low-income economies. Task shifting or labour substitution where typically the focus is on moving work from a more expensive worker to a less expensive alternative is often advocated to; compensate for shortages or reduce demand; reduce cost or improve efficiency.1 A number of countries use dental auxiliaries who are permitted to work in patients' mouths and there is a wide variation in their training and permitted duties. This review uses the term ‘operating dental auxiliaries which includes dental therapists, dental hygienists, extended-duty dental nurses, oral health therapists, orthodontic auxiliaries, clinical dental technicians, maxillofacial technicians and denturists. The aim of this review was to assess the effectiveness, costs and cost-effectiveness of dental auxiliaries in providing care traditionally provided by dentists.
This review was undertaken using the methodological approaches of the Cochrane Effective Practice and Organisation of Care (EPOC). This Cochrane Group has a focus on interventions designed to improve the delivery, practice and organisation of health care services. Because of the topic areas that they cover this group utilises a broader range of study designs in their reviews and this can been seen by the consideration of non-randomised controlled trials (NRCTs), controlled before and after studies (CBAs) and interrupted time series (ITSs) to address the review's question. However despite a wide search of a large number of databases no NRCTs, CBAs or ITSs study designs met the review's inclusion criteria.
Only five studies were included in the review; all were considered to be at high risk of bias, and the majority of those were more than 20 years old. The quality of the available evidence was considered to be very low, as it was in the 2012 review by Wright et al.2 and the 2002 review by Galloway et al.3 One of the main recommendations of the Galloway review was that more high-quality studies be undertaken into the effectiveness and cost-effectiveness of dental auxiliaries, and it is disappointing that this new review of the topic could find little or no new research since that review had been published. Here in the UK where there has been an expansion of both the numbers of operating dental auxiliaries being trained and the range of treatments they are able to provide, this lack of available evidence to help ensure their most effective use is likely to have a negative effect on the development of effective dental teams.
Corrections and clarifications
This article was originally published in the Sept 2014 issue of EBD. Owing to a problem in the production process an incorrect commentary section was paired with the abstract of the paper. The Editor would like to thank a number of readers who highlighted this error. The corrected article is reprinted here in full.
References
Sibbald B, McBride A, Birch S . Labour substitution and efficiency in health care delivery: general principles and key messages. Centre for Workforce intelligence. London 2011. (Downloaded from http://www.cfwi.org.uk/publications/labour-substitution-and-efficiency-in-healthcare-delivery-general-principles-and-key-messages)
Wright JT, Graham F, Hayes C et al. A systematic review of oral health outcomes produced by dental teams incorporating midlevel providers. J Am Dent Assoc 2013; 144: 75–91.
Galloway J, Gorham J, Lambert M, et al. The Professionals' Complementary to Dentistry: A Systematic Review and Synthesis. London: University College London, Eastman Dental Hospital, Dental Team Studies Unit, 2002.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Tom A Dyer, School of Clinical Dentistry, University of Sheffield, Claremont Crescent, Sheffield, S10 2TA, UK. E-mail: t.dyer@sheffield.ac.uk
Dyer TA, Brocklehurst P, Glenny AM, Davies L, Tickle M, Issac A, Robinson PG. Dental auxiliaries for dental care traditionally provided by dentists. Cochrane Database Syst Rev 2014; 8: Art. No. CD010076. DOI: 10.1002/14651858.CD010076. pub2.
This paper is based on a Cochrane Review published in the Cochrane Library 2014, issue 8 (see www.thecochranelibrary.com for information). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the Cochrane Library should be consulted for the most recent version of the review.
Rights and permissions
About this article
Cite this article
Richards, D. Lack of high-quality studies comparing the effectiveness, and cost-effectiveness, of dental auxiliaries and dentists in performing dental care. Evid Based Dent 16, 2–3 (2015). https://doi.org/10.1038/sj.ebd.6401070
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401070