Abstract
Cerebral blood flow pressure-passivity results when pressure autoregulation is impaired, or overwhelmed, and is thought to underlie cerebrovascular injury in the premature infant. Earlier bedside observations suggested that transient periods of cerebral pressure-passivity occurred in premature infants. However, these transient events cannot be detected reliably by intermittent static measurements of pressure autoregulation. We therefore used continuous bedside recordings of mean arterial pressure (MAP; from an indwelling arterial catheter) and cerebral perfusion [using the near-infrared spectroscopy (NIRS) Hb difference (HbD) signal) to detect cerebral pressure-passivity in the first 5 d after birth in infants with birth weight <1500 g. Because the Hb difference (HbD) signal [HbD = oxyhemoglobin (HbO2) − Hb] correlates with cerebral blood flow (CBF), we used coherence between MAP and HbD to define pressure-passivity. We measured the prevalence of pressure-passivity using a pressure-passive index (PPI), defined as the percentage of 10-min epochs with significant low-frequency coherence between the MAP and HbD signals. Pressure-passivity occurred in 87 of 90 premature infants, with a mean PPI of 20.3%. Cerebral pressure-passivity was significantly associated with low gestational age and birth weight, systemic hypotension, and maternal hemodynamic factors, but not with markers of maternal infection. Future studies using consistent serial brain imaging are needed to define the relationship between PPI and cerebrovascular injury in the sick premature infant.
Similar content being viewed by others
Main
Cerebral pressure autoregulation maintains CBF relatively constant despite changes over a range of systemic blood pressures known as the autoregulatory plateau (1). Conversely, when changes in blood pressure result in concordant changes in CBF, the cerebral circulation is deemed “pressure passive.” Current understanding is that cerebral pressure-passivity develops when changes in blood pressure exceed the capacity of the intact cerebral autoregulatory system or when the system is impaired by illness, injury, or vasoactive medications. Cerebral pressure-passivity is considered a risk factor for cerebrovascular injury in the sick premature infant (2–4). The current study extends our earlier work (3) using bedside NIRS to measure continuously cerebrovascular responses to spontaneous fluctuations in blood pressure. In our previous studies, we observed that cerebral pressure-passivity may wax and wane over relatively short periods in premature infants. To study the fluctuating nature of cerebral pressure-passivity and quantify its prevalence over time, we developed a continuous recording and analysis system because previously described techniques using intermittent static measurements (5–7) would be unable to measure the prevalence of fluctuating cerebral pressure-passivity over the highest risk for brain injury in premature infants. The principal aim of this technique is to make quantitative measurements of the prevalence of cerebral pressure-passivity rather than to test the integrity of cerebral pressure autoregulation and its limits.
Our hypotheses were that a pressure-passive state would be common but fluctuating in a population of critically ill premature infants, and that its incidence would be related to gestational age (GA) and to specific perinatal clinical risk factors known to affect systemic and cerebral hemodynamics (1,6).
METHODS
Subjects.
In this prospective study, we enrolled very low birth weight (VLBW) infants with birth weight <1500 g and postnatal age <12 h. Subjects were required to have a clinically indicated indwelling arterial catheter for continuous online measurement of blood pressure. We excluded infants in whom early cranial ultrasound (US) showed preexisting major brain injury or malformations and infants with genetic syndromes. We obtained written informed consent in all cases. The study was approved by the institutional review boards at both participating hospitals, Children's Hospital Boston and Brigham and Women's Hospital.
Clinical data.
We obtained maternal health, pregnancy, and labor and delivery data from the mother's medical record. Specifically, we recorded the diagnoses of pregnancy-induced hypertension, preterm labor, intrapartum hemorrhage, and chorioamnionitis made by the treating obstetrician. Fetal heart rate recordings were classified as abnormal if from the clinicians' report there were early or late decelerations, abnormal variability, or intermittent or sustained tachycardia or bradycardia. We recorded findings from the placental pathology report, including infarctions and chorioamnionitis.
We obtained detailed data from the infant's medical record (i.e. all serum blood gas, electrolyte, and hematological data), particularly over the first five postnatal days of life when the hemodynamic and NIRS measurements were made. We recorded the birth weight and GA (determined by dates and/or ultrasonography) and collected data regarding the type and duration of respiratory support, all major illnesses, suspected or culture-positive bacterial infections, surgical procedures, cranial US results, and all medications administered. Available cranial US studies performed for clinical indications during the first 5 d (i.e. the hemodynamic study period) were interpreted by two investigators (D.N.D. and A.J.du P.) blinded to the clinical and study data.
Continuous NIRS and blood pressure recording.
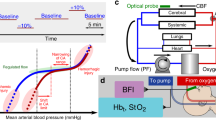
NIRS data were recorded continuously using a NIRO-500 spectrophotometer (Hamamatsu Photonics, Hamamatsu City, Japan); a technician at the bedside monitored the recording and events that could affect the NIRS signals. The recorded NIRS signals were changes in cerebral HbO2 and Hb concentration, as described in detail previously (8). Simultaneously and time-locked to these NIRS data, we recorded MAP from the arterial line and Hb saturation (SaO2) from pulse oximetry (Masimo, Irvine, CA) (Fig. 1). All signals were collected simultaneously in real time at a sampling rate of 2 Hz, converted to a digital format, and stored in a laptop computer. We used software (Onmain, Hamamatsu Photonics, Hamamatsu City, Japan) to display and save all the signal data. NIRS and systemic hemodynamic data were recorded continuously for up to 12 h per day for the first 5 d after birth. These recordings were terminated before 5 d if the indwelling arterial catheter (i.e. continuous MAP recording) was discontinued by the treating neonatologist.
Hemodynamic data processing and analysis.
We first removed all artifacts from the hemodynamic data, such as brief periods when the MAP signal was unavailable (e.g. during withdrawal of blood specimens through the catheter). In addition, because changes in the saturation of circulating Hb may directly affect the HbD signal, we rejected from the analysis periods of data in which there was concordance between the HbD and systemic SaO2 signals. We then used an automated program written in MatLab (The Mathworks Inc., Natick, MA) specifically to identify and remove occasional artifacts due to optode movement or light contamination. Data were interpolated if the artifact lasted three or fewer samples (i.e. ≤1.5 s), or excluded from analysis if the artifact lasted more than three samples. The data were then automatically divided into epoch lengths of 10 continuous minutes each.
The HbD signal was calculated as the difference between HbO2 and Hb for each data point. We previously validated changes in HbD to be highly correlated with changes in CBF (9). We used transfer function analysis to determine the coherence between the MAP and HbD signals (10,11) in the frequency range of 0–0.04 Hz. The coherence measures the degree of concordance between the changes in the two signals at specific frequencies for each 10-min epoch. If the MAP and HbD signals are varying together with high coherence, this would indicate a pressure-passive state because CBF (HbD) is changing in concert with blood pressure (e.g. Fig. 1A). If the MAP and HbD signals vary at different frequencies, then these signals are not coherent and cerebral pressure-passivity is absent (e.g. Fig. 1B). We determined the threshold coherence to be 0.77, using a published mathematical definition of threshold coherence (11). This coherence threshold was calculated from the sampling rate (down-sampled from 2 to 0.4 Hz), the fast Fourier transform length (120 samples = 300 s), and the signal length (600 s, i.e., 10 min), as described previously (11). Hence, if the mean coherence for an epoch was ≥0.77 within the 0- to 0.04-Hz frequency band, the epoch would be classified as pressure-passive. Finally, we defined the PPI as the percentage of 10-min epochs that were classified as coherent. For each infant, we calculated the PPI for each day and calculated an overall PPI for all days recorded.
In addition, we analyzed the blood pressure data with regard to hypotension and variability. First, we calculated the mean MAP over each 10-min epoch, and using published normative data (12), we designated epochs as hypotensive if the MAP during those 10 min was <10th percentile for birth GA and postnatal age. Next, we determined the hypotensive index (HOI) as the percentage of 10-min epochs classified as hypotensive, and we calculated both daily and overall HOI for each infant. Finally, we measured the MAP variability by determining the coefficient of variation of MAP for each 10-min epoch.
Statistical Analysis.
We analyzed the relationship between PPI, HOI, and other continuous variables using regression analysis. When comparing mean PPI or HOI with binary variables (e.g. gender), we used a t test and used log-transformations of the PPI and HOI data when the data were not normally distributed. For categorical variables that were not binary, analysis of variance was used with log-transformations of the data when necessary. For outcome measures that were measured daily over time, repeated-measures regression was used. After finding strong correlations between both PPI and HOI and birth GA and weight, we controlled for both of these variables in all subsequent analyses in which statistically significant results were found. When extreme outliers were found in the data, analyses were also repeated without these outliers to determine whether the outliers accounted for the statistically significant relationships between variables.
RESULTS
We made cerebral and systemic hemodynamic measurements in 90 VLBW infants during the first five postnatal days of life. The clinical characteristics of these infants and their mothers are shown in Tables 1 and 2. Based on their postnatal day of life, we obtained HbD and MAP data from 88 infants on d 1 (two infants not studied on d 1 were studied on later days), 81 infants on d 2, 62 on d 3, 53 on d 4, and 38 on d 5. There was a decrease in the number of infants studied over the first 5 d of life due to removal of the arterial catheter by clinicians or to early demise (four infants).
Hemodynamic indices.
Tables 3 and 4 shows the mean PPI and HOI indices for each day and for the overall 5 d combined. Notably, 87 of 90 infants showed pressure-passive epochs during their entire monitoring period, with an overall mean (±SD) number of pressure-passive epochs for the group of 22.1 (±15.3), with a range of 0–65. After removal of artifacts from the hemodynamic data, each infant had a mean of 103 (±46) epochs for analysis. Hence, by our definition of PPI, we found a mean PPI of 20.3% (±9.6) in the population overall for all days studied (Table 3). However, the range of PPI values was quite wide (0–48.6% for overall PPI). In fact, daily PPI values exceeded 40% in 17 infants with birth GA <29 wk on d 3–5 (up to maximum PPI of 81.8%). Examples of NIRS and MAP recordings from infants with and without pressure-passive data are shown in Fig. 1. Notably, there is no period of systemic hypoxemia (measured by SaO2) despite changes in both MAP and HbD signals.
Similarly, we found a significant incidence of hypotension as measured by the HOI. In the overall population, we found a mean HOI of 5.8% (±9.9) for all days recorded, with a range of up to 41.2% for overall mean HOI (Table 4). Moreover, we found that 14 infants had daily HOI values of >40% to a maximum HOI of 100% (Table 4).
GA and birth weight.
We found a strong association between PPI and both GA and weight at birth (Tables 3 and 4). Specifically, lower GA at birth (p = 0.018) and lower birth weight (p = 0.038) both correlated significantly with a higher overall PPI. Likewise, GA and weight at birth showed a strong inverse correlation with hypotension, as defined by overall HOI (p < 0.01 for both). Because of this significant effect of GA and birth weight, we controlled for both variables in all subsequent analyses below.
Postnatal age.
When evaluating the effect of postnatal age, we found an unexpected increase in both mean PPI and HOI over d 1–5 (Tables 3 and 4 and Fig. 2). To determine whether the increase in PPI and HOI was due to the dropout of healthier infants in whom arterial catheters were discontinued earlier, we analyzed the subset of infants (n = 34) with five full days of hemodynamic data. For this subset, we found no statistically significant increase in PPI over d 1–5; hence, the apparent increase in PPI in the whole group was likely related to sampling bias. However, we did find a statistically significant increase in the HOI for d 1–5 (p < 0.0001). We then analyzed this subset to determine whether the increase in HOI over d 1–5 was due to discontinuation of vasopressor medications before day 5. We compared infants who did and did not receive vasopressor medications on each day and found no significant difference in the mean daily HOI (Table 5). We then compared the average daily HOI between infants in whom vasopressors were either continued, discontinued, started, or never used and found that HOI rose with increasing postnatal age in all four cases (Table 6). In fact, infants who required vasopressors to be started or continued had a higher mean HOI than those in whom vasopressors were discontinued or never used.
Blood pressure.
We then examined the relationship between PPI and HOI to determine whether a pressure-passive state was more frequent in infants with hypotension and whether infants were more likely to have cerebral pressure-passivity during periods of hypotension. We found a highly significant correlation between the overall PPI and overall HOI for the entire group (r = 0.46, p < 0.0001). When we compared epochs with or without hypotension, we found that 31.7% of hypotensive epochs (n = 656) were pressure passive compared with 20.7% of nonhypotensive epochs (n = 8590, p < 0.0001 by χ2 test). We also examined the relationship between PPI and the variability of MAP to determine whether PPI was higher in infants with greater variation in their blood pressure. We found the correlation between MAP variability and PPI by individual epoch was quite low (r = 0.14, p < 0.001). Moreover, we found that mean coefficient of variation of MAP for pressure-passive epochs was 0.058 (n = 1988) compared with 0.047 for nonpressure-passive epochs (n = 7258, p < 0.0001).
Maternal/pregnancy factors.
We found no association between either PPI or HOI and indicators of maternal infection, including maternal chorioamnionitis (clinical or pathologic diagnosis), duration of ruptured membranes, or maternal fever.
When examining maternal hemodynamic factors, we found a higher overall PPI for infants with a maternal history of pregnancy-induced hypertension (PPI = 24.2) versus those without (PPI = 19.9, p < 0.05), but no difference in HOI. We also found a significantly higher PPI in cases with hemorrhage during labor and delivery (PPI = 26.7) versus those without (PPI = 19.1, p < 0.03). Finally, PPI was significantly higher in infants with placental infarction by pathologic examination (PPI = 28.0) versus those without (PPI = 19.0; p = 0.013).
We found no significant relationship between PPI or HOI and maternal age, race, administration of antenatal steroids, the presence or duration of labor, spontaneous rupture of membranes, cesarean section, fetal presentation, fetal heart rate abnormalities, or infants who were singletons versus those from multiple gestation pregnancies.
Neonatal clinical factors.
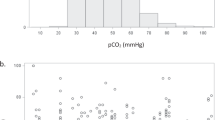
We evaluated the impact of early neonatal (first 6 h after birth) factors on PPI and HOI, again controlling for GA and birth weight. We found no significant relationship between either PPI or HOI and gender, Apgar score at 5 min, minimum pH or minimum or maximum Po2 or Pco2.
When examining the impact of neonatal clinical factors between 6 h and 5 d after birth, we found a strong relationship between indicators of significant cardiorespiratory illness and HOI but not PPI. Specifically, there was an association between the use of any vasopressors/inotropes (dopamine, dobutamine, epinephrine) or hydrocortisone (p < 0.004), sedative medications (p < 0.0001), or paralytic medications (p < 0.032) and the overall HOI but not PPI. When comparing infants who received high-frequency oscillatory ventilation (HFOV) versus intermittent mandatory ventilation (IMV) versus continuous positive airway pressure (CPAP), we found significantly higher HOI values for those with a higher level of ventilatory support (HFOV > IMV > CPAP, p < 0.0001), but no relationship to PPI. Infants diagnosed with a patent DA (n = 48) had a statistically higher overall HOI than those without (n = 42), but the difference was not large (HOI of 7.8% versus 3.5%, p = 0.001). Bacterial infection was strongly associated with a higher HOI (p = 0.0002) but not with PPI. Other clinical variables that were not related to the daily mean PPI or HOI included the daily maximum or minimum recorded values of pH, Pco2, Po2, HCO3, hematocrit, serum electrolytes, or glucose concentration. As shown in Table 3, the incidence of germinal matrix-intraventricular hemorrhage (GM-IVH) in our population (39%) was high and likely reflects the illness severity of our population, as suggested by the high level of cardiorespiratory support needed. However, there was no significant correlation between the PPI and HOI values and GM-IVH on the clinical US studies.
DISCUSSION
The principal finding of this study is that a pressure-passive cerebral circulation is frequent in sick premature infants in the first days after birth. Second, we found that cerebral pressure-passivity is not an all-or-none phenomenon, but rather fluctuates over time. In our VLBW study population, cerebral perfusion was pressure passive for a mean 20% of the time, and in certain extremely premature infants, this state exceeded 50% of epochs recorded. This study demonstrates the feasibility of our novel continuous monitoring technique for detecting frequent but often transient periods of cerebral pressure-passivity in sick premature infants.
Our finding of frequent but transient cerebral pressure-passivity exhibits a fundamental difference from previous studies of cerebral pressure autoregulation (CPA) in preterm infants. By providing prolonged and continuous measurements of cerebral perfusion in response to spontaneously occurring blood pressure changes, our technique provides insights into the fluctuating nature of cerebral pressure-passivity, which is not accessible with other techniques that use isolated intermittent measures of CPA. Static and/or intermittent measurements of CPA used in previous studies (2,7,13) are likely to miss transient cerebral pressure-passivity. Unlike earlier reports suggesting that pressure autoregulation is impaired in only some infants (3,13,14), we found that cerebral pressure-passivity may develop at some time in nearly all sick VLBW infants. By demonstrating that cerebral pressure-passivity fluctuates, our study also emphasizes the need for continuous monitoring if the role of pressure-passivity in cerebral injury is to be further elucidated.
The inverse relationship noted in our population between both GA and birth weight and a pressure-passive cerebral circulation is likely due to immaturity of the cerebral vasculature and vasoregulatory mechanisms (15). Because the risk of brain injury in premature infants is known to be inversely related to GA (16,17), our finding of increasing cerebral pressure-passivity with decreasing GA and birth weight is consistent with the notion that cerebral pressure-passivity plays a role in these brain injuries.
Previous reports have suggested a possible association between infection/inflammation, hypotension, and impaired cerebral vasoregulation (18,19). However, we found no association between indicators of maternal or placental infection and either cerebral pressure-passivity or hypotension. Our data suggest that the putative contribution of maternal infection to white matter injury is not mediated through vasoregulatory disturbances in early postnatal life. This question warrants further study.
Surprisingly, we found no association between acid-base status, oxygen or carbon dioxide levels, and cerebral pressure-passivity, given the known cerebral vasoreactive effects of blood gases, particularly carbon dioxide (10,20,21). However, this lack of association is likely related to the fact that blood gases were measured intermittently as opposed to our continuous and prolonged hemodynamic measurements. Given the fluctuating nature of cerebral pressure-passivity demonstrated in our study, the contribution of changing blood gases to these periods of cerebral pressure-passivity will demand more frequent or continuous blood gas measurements.
Using our hypotensive index based on previously described criteria for hypotension (12), we found an overall mean prevalence of systemic hypotension of 5.8% in our population. However, hypotension was much more common in extremely low birth weight infants, with the hypotensive index exceeding 80% in some infants on d 3–5. As with cerebral pressure-passivity, we found a significant inverse relationship between systemic hypotension and both GA and birth weight. Furthermore, we found a strong correlation between PPI and HOI, suggesting an increased risk of cerebral ischemia when systemic hypotension is combined with a pressure-passive cerebral circulation. However, we found that hypotension at any particular time was not invariably associated with a pressure-passive state (or vice versa). In this respect our findings are similar to previous work that suggested that cerebral pressure-passivity may be present despite normal blood pressure (2). One possible explanation for this finding is that the autoregulatory plateau is not fixed, but rather shifts in response to vasoactive stimuli other than blood pressure. This fluctuating relationship between blood pressure and cerebral pressure-passivity cautions against the reliance on fixed blood pressure guidelines for the preservation of cerebral pressure autoregulation and emphasizes the need for continuous monitoring of the cerebral circulation to detect disturbances in cerebral perfusion.
When we examined the effect of postnatal age on hemodynamics, we found an unexpected increase in HOI over the first five days of life. This finding seems counterintuitive given the expected maturation of physiologic systems with postnatal age. We considered several possible explanations for this finding. First, a patent DA in some infants was unlikely to be a major contributor to the observed increase in HOI since there was only a small difference in HOI values between those with or without a patent DA. Second, our analysis of the subset of infants with recordings over all 5 d showed that the increase in HOI with postnatal age remained statistically significant and hence was not due only to the dropout of healthier infants whose catheters were removed before d 5. Third, it is possible that clinicians at our center do not base their management of hypotension on the expected increase in normal blood pressure with postnatal age, even though previous studies (12,22) have shown that blood pressure increases over the first days after birth. However, we found that the mean HOI increased with postnatal age regardless of whether vasopressors were continued, discontinued, initiated later, or never used. Moreover, HOI was higher in infants receiving vasopressors for hypotension than in those not receiving vasopressors. Thus, the true increase in hypotension with advancing postnatal age noted in our study could not be attributed to the clinicians' interventions alone. Possibly hypotension in these infants was refractory to vasopressors or clinical target levels for blood pressure were lower than those used for our definition of hypotension (12).
There are several potential limitations of our technique. First, we used the NIRS HbD signal as a surrogate for CBF. This was based on the strong correlation between HbD and CBF in previous animal validation studies (9,23). It may be argued that in some instances, a change in HbD could reflect a change in oxygen extraction fraction. However, in premature newborns, cerebral oxygen extraction fraction is inversely related to cerebral oxygen delivery (24) and hence to cerebral perfusion (25). Therefore, by our technique, a decrease in CBF associated with a decrease in MAP that results in increased oxygen extraction will cause a decrease in HbD, thereby accurately identifying cerebral pressure-passivity. An additional concern is the fact that changes in circulating oxygenation may change the HbD signal independent of changes in perfusion. For this reason, we removed from the analysis all periods with concordant changes in HbD and SaO2.
The apparent lack of relationship between cerebral pressure-passivity and GM-IVH by cranial US may be perceived as a limitation of our technique. However, the principal aim of this study was to describe the prevalence of cerebral pressure-passivity in sick preterm infants using our novel technique. Given the relative insensitivity of cranial US to hypoxic-ischemic brain injury, we analyzed the US studies only for GM-IVH. The lack of association between both PPI and HOI and GM-IVH must be interpreted with extreme caution because the temporal relationship between hemodynamic measures and the cranial US studies was very inconsistent. Furthermore, 20% of infants already showed evidence of GM-IVH on their first US studies. Consequently, it was impossible in our study to establish whether hemodynamic patterns precede or follow GM-IVH. To study the temporal relationship between fluctuating hemodynamics and brain lesions, US studies will need to be performed on a frequent and consistent basis.
We confined our investigation of cerebral autoregulation to measurement of coherence only in the very low frequency band (0–0.04 Hz), which could theoretically limit detection of impairments in CPA at higher frequencies. We intentionally selected this frequency band because the impulse-response time for cerebral vasoreactivity to blood pressure changes is approximately 5–15 s in adults (10) and 12–50 s in newborns (26,27). Furthermore, our previous study (3) suggested that high coherence was found in VLBW infants predominantly at very low frequencies (0–0.01 Hz). Hence, we investigated autoregulation at these very low frequencies where biologic relevance had previously been demonstrated.
Another potential limitation of our approach is that spontaneous fluctuations in blood pressure are required to test the integrity of pressure autoregulation. Indeed, we found that PPI was positively correlated with variability in MAP, suggesting that a pressure-passive state was more likely to be detected when there was greater variation in MAP. However, the correlation was low, and there was not a great difference in MAP variability between epochs that were or were not pressure-passive. Hence, we were able to detect pressure-passivity during epochs with low MAP variability.
In summary, we have shown that our technique of continuous cerebrovascular monitoring is capable of identifying periods of cerebral pressure-passivity in the first days after birth. Our main findings were the high prevalence of a pressure-passive cerebral circulation in critically ill preterm newborns and a strong correlation of both a pressure-passive state and hypotension with lower GA and birth weight. Although the prevalence of cerebral pressure-passivity and hypotension was highest in certain infants, there was no consistent relationship between blood pressure and cerebral pressure-passivity. Given the fluctuating relationship between blood pressure and cerebral pressure-passivity described in this report, prevention of cerebral pressure-passivity in sick preterm infants may not be ensured by simply maintaining currently used blood pressure targets. Rather our data suggest that management aimed at preventing cerebral pressure-passivity in at-risk preterm infants should be guided by continuous monitoring of systemic-cerebral hemodynamic interactions.
Abbreviations
- CBF:
-
cerebral blood flow
- CPA:
-
cerebral pressure autoregulation
- GM-IVH:
-
germinal matrix–intraventricular hemorrhage
- HbD:
-
hemoglobin difference
- HOI:
-
hypotensive index
- MAP:
-
mean arterial blood pressure
- NIRS:
-
near-infrared spectroscopy
- PPI:
-
pressure-passive index
- SaO2:
-
oxyhemoglobin saturation
- US:
-
ultrasound
- VLBW:
-
very low birth weight
References
Greisen G 1997 Cerebral blood flow and energy metabolism in the newborn. Clin Perinatol 24: 531–546
Lou HC, Lassen N, Friis-Hansen B 1979 Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr 94: 118–121
Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, Volpe JJ 2000 Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106: 625–632
Volpe JJ 2001 Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res 50: 553–562
Younkin DP, Reivich M, Jaggi JL, Obrist WD, Delivoria-Papadopoulos M 1987 The effect of hematocrit and systolic blood pressure on cerebral blood flow in newborn infants. J Cereb Blood Flow Metab 7: 295–299
Pryds O, Greisen G 1989 Effect of PaCO2 and haemoglobin concentration on day to day variation of CBF in preterm neonates. Acta Paediatr Scand Suppl 360: 33–36
Tyszczuk L, Meek J, Elwell C, Wyatt JS 1998 Cerebral blood flow is independent of mean arterial blood pressure in preterm infants undergoing intensive care. Pediatrics 102: 337–341
Soul JS, du Plessis AJ 1999 New technologies in pediatric neurology. Near-infrared spectroscopy. Semin Pediatr Neurol 6: 101–110
Soul JS, Taylor GA, Wypij D, du Plessis AJ, Volpe JJ 2000 Noninvasive detection of changes in cerebral blood flow by near-infrared spectroscopy in a piglet model of hydrocephalus. Pediatr Res 48: 445–449
Zhang R, Zuckerman JH, Giller CA, Levine BD 1998 Transfer function analysis of dynamic cerebral autoregulation in humans. Am J Physiol 274: H233–H241
Taylor JA, Carr DL, Myers CW, Eckberg DL 1998 Mechanisms underlying very-low-frequency RR-interval oscillations in humans. Circulation 98: 547–555
Watkins AM, West CR, Cooke RW 1989 Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 19: 103–110
Boylan GB, Young K, Panerai RB, Rennie JM, Evans DH 2000 Dynamic cerebral autoregulation in sick newborn infants. Pediatr Res 48: 12–17
Pryds O, Greisen G, Lou H, Friis-Hansen B 1989 Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 115: 638–645
Kuban KC, Gilles FH 1985 Human telencephalic angiogenesis. Ann Neurol 17: 539–548
Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR 2005 The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed 90: F134–F140
Greisen G, Borch K 2001 White matter injury in the preterm neonate: the role of perfusion. Dev Neurosci 23: 209–212
Yanowitz TD, Jordan JA, Gilmour CH, Towbin R, Bowen A, Roberts JM, Brozanski BS 2002 Hemodynamic disturbances in premature infants born after chorioamnionitis: association with cord blood cytokine concentrations. Pediatr Res 51: 310–316
Yanowitz TD, Baker RW, Roberts JM, Brozanski BS 2004 Low blood pressure among very-low-birth-weight infants with fetal vessel inflammation. J Perinatol 24: 299–304
Panerai RB, Kelsall AW, Rennie JM, Evans DH 1996 Analysis of cerebral blood flow autoregulation in neonates. IEEE Trans Biomed Eng 43: 779–788
Verma PK, Panerai RB, Rennie JM, Evans DH 2000 Grading of cerebral autoregulation in preterm and term neonates. Pediatr Neurol 23: 236–242
Nuntnarumit P, Yang W, Bada-Ellzey HS 1999 Blood pressure measurements in the newborn. Clin Perinatol 26: 981–996
Pryds A, Tonnesen J, Pryds O, Knudsen GM, Greisen G 2005 Cerebral pressure autoregulation and vasoreactivity in the newborn rat. Pediatr Res 57: 294–298
Kissack CM, Garr R, Wardle SP, Weindling AM 2005 Cerebral fractional oxygen extraction is inversely correlated with oxygen delivery in the sick, newborn, preterm infant. J Cereb Blood Flow Metab 25: 545–553
Derdeyn CP, Videen TO, Yundt KD, Fritsch SM, Carpenter DA, Grubb RL, Powers WJ 2002 Variability of cerebral blood volume and oxygen extraction: stages of cerebral haemodynamic impairment revisited. Brain 125: 595–607
Zernikow B, Michel E, Kohlmann G, Steck J, Schmitt RM, Jorch G 1994 Cerebral autoregulation of preterm neonates—a non-linear control system?. Arch Dis Child Fetal Neonatal Ed 70: F166–F173
Panerai RB, Rennie JM, Kelsall AW, Evans DH 1998 Frequency-domain analysis of cerebral autoregulation from spontaneous fluctuations in arterial blood pressure. Med Biol Eng Comput 36: 315–322
Author information
Authors and Affiliations
Additional information
The authors acknowledge the support of National Institutes of Health grant P01NS38475, the United Cerebral Palsy Foundation (J.S.S.), the LifeBridge Fund, and the Caroline Levine Foundation. This project was funded in part by grant MO1-RR02172 from the National Center for Research Resources, National Institutes of Health, to the Children's Hospital Boston General Clinical Research Center.
Rights and permissions
About this article
Cite this article
Soul, J., Hammer, P., Tsuji, M. et al. Fluctuating Pressure-Passivity Is Common in the Cerebral Circulation of Sick Premature Infants. Pediatr Res 61, 467–473 (2007). https://doi.org/10.1203/pdr.0b013e31803237f6
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/pdr.0b013e31803237f6
This article is cited by
-
Predicting severe intraventricular hemorrhage or early death using machine learning algorithms in VLBWI of the Korean Neonatal Network Database
Scientific Reports (2024)
-
Near-infrared spectroscopy monitoring of neonatal cerebrovascular reactivity: where are we now?
Pediatric Research (2023)
-
Neuromonitoring in neonatal critical care part II: extremely premature infants and critically ill neonates
Pediatric Research (2023)
-
Clinical determinants of cerebrovascular reactivity in very preterm infants during the transitional period
Pediatric Research (2022)
-
Assessing cerebral blood flow, oxygenation and cytochrome c oxidase stability in preterm infants during the first 3 days after birth
Scientific Reports (2022)