Abstract
Objective
To determine whether ventilator-related fluctuations in cerebral blood volume (CBV) are associated with cerebral pressure passivity.
Study design
In a prospective study of newborns undergoing positive-pressure ventilation, we calculated coherence between continuous mean arterial pressure (MAP) and cerebral near-infrared spectroscopy hemoglobin difference (HbD). Significant HbD–MAP coherence indicated cerebral pressure passivity. CBV changes were measured as the spectral power of total hemoglobin (SHbT) at the ventilator frequency. A regression model tested whether SHbT predicts cerebral pressure passivity and/or death/brain injury, controlling for birth gestational age and other factors.
Results
We studied 68 subjects with prematurity (n = 19), congenital heart disease (n = 11), and hypoxic–ischemic encephalopathy (n = 38). SHbT, sedative use, and pCO2 were positively associated, and circulating hemoglobin negatively associated, with cerebral pressure passivity (p < 0.001), which was positively associated with brain injury (p < 0.001).
Conclusion
In sick newborns, ventilator-related CBV fluctuations may predispose to cerebral pressure passivity, which may predispose to an adverse neonatal outcome.
Similar content being viewed by others
Introduction
Critically ill infants with impaired cerebral pressure autoregulation are at significant risk for brain injury [1,2,3,4]. Typically, cerebral pressure autoregulation maintains a relatively constant cerebral blood flow (CBF) over a range (the cerebral pressure autoregulation plateau) of cerebral perfusion pressures (CPP, the gradient between arterial blood pressure and cerebral venous pressure), thereby buffering variations in systemic arterial blood pressure [1, 3]. Normally, cerebral venous compliance is significantly greater than arterial compliance, and hence venous pressure is usually much lower than arterial pressure. Cerebral venous pressure is usually low and not easily measured, particularly in small sick infants. Therefore, its effect is often disregarded, and arterial blood pressure is used as the surrogate for CPP. When CPP is no longer on the cerebral pressure autoregulation plateau, the cerebral circulation becomes pressure passive, and changes in CPP result in parallel changes in CBF [3]. Particularly in conditions with high risk for systemic hypotension (e.g., critically ill newborn infants), elevation of cerebral venous pressure will decrease CPP and eventually abolish the cerebral pressure autoregulation. Positive-pressure ventilation is often required to support the critically ill newborn, and may cause significant fluctuations in intrathoracic, and hence, cerebral venous pressure and volume [5]. Of note, a piglet model showed a significant correlation between cerebral oxygen saturation and venous oxygen saturation measured from jugular bulb [6].
The integrity of cerebral pressure autoregulation may be measured using the concordance between CPP and CBF changes; as cerebral pressure autoregulation fails, CPP and CBF become more closely correlated [3]. Studies in high-risk newborns have shown that cerebral pressure autoregulation may wax and wane over the course of critical illness [3], making periodic point estimates of cerebral pressure autoregulation unreliable. In order to detect and respond to cerebral pressure passivity appropriately, continuous cerebral pressure autoregulation monitoring is needed. We have used the technique of near-infrared spectroscopy (NIRS) for continuous monitoring of cerebral perfusion at the bedside of sick newborns [3, 7]. We have previously validated continuous NIRS-derived hemodynamic signals in animal models as reliable surrogates for CBF to allow for the continuous, noninvasive derivation of cerebral pressure autoregulation [8]. For this study, our goals were to evaluate the association between cerebral venous volume changes at the ventilator frequency on the development of (1) cerebral pressure passivity, and (2) brain injury, in newborn infants undergoing intensive care. We hypothesized that higher ventilator-related changes in cerebral venous volume would predict periods of cerebral pressure passivity, and that higher venous volume changes would predict brain injury.
Materials and methods
Study population and data collection
In this retrospective study, we analyzed data collected from infants undergoing conventional positive-pressure mechanical ventilation in the neonatal and cardiac intensive care units of Children’s National Hospital. The study population included infants with three broad categories of illness, all known to be at significant risk of brain injury, namely, term/near-term infants with either perinatal hypoxic–ischemic encephalopathy (HIE) or congenital heart disease (CHD), as well as preterm infants (<37 weeks of gestational age (GA)). It is important to note that the purpose of our study was not to analyze the impact of disease conditions on the relationship between positive-pressure ventilation and brain injury. The HIE infants all met inclusion criteria for, and were treated with, induced hypothermia between 2011 and 2016 [9]. All CHD infants requiring surgery within the newborn period were studied, and they were recruited from years 2012 to 2014. Premature infants were recruited from years 2011 to 2015. We excluded from the study infants with obvious syndromic diagnoses or known cerebral malformations. All data were acquired in prospective studies approved by the Children’s National Institutional Review Board, and informed consent was obtained in all cases. Continuous recording of changes in cerebral oxygenated hemoglobin (Hb) and deoxygenated Hb was performed using NIRS (NIRO 200, Hamamatsu Photonics, Hamamatsu City, Japan). The cerebral NIRS data were measured from the frontotemporal regions over both cerebral hemispheres (as previously described) [7, 10]. The arterial blood pressure signal was collected from the analog port of the Philips MP70 bedside monitor (IntelliVue, Philips, MA, USA). Continuous recordings of NIRS and invasive arterial blood pressure were sampled at 1 kHz, time locked, and saved into files using custom software developed in Lab View (National Instruments, TX, USA). The clinical variables, including GA at birth, postnatal age, gender, partial pressure of carbon dioxide (pCO2), circulating Hb concentration, use of sedatives (phenobarbital, benzodiazepines, morphine, and fentanyl), use of vasopressor medications (dopamine and epinephrine) administered to the infant during our study period, and death during hospitalization, were retrieved from the medical record.
Cerebral hemodynamic studies
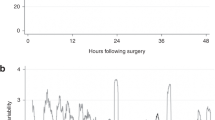
All analyses were performed offline using MATLAB (Mathworks Inc., Natick, MA, USA). To exclude possible direct confounding effects within the autoregulation frequency (0.05–0.25 Hz), we only included data from infants with a ventilator rate frequency greater than 0.25 Hz. For each cycle of the blood pressure, the peak systolic and trough diastolic pressures were identified. The mean arterial pressure (MAP) was calculated as the linear combination of one-third of systolic pressure and two-thirds of diastolic pressure. For further analysis, MAP was converted into a uniformly sampled signal using a cubic spline function with a sample rate of 5 Hz, and the NIRS signal was downsampled to 5 Hz. Next, we derived the cerebral hemoglobin difference (HbD) signal (HbD = oxygenated Hb − deoxygenated Hb) and the total cerebral Hb (HbT = oxygenated Hb + deoxygenated Hb) from the NIRS measurements. We used HbD and HbT as surrogates for CBF and cerebral blood volume (CBV), respectively, as previously described [8, 11]. The continuous MAP, HbD, and HbT signals were partitioned into 10-min nonoverlapping epochs, and the coherence between MAP and HbD (coherenceMAP–HbD) was calculated for each epoch [8, 11]. The coherence in a frequency band was considered statistically significant if it was above the mathematically defined threshold of 0.3842 [12]. The impulse response time for the MAP–HbD interaction during intact cerebral pressure autoregulation is between 5 and 20 s [13]. On this basis, we consider significant coherence between the MAP and HbD in the frequency band of 0.05–0.25 Hz to reflect cerebral pressure passivity. To study the effect of ventilator-related cerebral venous volume changes on cerebral pressure autoregulation, we categorized epochs as cerebral pressure passive (coherenceMAP–HbD > 0.3842) or cerebral autoregulating (coherenceMAP–HbD ≤ 0.3842). Next, we calculated the power spectral density HbT (SHbT) for changes at the ventilator frequency in every 10-min epoch to quantify venous volume fluctuations. We used the maximum power in the frequency band of 0.3–1 Hz, which is dominated by the ventilator oscillations, that is, there was a distinct peak at the ventilator frequency in the power spectrum of HbT.
Neuroimaging studies
Neonatal brain imaging was performed using cranial ultrasound (US) and/or brain magnetic resonance imaging (MRI). The US studies were performed on Philips CX50 (Philips HealthCare, Andover, MA, USA) or Voluson E8 (National Ultrasound, Duluth, GA, USA) devices, and MRI studies were performed on a 3T scanner (Discovery MR750, GE Healthcare, Waukesha, WI, USA), with standard sequences including 3D T1 SPGR, T2 FSE, T2* susceptibility, and DTI diffusion.
The timing and modality of imaging followed standardized clinical imaging protocols at our institution: premature infants (<28 weeks of GA) underwent cranial US studies at 3 and 7 days after birth, and a brain MRI at term-equivalent age if still in the NICU. In HIE survivors, MRI was performed at 3–5 days and again at 10–12 days of life. In the critical CHD group destined for neonatal cardiopulmonary bypass, MRI studies were performed prior to their cardiac surgery. All neuroimaging studies were reviewed by experienced pediatric neuroradiologists (GV and JM). Infants with brain malformations were excluded, and evidence of acquired hemorrhagic or hypoxic–ischemic lesions was documented. Cranial US studies were considered significantly abnormal if they had evidence of intraventricular hemorrhage grade III, periventricular hemorrhagic infarction, periventricular white matter injury (focal hyper- and/or hypoechoic lesions), or ventriculomegaly. MRI studies were reviewed to exclude infants with congenital malformations. When both US and MRI were available, the study showing the clearest injury pattern was used.
Statistical analysis
The statistical analysis was carried out using SAS 9.3 (SAS Institute Inc., NC, USA) with two-tail significance level α = 0.05. Continuous data were summarized as mean (standard deviation) or median (minimum and maximum). Categorical variables were summarized using counts and percentages. The SHbT values were compared between two cerebral hemispheres using a Student’s t test, and averaged if there were no significant differences. The clinical variables associated with pressure passivity or brain injury/death were identified using Fisher exact test or Wilcoxon test. The following clinical variables were included in the model: gender, sedation use, pressor support, midazolam (seizure medication) use, GA, pCO2, and circulating Hb. Using significantly associated clinical variables and SHbT, a random effect model was developed to predict pressure passivity. To predict brain injury, a logistic regression was built using the average of SHbT and pressure passivity, calculated from all 10-min epochs. Of note, we did not average the raw HbD–MAP coherence values; rather, we averaged the number of epochs that were pressure passive or autoregulating. In our earlier studies, we defined the pressure-passivity index as the percentage of study time the infant was pressure passive [13].
Results
We studied a total of 68 subjects (50% males). The average GA in the three categories, i.e., prematurity (n = 19), CHD (n = 11), and HIE (n = 38), was 24.7 (±0.9), 38.2 (±1.6), and 38.5 (±1.5) weeks, respectively. The median postnatal age was 0.84 (range: 0.25–50.51) days. The mean (standard deviation) birth weight of the infants was 2570 (1343) g. Thirty-eight infants (55.8%) were delivered by cesarean section. The median (minimum–maximum) MAP was 42 (26–60) mmHg. Other clinical and demographic features of the subjects are summarized in Table 1. The CHD cohort included infants with hypoplastic left heart syndrome (n = 2), transposition of greater arteries (n = 7), ventricular septal defect (n = 1), and Ebstein anomaly (n = 1). MRI was performed on 54 infants overall, 31 with HIE, 15 with prematurity, and 8 with CHD. Preterm infants (n = 15) who remained in the Children’s National NICU until term-equivalent age underwent MRI scanning. CHD infants (n = 8) underwent MRI prior to their corrective surgical procedure as per the institutional protocol.
Twenty-five infants had imaging evidence of brain injury, of which 21 were diagnosed by MRI (HIE, 16; CHD, 1; preterm infants, 4) and four by cranial US (CHD, 1; preterm infants, 3). Eight (all HIE infants) died in the intensive care unit. Across the entire population of critically ill infants, 53 (78%) experienced one or more periods of cerebral pressure passivity during their study periods.
Inotropic support was provided to 65.6% of infants and sedatives to 48% of infants. The mean (standard deviation) pCO2 value was 40.61 (12.31) mmHg. The mean (standard deviation) circulating Hb was 14.81 (3.13) g/dl.
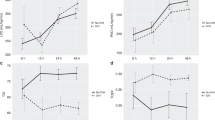
We obtained a total of 17,298 hemodynamic 10-min study epochs from 68 patients, of which 13,982 were autoregulating and 3316 were pressure passive. Of the 118.15 days of hemodynamic monitoring, 0.89 days were rejected for poor quality. No significant differences were observed between the cerebral hemispheres (p > 0.05); therefore, the results from the two hemispheres were averaged for analysis. The unadjusted SHbT values were significantly higher in pressure-passive epochs compared with autoregulation epochs (p < 0.001) (see Table 2). SHbT (p < 0.001), sedation (p < 0.001), and pCO2 (p < 0.001) were positively associated, and circulating Hb (p < 0.001) was negatively associated, with pressure passivity (see Table 3). While SHbT was associated with brain injury in unadjusted analysis, this relationship was no longer significant after adjusting for covariates. Logistic regression analysis showed that cerebral pressure passivity was independently associated with brain injury or death with a magnitude of 0.0430 and standard error of 0.0192 (p = 0.0248), whereas SHbT was not.
Discussion
In this study, we identified a significant relationship between the magnitude of fluctuations in CBV associated with positive-pressure ventilation, and the presence of cerebral pressure passivity, in a population of critically ill newborn infants. This association was present in infants of different GAs and different forms of critical illness, all previously identified as risk factors for neonatal brain injury [14,15,16,17,18].
Cerebral pressure passivity is an important upstream antecedent in the causal pathway leading to brain injury in critically ill infants [3, 18,19,20]. Thus, detection of cerebral pressure passivity can be regarded as an actionable biomarker that presents intensivists with a window of opportunity to prevent brain injury. We have previously shown that in critically ill infants, cerebral pressure passivity was waxed and waned, and could not be predicted by changes in arterial blood pressure alone, and that other factors, including medications and respiratory status, may also play a role [3, 18]. Our current findings suggest that fluctuations in cerebral venous volume, in the setting of positive-pressure ventilation, may be another such factor. As clinicians begin to formulate strategies for optimizing intrinsic cerebral pressure autoregulation, changes in the cerebral venous compartment will need to be considered, as these are currently not routinely monitored in sick newborn infants.
Animal studies have shown the emergence of cerebral pressure passivity during experimental induction of hypotension, presumably due to a decrease in the transcerebral blood pressure gradient [21,22,23]. In addition, both the frequency of cerebral pressure-passive episodes [1, 3, 22, 24,25,26] and the severity or “gain” of cerebral pressure passivity, as measured by the quantitative change in CBF per unit change in blood pressure, are higher in critically ill infants who develop brain injury than in intact survivors [7, 13]. In our previous studies [3, 13], changes in arterial blood pressure alone could not consistently explain the observed pressure passivity, suggesting that other factors, possibly including cerebral venous hemodynamics, might play an underrecognized role in disrupting cerebral pressure autoregulation.
The pCO2 related to pressure passivity is not surprising, given that changes in circulating CO2 are known to influence cerebrovascular responses. Specifically, hypercarbia causes vasodilation, decreasing cerebrovascular resistance, and increasing CBF, whereas hypocapnia has the opposite effects [27, 28]. Thus, an increased pCO2 may compromise pressure vasoreactivity and, in turn, cerebral pressure autoregulation. Likewise, use of sedatives has been shown to impair cerebral pressure autoregulation, which is corroborated by our data [29]. Although there was a negative association between circulating Hb concentration and cerebral pressure passivity, the magnitude of association was not clinically relevant.
Cardiorespiratory failure is common among critically ill newborn infants, often necessitating ventilatory and hemodynamic support. Positive-pressure ventilation is associated with fluctuating increases in intrathoracic pressure, and decreased venous return, with increasing cerebral venous pressure and volume. In sick newborns, particularly those at risk for arterial hypotension, clinical consideration of cerebral venous pressures may be an important, but underappreciated, factor in the delivery of brain-oriented critical care.
The fluctuating venous volumes in our study were not an independent predictor of brain injury, but did predict cerebral pressure passivity, which, in turn, predicted brain injury. This relationship remained significant after adjusting for covariates in our study. One explanation could be that we used averaged SHbT values from each subject as a predictor in the logistic regression model, thereby leaving these analyses underpowered. Our results suggest that cerebral venous fluctuations may not have been a dominant predictor of brain injury, but rather one factor in the causal pathway. Future studies are needed to resolve this question.
Our study has several strengths, such as the prolonged duration of hemodynamic monitoring, the use of advanced signal- processing techniques to quantify ventilator-related changes imprinted on hemodynamic signals, and an inclusion of a heterogeneous population vulnerable to brain injury. The central hypothesis of our study was that in infants receiving positive-pressure ventilation, cerebral venous volume changes would be associated with cerebral pressure-flow passivity, presumably because of a decrease in the transcerebral pressure gradient. We also predicted that this association would be present regardless of the underlying critical illness and GA. This high-risk condition is likely to go underdetected with current forms of bedside monitoring. Larger studies are needed to corroborate our findings, and to explore the potential role of other clinical factors, including maturational status.
This study also has important limitations. While the inclusion of infants with different high-risk conditions makes the population heterogenous, it might bring in confounding variables, such as disease condition and GA at birth. In our study, GA at birth was not significantly associated with the relationship between cerebral venous volume changes and pressure passivity. In addition, we assumed (as have others) [5] that cerebral HbT changes occurring at the positive-pressure ventilatory frequency were occurring on the venous side of the cerebral circulation alone. While entirely plausible based on current understanding, this fact cannot currently be confirmed. Within subjects, fluctuations in the spectral power of HbT were noted during constant ventilator settings, suggesting that other as yet unknown factors may be playing a role in these complex hemodynamics. For example, in preterm infants born at less than 32 weeks of GA, cerebral oxygen saturation increases during the first 72 h of life, at a rate of 1% per GA week at birth [30]. Identifying such factors was beyond the scope of this study and should be pursued in future studies. Another limitation includes the methods used to diagnose brain injury; in this retrospective study, the timing of neuroimaging and its relationship with the hemodynamic studies differed across the three diagnostic groups. In addition, a minority of infants underwent US only. For these reasons, the potential causal relationship between the hemodynamic and neuroimaging findings cannot be resolved by the current data, and will require prospective evaluation.
Conclusion
In conclusion, our findings suggest that changes in cerebral venous volume in critically ill newborn infants, particularly those at risk for hypotension, may be an underappreciated factor in the development of cerebral pressure passivity in this vulnerable population. Furthermore, we show that such cerebral venous volume changes are readily detectable by NIRS, a monitoring device now widely available in most major centers. The importance of these findings and their application in brain-oriented neonatal care will require larger prospective studies.
References
Bassan H, Gauvreau K, Newburger JW, Tsuji M, Limperopoulos C, Soul JS, et al. Identification of pressure passive cerebral perfusion and its mediators after infant cardiac surgery. Pediatr Res. 2005;57:35–41.
Boylan GB, Young K, Panerai RB, Rennie JM, Evans DH. Dynamic cerebral autoregulation in sick newborn infants. Pediatr Res. 2000;48:12–7.
Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res. 2007;61:467–73.
Brady KM, Mytar JO, Lee JK, Cameron DE, Vricella LA, Thompson WR, et al. Monitoring cerebral blood flow pressure autoregulation in pediatric patients during cardiac surgery. Stroke. 2010;41:1957–62.
Heldt T, Kashif FM, Sulemanji M, O’Leary HM, du Plessis AJ, Verghese GC. Continuous quantitative monitoring of cerebral oxygen metabolism in neonates by ventilator-gated analysis of NIRS recordings. Acta Neurochir Suppl. 2012;114:177–80.
Naulaers G, Meyns B, Miserez M, Leunens V, Van Huffel S, Casaer P, et al. Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology. 2007;92:120–6.
Massaro AN, Govindan RB, Vezina G, Chang T, Andescavage NN, Wang Y, et al. Impaired cerebral autoregulation and brain injury in newborns with hypoxic-ischemic encephalopathy treated with hypothermia. J Neurophysiol. 2015;114:818–24.
Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ. Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res. 1998;44:591–5.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Govindan RB, Massaro A, Chang T, Vezina G, du Plessis A. A novel technique for quantitative bedside monitoring of neurovascular coupling. J Neurosci Methods. 2016;259:135–42.
Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 2000;106:625–32.
Govindan RB, Massaro AN, Andescavage NN, Chang T, du Plessis A. Cerebral pressure passivity in newborns with encephalopathy undergoing therapeutic hypothermia. Front Hum Neurosci. 2013;8:266.
O’Leary H, Gregas MC, Limperopoulos C, Zaretskaya I, Bassan H, Soul JS, et al. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics. 2009;124:302–9.
Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8:110–24.
du Plessis AJ. The role of systemic hemodynamic disturbances in prematurity-related brain injury. J Child Neurol. 2009;24:1127–40.
du Plessis AJ. Neurologic complications of cardiac disease in the newborn. Clin Perinatol. 1997;24:807–26.
Peyvandi S, Latal B, Miller SP, McQuillen PS. The neonatal brain in critical congenital heart disease: insights and future directions. Neuroimage. 2019;185:776–82.
Vesoulis ZA, Mathur AM. Cerebral autoregulation, brain injury, and the transitioning premature infant. Front Pediatr. 2017;5:64.
Lou HC. The “lost autoregulation hypothesis” and brain lesions in the newborn—an update. Brain Dev. 1988;10:143–6.
Pryds O, Greisen G, Lou H, Friis-Hansen B. Vasoparalysis associated with brain damage in asphyxiated term infants. J Pediatr. 1990;117:119–25.
Brady KM, Lee JK, Kibler KK, Easley RB, Koehler RC, Shaffner DH. Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke. 2008;39:2531–7.
Brady KM, Lee JK, Kibler KK, Smielewski P, Czosnyka M, Easley RB, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38:2818–25.
Lee JK, Yang ZJ, Wang B, Larson AC, Jamrogowicz JL, Kulikowicz E, et al. Noninvasive autoregulation monitoring in a swine model of pediatric cardiac arrest. Anesth Analg. 2012;114:825–36.
Howlett JA, Northington FJ, Gilmore MM, Tekes A, Huisman TA, Parkinson C, et al. Cerebrovascular autoregulation and neurologic injury in neonatal hypoxic-ischemic encephalopathy. Pediatr Res. 2013;74:525–35.
Lee JK, Kibler KK, Benni PB, Easley RB, Czosnyka M, Smielewski P, et al. Cerebrovascular reactivity measured by near-infrared spectroscopy. Stroke. 2009;40:1820–6.
Vesoulis ZA, Liao SM, Trivedi SB, Ters NE, Mathur AM. A novel method for assessing cerebral autoregulation in preterm infants using transfer function analysis. Pediatr Res. 2016;79:453–9.
Perry BG, Lucas SJ, Thomas KN, Cochrane DJ, Mundel T. The effect of hypercapnia on static cerebral autoregulation. Physiol Rep. 2014;2:e12059.
Panerai RB, Deverson ST, Mahony P, Hayes P, Evans DH. Effects of CO2 on dynamic cerebral autoregulation measurement. Physiol Meas. 1999;20:265–75.
Oddo M, Crippa IA, Mehta S, Menon D, Payen JF, Taccone FS, et al. Optimizing sedation in patients with acute brain injury. Crit Care. 2016;20:128.
Alderliesten T, Dix L, Baerts W, Caicedo A, van Huffel S, Naulaers G, et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr Res. 2016;79:55–64.
Funding
This study was supported by (1) internal special-purpose funds in the Fetal Medicine Institute at Children’s National and (2) the Clinical and Translational Science Institute at Children’s National (UL1TR000075, 1KL2RR031987-01) and the National Institutes of Health Intellectual and Developmental Disabilities Research Consortium (U54 HD090257).
Author information
Authors and Affiliations
Contributions
VG performed data collection, performed data analysis, and drafted the initial paper. RG and TA-S performed data analysis. ANM and NNA aided in recruitment of subjects and worked to shape the design of the study. GV and JM performed radiological classification of MRI. YW performed statistical analysis and summarized the results. MM, CC, CS, and DR performed data collection. AP and RG conceptualized and designed the study, supervised data analysis. All authors participated in the interpretation of the results, reviewed, and endorsed the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Govindan, V., Govindan, R., Massaro, A.N. et al. Cerebral venous volume changes and pressure autoregulation in critically ill infants. J Perinatol 40, 806–811 (2020). https://doi.org/10.1038/s41372-020-0626-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0626-0
This article is cited by
-
Effect of the change of mechanical ventilation mode on cerebral oxygen saturation level in neonates
BMC Pediatrics (2023)
-
Cerebral venous volume changes and pressure autoregulation in critically ill infants: an editorial comment
Journal of Perinatology (2020)