Abstract
Introduction: The use of chromosome analysis on products of conception from spontaneous abortions is recommended to identify a genetic etiology. However, 20% of products of conception cultures are unsuccessful due to microbial contamination or lack of viable dividing cells. Our laboratory implemented a reflex fluorescent in situ hybridization (FISH) assay to detect numeric chromosome abnormalities for unsuccessful cultures.
Materials and Methods: All products of conception samples were simultaneously processed for both chromosome analysis and FISH analysis. If the chromosome analysis was unsuccessful, interphase FISH was performed for chromosomes 13, 16, 18, 21, 22, X, and Y. To assess the performance of the FISH assay, a 3-year retrospective comparative analysis of the FISH results versus chromosome results was performed.
Results: Of 5555 total specimens, 4189 (75%) represented chorionic villi/fetal tissue and 1366 (25%) represented tissue of unidentified origin. Of the 1189 tissues of unidentified origin with chromosome or FISH results, 1096 (92%) were XX, indicating that the majority of these tissues are likely maternal in origin. Of the 3361 successful chromosome studies on the chorionic villi/fetal tissue specimens, 1734 (52%) samples had a chromosome abnormality. Of the 762 successful FISH studies on chorionic villi/fetal tissue specimens that were unsuccessful by chromosome studies, 181 (25%) had an abnormal result with the targeted FISH panel. Overall, the FISH panel detected approximately 70% of the chromosome abnormalities in products of conception detectable by karyotype. When the FISH panel results were combined with chromosome analysis for the 4189 chorionic villi/fetal tissue specimens, the overall abnormality rate is 47%.
Conclusions: Our reflex FISH assay proved useful for the detection of common chromosome aneuploidies in products of conception samples that failed conventional chromosome analysis. Because of its limited view of the genome, cautious interpretation of FISH results is required for all samples, in particular, trisomy of an acrocentric chromosome, which may represent a Robertsonian translocation. An algorithmic approach to the genetic evaluation of products of conception specimens, with the potential for initial evaluation by a FISH panel, may be warranted.
Similar content being viewed by others
Main
The estimated maximum likelihood of achieving a pregnancy is 30–40% under optimum conditions.1–3 Given such a low fecundity, it is not surprising that at least 15–20% of clinically recognized pregnancies result in a spontaneous abortion (SA).2 Determining the genetic cause of a miscarriage, the recurrence risk, and chances for a subsequent successful pregnancy impact family planning, management of future pregnancies, and may alleviate feelings of guilt or inadequacy related to the pregnancy loss. Numerous etiologies of SA have been identified, including infection, maternal endocrine imbalances, abnormal uterine anatomy, immunological disorders, and fetal genetic defects.
The most common cause of early pregnancy loss results from a chromosomally abnormal conceptus, accounting for 32–60% of all SA.4–12 Upward of 96% of the chromosomal defects are due to numerical abnormalities, with monosomy X, triploidy, and autosomal trisomy being the most common.13 Chromosome analysis, which requires dividing cells, is the current gold standard for genetic evaluation of products of conception (POC).
Chorionic villus is the tissue of choice, but fetal tissue (i.e., muscle/skin biopsy) or placental tissue may be studied. However, as fetal tissue may be retained in utero for several days or weeks after the fetal demise, the tissue may be autolyzed and unresponsive to standard culture methods. In addition, microbial contamination may impede cell division processes. As a result, approximately 20% of all POC cultures fail to produce a successful chromosome study.
Several alternative assays have been used to evaluate POC genetics, including comparative genomic hybridization (CGH),14,15 array CGH,16–21 quantitative fluorescent polymerase chain reaction (PCR),22 multiplex ligation-dependent probe amplification (MLPA),14,15 and fluorescent in situ hybridization (FISH).23–26 These techniques circumvent the need for dividing tissue and can be readily integrated in the clinical laboratory setting.
To improve the success rate of POC analysis in our laboratory, we implemented a reflex FISH assay to detect common numeric chromosome abnormalities from unsuccessful cultures. All POC samples received in the laboratory were simultaneously processed for both chromosome analysis (cultured) and FISH analysis (uncultured). On an unsuccessful chromosome analysis, an interphase FISH assay consisting of probes for chromosomes 13, 16, 18, 21, 22, X, and Y was performed on the uncultured fixed-cell pellet. Using this algorithm during a 3-year period, our laboratory attempted 5555 POC chromosome analyses of which 943 were subsequently analyzed by our reflex FISH panel test. Herein, we report our findings of a retrospective analysis comparing FISH results with chromosome results for this patient cohort.
MATERIALS AND METHODS
Study design
After Institutional Review Board approval, we conducted a retrospective review of the Mayo Clinic Cytogenetics Laboratory database to identify all POC chromosome and reflex FISH analyses from October 2002 to October 2005. We reviewed the chromosome and FISH results along with tissue type studied. As most of the specimens were referred to our laboratory with a limited amount of clinical data, we were not able to include data on the gestational age, relevant history including recurrent pregnancy loss, use of reproductive assisted technologies, or whether samples were due to elective versus SAs.
Specimen preparation
Tissues were transported to the laboratory in Hank's balanced salt solution. Using a dissecting microscope, the tissue was cleaned and placed in tissue wash solution (antibiotic/antimycotic) overnight at 37°C. The tissue was minced with a sterile scissors and treated for 30–40 minutes with collagenase type V Sigma (1 mg/mL; 2 mL used for approximately 20 mg of tissue). The tissue was then suspended in Hank's balanced salt solution, centrifuged, aspirated, and resuspended with Chang/Minimum Essential Media alpha working solution. Approximately 0.5 mL of this suspension was removed for future interphase FISH analysis. The remaining cell suspension was grown on no. 1 ½ 22 × 22 mm coverslips in 35 × 10 mm Petri dishes (in situ cultures) at 37°C with 5% CO2, 5% O2, and 90% N2. The cultures were harvested using a Tecan robotic harvest system MiniPrep75™ using the standard method for in situ cultures.27 The coverslips were dried in a Thermotron Slide Drying Chamber CDS-5™.28 After slide drying, the slides were submerged in a trypsin working solution followed by a water rinse. Next, the slides were stained with Leishman's stain followed by a brief water rinse. Each specimen had 20–30 metaphase cells analyzed by conventional cytogenetic techniques.
For interphase FISH, 5 mL of sodium citrate hypotonic solution (0.6%) was mixed with the aliquoted 0.5 mL cell suspension. If the culture media was from the first media change, the suspension was centrifuged for 8 minutes at 1000 rpm and removed before the addition of the hypotonic solution. Two milliliters of 2:1 methanol:glacial acetic acid fixative was added to the suspension, mixed, centrifuged for 8 minutes at 1000 rpm, and aspirated followed by the addition of 10 mL fresh fixative. The specimen was stored at −20°C until needed.
If the chromosome analysis was unsuccessful, the FISH specimen was removed from −20°C and allowed to warm to room temperature. The suspension was centrifuged for 8 minutes at 1000 rpm, the supernatant aspirated, followed by the addition of 10 mL fresh fixative. The suspension was centrifuged for another 8 minutes at 1000 rpm followed by the aspiration of supernatant down to 0.5–1.0 mL depending on the pellet size. The cell suspension was then dropped onto four Fisherbrand Fluorescent Antibody Slides with two 15 mm circles in a Thermotron Slide Drying Chamber at 25°C and 50% relative humidity.
FISH protocol
Two slides were aged for 30 minutes in a 65°C oven. The slides were then immersed in a 2× standard saline citrate (SSC) at 37°C for 30 minutes, digested in a 0.9% NaCl pepsin working solution (160 mg pepsin/40 mL 0.9% NaCl) (pH 1.5) at 37°C for 13 minutes, and immediately rinsed in phosphate buffered solution for 5 minutes at room temperature. Next, the slides were immersed in 1% formaldehyde and phosphate buffered solution at room temperature for 5 minutes each. Slides were dehydrated in 70%, 85%, and 100% ethanol for 2 minutes each at room temperature and air dried.
Commercial probes (Abbott Molecular, Abbott Park, IL) were used for the centromere of chromosome 16, a locus-specific probe for chromosome 22 (the bcr gene region), and the AneuVysion™ kit, which consisted of centromere probes for chromosomes X, Y, and 18, and locus-specific probes for chromosomes 13 and 21. The three probe sets, X;Y;18, 13;21, and 16;22, were applied to three separate hybridization targets, coverslipped, and rubber cemented. The slides and probes were codenatured at 73°C for 5 minutes and hybridized overnight in a 37°C humidified oven. After hybridization, the slides were subjected to a posthybridization wash in 0.4× SSC for 2 minutes at 74°C and then rinsed in 2× SSC/0.1% NP-40 for 2 minutes at room temperature. Slides were stained with 4′-6,-diamidino-2-phenylindole and antifade compound (Vectashield) and were coverslipped.
Chromosome and FISH analysis criteria
Cytogenetic analysis was carried out in the Mayo Clinic Cytogenetics laboratory. G-banded slides were analyzed, and all karyotypes were described according to the International System of Human Cytogenetic Nomenclature.
The FISH slides were evaluated using a Leica fluorescent microscope equipped with an appropriate filter wheel and cubes to visualize the SpectrumOrange™, SpectrumGreen™, SpectrumGreen/SpectrumOrange™, and SpectrumAqua™ fluorophores. Two technologists each scored 100 consecutive nonoverlapping nuclei (200 total). After the analysis, the results for both scorers were combined, and the percentage abnormal nuclei were calculated. Normal cutoffs, which were previously established in our laboratory (data not shown), were then used to determine whether the sample was abnormal. The normal cutoffs for trisomy of chromosomes 13, 16, 18, 21, 22, X, and Y were 3%, 8.5%, 6%, 4.5%, 7%, 10%, and 10%, respectively. Monosomy X and triploidy/tetraploidy had normal cutoffs of 20% and 5%, respectively.
RESULTS
Tissue type and abnormality rates
Each sample source was identified to the best of our ability and grouped into chorionic villi, fetal tissue, or unidentified tissue (Table 1). Chorionic villi had the highest success rates of 90% and 96% for chromosome and FISH analyses, respectively. A marked difference, 37% vs. 95%, for fetal tissue success rates was observed by chromosome and FISH analyses, respectively. Both methods had 85% success rates for unidentified tissue. Abnormality rates for chromosome and FISH studies, respectively, were highest for chorionic villi (55% and 36%), followed by fetal tissue (17% and 17%), and unidentified tissue (9% and 15%).
Gender comparison of tissue types for normal results
XY:XX sex ratios for normal samples were computed for both chromosome and FISH analyses (Table 2). When comparing XY:XX sex ratios by tissue type for chromosome studies, chorionic villi had a sex ratio of 1.00, fetal tissue had a sex ratio of 1.1, and unidentified tissue had a sex ratio of 0.05. For FISH studies, XY:XX sex ratios were 1.0 for chorionic villi, 1.1 for fetal tissue, and 0.42 for unidentified tissue. As the sex ratios for both chromosome and FISH results on unidentified tissue strongly indicate that the majority of this tissue is likely maternal, these 1366 samples have been evaluated separately in several subsequent analyses.
Chromosome and reflex FISH results summary
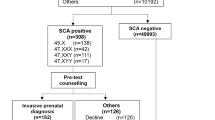
Chromosome analysis in chorionic villi and fetal tissue specimens was successful for 3361 (80%) samples and identified an abnormality in 1734 (52%) samples (Fig. 1). Of the 828 (20%) unsuccessful chorionic villi/fetal tissue samples, 762 were subsequently studied by FISH. Further study of 66 samples was not performed because of either lack of client consent or an insufficient sample. Of the 762 chorionic villi and fetal specimens studied by FISH, a successful analysis was achieved for 727 (95%) samples, and an abnormality was identified in 181 (25%) samples. When the results for chromosome analysis and FISH were combined for the chorionic villi/fetal tissue samples, an abnormality was detected in 1915 of 4088 (47%) successfully analyzed samples.
Unidentified tissue accounted for 1366 (25%) of the total 5555 POC samples evaluated. The overall XY:XX sex ratio for these samples is 0.08 (92% XX and only 8% XY), demonstrating that the overwhelming majority are likely maternal in origin. This assertion is supported by the lower chromosome abnormality rate (9%) and the lower FISH abnormality rate (15%) for these unidentified tissues (Fig. 1).
Abnormal chromosome and FISH result distribution
All 2040 abnormal results were grouped into broad categories listed in Table 3. Pure trisomy, monosomy X, triploidy, and tetraploidy were the most prevalent abnormalities identified by chromosome analysis and FISH. Despite a different tissue composition studied by FISH (i.e., more fetal tissue), similar percentages were observed for the aforementioned abnormalities with the exception of triploidy (12% for chromosome analysis vs. 22% for FISH). Pure trisomy was the most common abnormality detected by both methods followed by monosomy X and triploidy. Forty-nine cases of double trisomy were detected by chromosome analysis (previously published by MiCale et al.29), and only one case was detected by FISH. Single cases each of triple and quadruple trisomy were also observed. Of the 17 autosomal monosomies observed, 14 cases were monosomy 21.
Sixty-one of the 92 structural rearrangements were unbalanced. Of the 61 specimens, the chromosome abnormalities included 27 additions, 19 derivatives, five recombinants, three deletions, three isochromosomes, one marker, one duplication, and one case with both structural and numeric abnormalities. Of the 31 balanced rearrangements, there were 23 translocations and eight inversions. Twenty-six of the balanced rearrangements were XX, whereas five cases (three translocations and two inversions) were XY.
Chromosome and FISH trisomy results
The number of samples observed with a single trisomy by chromosome (n = 1074) and FISH (n = 108) analyses is detailed in Table 4. The three most prevalent trisomies identified by chromosome analysis were chromosomes 16 (23.7%), 22 (14.9%), and 21 (13.1%). At least one case of each autosomal trisomy was observed, with the exception of chromosome 1. For FISH, the three most prevalent trisomies were chromosomes 21 (37%), 18 (22.2%), and 16 (14.8%). Sex chromosome trisomies observed by both chromosome analysis and FISH totaled three cases of XXX and four cases of XYY. No significant gender difference for any trisomy was observed (data not shown).
Robertsonian translocations
Forty-three Robertsonian translocations (RTs) were detected by chromosome analysis (Table 5). Of these, 30 were unbalanced, thus contributing an extra copy of an acrocentric chromosome. The most prevalent RT observed was the der(13;14), which contributed to a gain of chromosomes 13 or 14, in five and six samples, respectively. The der(14;14) was the next most frequently identified translocation in six samples.
The number of samples detected by chromosome analysis with a pure acrocentric trisomy versus a RT trisomy is presented in Table 6. A total of 552 acrocentric trisomies were defined by chromosome studies, including 522 pure trisomies and 30 due to RTs. Chromosome 14 had the highest number of trisomies due to a RT (28% of cases). The FISH panel evaluated only three acrocentric chromosomes, 13, 21, and 22, and a total of 66 trisomies were defined. Extrapolating from the chromosome studies regarding percent of acrocentric trisomies due to RTs, the FISH panel theoretically identified three acrocentric trisomies due to a RT.
DISCUSSION
Overview
The goal of this report is to describe our experience with a two-tier testing algorithm designed to improve the success rate for genetic analysis of our POC samples. It is well established that approximately 50% of first-trimester SA is chromosomally abnormal. 6,8,10,30 Chromosome analysis is the current gold standard for detection of chromosome aberrations; however, approximately 20% of POC samples fail to yield a chromosome result due to culture failure, often attributable to microbial contamination or nonviable tissue.
To improve our success rate, our laboratory implemented a reflex FISH assay to detect common numeric chromosome abnormalities in POC samples with unsuccessful chromosome results. During a 3-year period, the use of our FISH panel on chorionic villi and fetal tissue specimens reduced the number of POC samples without genetic results from 762 to 35 (excluding the 66 samples not analyzed by FISH). Although the FISH panel does not provide results for the entire chromosome complement, approximately 70% of all POC abnormalities detectable by karyotype can be detected by the FISH panel. An overall abnormality rate of 47% was achieved when combining the FISH panel results with the chromosome studies on the 4189 chorionic villi/fetal tissue specimens.
POC tissue type and chromosome versus FISH analyses
Various tissue types from POC are submitted to cytogenetics laboratories, including chorionic villi, fetal tissue, and often, a tissue with an unidentifiable origin (accounting for 25% of samples in our series; Fig. 1). To improve success and abnormality rates, the use of only chorionic villi has been recommended30; however, we continue to test fetal and unidentified tissue in an attempt to identify a genetic cause for the fetal demise. For fetal tissue specimens, the percent abnormal for both chromosome and FISH analyses was identical (17%). However, chromosome analysis produced a result in only 37% of fetal tissue samples, whereas FISH generated a result in 95% of fetal tissue samples. Thus, although our targeted FISH panel yields only a limited view of the genome, our study results indicate that panel FISH testing may be superior to chromosome analysis for the evaluation of fetal tissue.
Chromosome versus FISH analyses for abnormality detection
The specific abnormality frequencies observed by chromosome analysis (Table 3) were comparable with other large POC chromosome studies.8,30–35 Pure trisomy, specifically for chromosomes 16, 22, and 21 (Table 4), monosomy X, and triploidy were the most prevalent abnormalities observed. Structural abnormalities were detected in 5% of all abnormal samples of which 65% were unbalanced.
The lower overall abnormality rate of 23% for our FISH panel can be explained by the sample characteristics (i.e., more fetal tissue and less chorionic villi) and the limited view of the genome provided by the FISH panel. Similar to chromosome analysis, the FISH panel found isolated trisomy to be the most frequent abnormality (53% vs. 58%, respectively; Table 3). However, FISH identified a higher percentage of samples than chromosome studies with monosomy X (21% vs. 14%, respectively) and with triploidy (22% vs. 12%, respectively). These differences seem to be due to mathematical variances because of a restriction of the abnormalities detectable by FISH. To verify this assumption, we removed the 30% of chromosome cases that were not detectable by our FISH panel, and then recalculated the percentage of chromosome cases with monosomy X (20%) and triploidy (17%). These revised percentages more closely approximate the percentages identified by our FISH panel, suggesting these two methods are similar in their evaluation of POC specimens for these genetic subgroups.
Our data showed an infrequent occurrence of sex chromosome trisomy. The sex chromosome trisomies of 47,XXX, 47,XXY, and 47,XYY were observed in three, zero, and four cases by chromosome analysis or FISH, respectively. The observance of these abnormalities at term is approximately 1 in 1000 infants of the appropriate gender.36 Our POC data are not surprising as the overwhelming majority of these individuals have a very mild phenotype. Of interest, in a smaller study of 259 first-trimester miscarriages, Ljunger et al.37 reported a 47,XXY karyotype in nine (3.4%) cases. Our data do not support a similar frequency of this abnormality, as a 47,XXY karyotype was not found in our total of 4088 chorionic villi/fetal tissue samples successfully analyzed for sex chromosome status by chromosome or FISH analysis. The reason for the discrepant percentages of 47,XXY cases between our studies is unclear, but other large POC chromosome studies were similar to our study with very few cases of 47,XXY identified.36
Double trisomy accounted for approximately 3% of abnormalities observed (previously reported in the meta-analysis by Micale et al.29). The sole double trisomy detected by FISH involved chromosomes X and 21. Because of the reduced number of chromosomes tested by our FISH panel, 37 of the 49 double trisomies detected by chromosome analysis would have been missed by FISH. Intuitively, if the testing algorithm used FISH first and identified a single trisomy, further analysis by chromosome studies may not have been performed and, thus, would have prevented the identification of the second trisomy. However, the finding of a second trisomy is generally not clinically relevant as the identification of the first trisomy likely explains the fetal demise.
Autosomal monosomies are infrequently observed in the prenatal setting. The severity of autosomal monosomy likely leads to very early SA, presumably precluding the genetic analysis of these samples. In our data, approximately 1% of all abnormalities were autosomal monosomies. Of these 17 samples, 14 had monosomy 21. However, as three cases were observed by FISH, it is possible that a more complex chromosome abnormality or a simple deletion of the chromosome 21 locus tested by FISH was identified. Our data are similar to that of Menasha et al.,30 where 11 of 13 autosomal monosomies involved chromosome 21. Monosomy 21 has also been described prenatally38,39 and in liveborns.40–45 The majority of these cases did not have molecular confirmation of true monosomy 21. In two cases, the retained chromosome 21 was determined to be of paternal origin implicating a maternal meiosis I nondisjunction event.38,39 The frequency of monosomy 21 vs. other autosomal monosomies in our series suggests a greater survival advantage for this autosomal monosomy.
Robertsonian translocations
RTs are identified in approximately 1 in 1000 newborns.46 We identified 43 RT in our POC series, including 30 unbalanced cases resulting in an acrocentric trisomy, six balanced XY cases, and seven balanced XX cases. As six of the seven balanced XX RT results were derived from an unidentified tissue source (Table 5), these results likely represent maternal tissue and will not be included in further evaluations of this dataset (see subsequent Discussion on maternal cell contamination).
Of the 36 POC specimens from chorionic villi or fetal tissue that had a RT, 15 were homologous RT and 21 were nonhomologous RT. Although parental follow-up was not available for most of our POC cases, the anticipated recurrence risk for the cases with homologous RT is extremely low, as these generally represent new mutations. Of the 21 nonhomologous RT, 14 were the common der(13;14). The der(13;14) is the most prevalent RT in the general population, accounting for 75% of cases.46 Although a der(13;14) carrier parent has only a 1% empiric risk for having a liveborn child with an unbalanced der(13;14), there is a more significant risk for multiple miscarriages due to malsegregation during meiosis. Thus, although any RT identified in a POC by chromosome studies should result in subsequent parental chromosome studies, the identification of a nonhomologous RT increases the likelihood of an abnormal parental chromosome result, particularly in families experiencing multiple miscarriages.
As FISH testing represents a limited view of the genome, the identification of acrocentric trisomies presents a conundrum as to the etiology of the trisomy, i.e., pure trisomy versus a RT. Our POC data on acrocentric trisomies identified by chromosome studies can be extrapolated to predict the number of trisomies observed by FISH that could be due to an unbalanced RT (Table 6). By performing a simple calculation, the percentage of total trisomies due to RT identified by chromosome analysis were calculated and used to extrapolate a theoretical RT cause for trisomy of chromosomes 13, 21, and 22 identified by FISH. As an example, chromosome studies identified 89 cases with trisomy 13, of which nine (10%) represented a RT. The FISH panel identified 15 cases with trisomy 13 for which 10% would yield 1.5 or approximately two cases theoretically due to a RT. The most frequent acrocentric trisomy identified by chromosome studies was chromosome 22 and included 161 cases, with only one case representing a RT. Thus, the incidence of a RT as the cause for trisomy 22 in POC samples is extremely low, suggesting minimal concern for a RT origin of + 22 identified by FISH. Based on the frequency of trisomy 15 observed in our POC chromosome series (110 cases or 10% of all trisomies; Table 4), we have recently added a chromosome 15 probe into our POC FISH panel.
Maternal cell contamination and an unidentified tissue source in POC specimens
Although unidentified tissue grew well in culture, these tissues likely contained heavy maternal cell contamination or represented pure maternal tissue, as our results indicated only 55 cases of 46,XY and 1004 cases of 46,XX (XY:XX sex ratio of 0.05, Table 2). The overgrowth of maternal decidua in the unidentified tissue samples is likely responsible for the low abnormality rate of only 9% by chromosome studies. Thus, the “successful chromosome analysis” obtained in 85% of unidentified tissue samples may mean little, as the 46,XX result is generally maternal in origin.
However, of the 1366 cases of unidentified tissue, 102 samples were identified with abnormal chromosome results, and 23 samples were identified with an abnormal FISH result (Fig. 1). Of the 102 abnormal chromosome results, 32 had an XX sex chromosome complement and a balanced structural rearrangement, including six samples with a 13;14 RT. It should be noted that our clinical interpretation of these XX balanced structural abnormality results from unidentified tissue sources, emphasize the significant possibility that the chromosome results represent the maternal karyotype, and indicate the need for a follow-up maternal peripheral blood chromosome study and a genetic consultation.
A total of 93 abnormalities were detected in unidentified tissues by chromosome or FISH studies, which were trisomy, triploidy, tetraploidy, or an unbalanced structural abnormality. Thus, of 1366 cases of unidentified tissue, 93 (7%) cases yielded an abnormal result likely representing the cause of the fetal demise. The pursuit of genetic studies on unidentified tissues is an individual laboratory decision and obviously resulted in an overall low yield (7% abnormal fetal and 2% abnormal maternal) in our dataset. However, we believe that the evaluation of these tissues is still warranted as the identification of the abnormal results can provide clinically relevant genetic information, although the interpretation must clearly indicate if these results represent the fetal genome, the maternal genome, or possibly both genomes.
Genetic testing algorithm for POC samples
Conventional chromosome analysis continues to be the current gold standard for genetic analysis of POC specimens. However, the generation and propagation of tissue cultures, the expense of technologist effort, and the time required to generate a complete chromosome analysis are significant. In addition, culture failure due to microbial contamination or nonviable tissue results in an unsuccessful outcome in 20% of POC samples. These multiple issues suggest that other testing modalities, including FISH, array CGH, and MLPA, are viable candidates in a potential genetic testing algorithm for POC samples. The use of molecular cytogenetic techniques, specifically array CGH and MLPA, have been investigated for genetic analysis of POC samples.16–21,47,48 Similar to FISH, array CGH and MLPA circumvent the need for cell culture, thereby reducing the incidence of maternal cell overgrowth and possibly negating the effects of microbial contamination. The use of subtelomeric MLPA in POC specimens should identify all trisomies and unbalanced translocations but will miss polyploidy,47 unless an concurrent FISH panel is also evaluated.48 Additionally, array CGH removes the analytic ambiguity of poor chromosome morphology and provides a greater genomic resolution than both chromosome and FISH analysis. However, difficulties in interpretation of array CGH occur due to the detection of polymorphisms or variations of unknown clinical significance, in addition to the missed identification of balanced rearrangements and polyploid states. A possible algorithm for the evaluation of POC specimens could be a FISH panel that identifies the common trisomies, triploid, and tetraploid miscarriage cases followed by array CGH as a reflex test.15 Further larger studies are needed to assess the combination of chromosome analysis, FISH panels, array CGH, and/or MLPA to identify the best algorithm for the most accurate, cost-effective, and timely genetic evaluation of POC specimens.
Conclusions
Through this retrospective study of 5555 POC specimens, our data demonstrate that reflex FISH testing has significantly improved the evaluation of chorionic villi and fetal tissue specimens, with an overall abnormality rate of 47% for these tissues. Our study indicates that a targeted panel of FISH probes, including chromosomes 13, 16, 18, 21, 22, X, and Y, will detect approximately 70% of all POC genetic abnormalities detectable by karyotype. A FISH panel may be particularly advantageous for studying fetal tissue, which often results in culture failure. Our data indicate that the genetic evaluation of unidentified tissue from a POC can yield useful information in approximately 10% of specimens; however, as the overwhelming majority of these tissues are likely maternal, the benefits of proceeding with a full genetic evaluation should be carefully considered. An algorithmic approach to genetic testing of POC specimens with an initial screen by a targeted FISH panel may be warranted. However, as illustrated by our RT data, careful interpretation of all POC FISH results is necessary due to its limited view of the genome. Overall, the use of FISH in combination with chromosome analysis proved beneficial and clearly enhanced POC testing in our laboratory.
References
van Noord-Zaadstra BM, Looman CW, Alsbach H, Habbema JD, te Velde ER, Karbaat J . Delaying childbearing: effect of age on fecundity and outcome of pregnancy. BMJ 1991; 302: 1361–1365.
Zinaman MJ, Clegg ED, Brown CC, O'Connor J, Selevan SG . Estimates of human fertility and pregnancy loss. Fertil Steril 1996; 65: 503–509.
Slama R, Eustache F, Ducot B, et al. Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Hum Reprod 2002; 17: 503–515.
Bowen P, Lee CS . Spontaneous abortion. Chromosome studies on 41 cases and an analysis of maternal age and duration of pregnancy in relation to karyotype. Am J Obstet Gynecol 1969; 104: 973–983.
Boue J, Bou A, Lazar P . Retrospective and prospective epidemiological studies of 1500 karyotyped spontaneous human abortions.[see comment]. Teratology 1975; 12: 11–26.
Warburton D, Stein Z, Kline J, Susser M, Chromosome abnormalities in spontaneous abortion: data from the New York city study. In: Porter IH, Hook EB (eds) Embryonic and fetal death. New York, Academic Press, 1980; 261–287.
Kline J, Stein Z, Epidemiology of chromosomal anomalies in spontaneous abortion: prevalence, manifestation and determinants. In: Bennett MJ, Edmonds DK (eds) Spontaneous and recurrent abortion. Chicago, Oxford Blackwell Scientific, 1987; 29–50.
Hassold T, Chen N, Funkhouser J, et al. A cytogenetic study of 1000 spontaneous abortions. Ann Hum Genet 1980; 44: 151–178.
Kajii T, Ferrier A, Niikawa N, Takahara H, Ohama K, Avirachan S . Anatomic and chromosomal anomalies in 639 spontaneous abortuses. Hum Genet 1980; 55: 87–98.
Hassold T, Chiu D . Maternal age-specific rates of numerical chromosome abnormalities with special reference to trisomy. Hum Genet 1985; 70: 11–17.
Lin CC, De Braekeleer M, Jamro H . Cytogenetic studies in spontaneous abortion: the Calgary experience. Can J Genet Cytol 1985; 27: 565–570.
Dejmek J, Vojtassak J, Malova J . Cytogenetic analysis of 1508 spontaneous abortions originating from south Slovakia. Eur J Obstet Gynecol Reprod Biol 1992; 46: 129–136.
Pflueger SMV, Cytogenetics of spontaneous abortion. In: Gersen SL, Keagle MB (eds) The principles of clinical cytogenetics, 2nd ed. Totowa, NJ, Humana Press Inc., 2004; 323–345.
Daniely M, Barkai G, Goldman B, Aviram-Goldring A . Detection of numerical chromosome aberrations by comparative genomic hybridization. Prenat Diagn 1999; 19: 100–104.
Lomax B, Tang S, Separovic E, et al. Comparative genomic hybridization in combination with flow cytometry improves results of cytogenetic analysis of spontaneous abortions. Am J Hum Genet 2000; 66: 1516–1521.
Benkhalifa M, Kasakyan S, Clement P, et al. Array comparative genomic hybridization profiling of first-trimester spontaneous abortions that fail to grow in vitro. Prenat Diagn 2005; 25: 894–900.
Schaeffer AJ, Chung J, Heretis K, Wong A, Ledbetter DH, Lese Martin C . Comparative genomic hybridization-array analysis enhances the detection of aneuploidies and submicroscopic imbalances in spontaneous miscarriages. Am J Hum Genet 2004; 74: 1168–1174.
Robberecht C, Schuddinck V, Fryns JP, Vermeesch JR . Diagnosis of miscarriages by molecular karyotyping: benefits and pitfalls. Genet Med 2009; 11: 646–654.
Menten B, Swerts K, Delle Chiaie B, et al. Array comparative genomic hybridization and flow cytometry analysis of spontaneous abortions and mors in utero samples. BMC Med Genet 2009; 10: 89.
Warren JE, Turok DK, Maxwell TM, Brothman AR, Silver RM . Array comparative genomic hybridization for genetic evaluation of fetal loss between 10 and 20 weeks of gestation. Obstet Gynecol 2009; 114: 1093–1102.
Shimokawa O, Harada N, Miyake N, et al. Array comparative genomic hybridization analysis in first-trimester spontaneous abortions with ‘normal’ karyotypes. Am J Med Genet A 2006; 140: 1931–1935.
Diego-Alvarez D, Garcia-Hoyos M, Trujillo MJ, et al. Application of quantitative fluorescent PCR with short tandem repeat markers to the study of aneuploidies in spontaneous miscarriages. Hum Reprod 2005; 20: 1235–1243.
Fejgin MD, Pomeranz M, Liberman M, Fishman A, Amiel A . Fluorescent in situ hybridization: an effective and less costly technique for genetic evaluation of products of conception in pregnancy losses. Acta Obstet Gynecol Scand 2005; 84: 860–863.
Lescoat D, Jouan H, Loeuillet-Olivo L, Le Calve M . Fluorescent in situ hybridization (FISH) on paraffin-embedded placental tissues as an adjunct for understanding the etiology of early spontaneous abortion. Prenat Diagn 2005; 25: 314–317.
Jobanputra V, Sobrino A, Kinney A, Kline J, Warburton D . Multiplex interphase FISH as a screen for common aneuploidies in spontaneous abortions. Hum Reprod 2002; 17: 1166–1170.
Moore GE, Ruangvutilert P, Chatzimeletiou K, et al. Examination of trisomy 13, 18 and 21 foetal tissues at different gestational ages using FISH. Eur J Hum Genet 2000; 8: 223–228.
Spurbeck JL, Carlson RO, Allen JE, Dewald GW . Culturing and robotic harvesting of bone marrow, lymph nodes, peripheral blood, fibroblasts, and solid tumors with in situ techniques. Cancer Genet Cytogenet 1988; 32: 59–66.
Spurbeck JL, Zinsmeister AR, Meyer KJ, Jalal SM . Dynamics of chromosome spreading. Am J Med Genet 1996; 61: 387–393.
Micale M, Insko J, Ebrahim SA, Adeyinka A, Runke C, Van Dyke DL . Double trisomy revisited—a multicenter experience. Prenat Diagn 2010; 30: 173–176.
Menasha J, Levy B, Hirschhorn K, Kardon NB . Incidence and spectrum of chromosome abnormalities in spontaneous abortions: new insights from a 12-year study. Genet Med 2005; 7: 251–263.
Philipp T, Philipp K, Reiner A, Beer F, Kalousek DK . Embryoscopic and cytogenetic analysis of 233 missed abortions: factors involved in the pathogenesis of developmental defects of early failed pregnancies. Hum Reprod 2003; 18: 1724–1732.
Sanchez JM, Franzi L, Collia F, De Diaz SL, Panal M, Dubner M . Cytogenetic study of spontaneous abortions by transabdominal villus sampling and direct analysis of villi. Prenat Diagn 1999; 19: 601–603.
Strom CM, Ginsberg N, Applebaum M, et al. Analyses of 95 first-trimester spontaneous abortions by chorionic villus sampling and karyotype. J Assist Reprod Genet 1992; 9: 458–461.
Eiben B, Bartels I, Bahr-Porsch S, et al. Cytogenetic analysis of 750 spontaneous abortions with the direct-preparation method of chorionic villi and its implications for studying genetic causes of pregnancy wastage. Am J Hum Genet 1990; 47: 656–663.
Guerneri S, Bettio D, Simoni G, Brambati B, Lanzani A, Fraccaro M . Prevalence and distribution of chromosome abnormalities in a sample of first trimester internal abortions. Hum Reprod 1987; 2: 735–739.
Simpson JL, Elias S, Sex chromosomal polysomies (47,XXY; 47,XXY; 47,XYY; 47,XXX), sex reversed (46,XX) males, and disorders of the male reproductive ducts. In: Simpson JL, Elias S (eds) Genetics in obstetrics and gynecology. Philadelphia, Saunders, 2003; 323–341.
Ljunger E, Cnattingius S, Lundin C, Anneren G . Chromosomal anomalies in first-trimester miscarriages. Acta Obstet Gynecol Scand 2005; 84: 1103–1107.
Mori MA, Lapunzina P, Delicado A, et al. A prenatally diagnosed patient with full monosomy 21: ultrasound, cytogenetic, clinical, molecular, and necropsy findings. Am J Med Genet 2004; 127: 69–73.
Joosten AM, De Vos S, Van Opstal D, Brandenburg H, Gaillard JL, Vermeij-Keers C . Full monosomy 21, prenatally diagnosed by fluorescent in situ hybridization. Prenat Diagn 1997; 17: 271–275.
Dziuba P, Dziekanowska D, Hubner H . A female infant with monosomy 21. Hum Genet 1976; 31: 351–353.
Fryns JP, D'Hondt F, Goddeeris P, van den Berghe H . Full monosomy 21: a clinically recognizable syndrome?. Hum Genet 1977; 37: 155–159.
Garzici B, Gu-Seki M, Pili-Radivojevi G, Ignjatovi M, Vilhar N . A case of monosomy 21. Ann Genet 1988; 31: 247–249.
Herva R, Koivisto M, Seppanen U . 21-Monosomy in a liveborn male infant. Eur J Pediatr 1983; 140: 57–59.
Houston CS, Chudley AE . Separating monosomy-21 from the “arthrogryposis basket”. J Can Assoc Radiol 1981; 32: 220–223.
Pellissier MC, Philip N, Voelckel-Baeteman MA, Mattei MG, Mattei JF . Monosomy 21: a new case confirmed by in situ hybridization. Hum Genet 1987; 75: 95–96.
Gardner RJM, Sutherland GR . Chromosome abnormalities and genetic counselling, 2nd ed. Oxford, Oxford University Press, 1996.
Diego-Alvarez D, Rodriguez de Alba M, Cardero-Merlo R, et al. MLPA as a screening method of aneuploidy and unbalanced chromosomal rearrangements in spontaneous miscarriages. Prenat Diagn 2007; 27: 765–771.
Bruno DL, Burgess T, Ren H, et al. High-throughput analysis of chromosome abnormality in spontaneous miscarriage using an MLPA subtelomere assay with an ancillary FISH test for polyploidy. Am J Med Genet A 2006; 140: 2786–2793.
Acknowledgements
This article is fondly dedicated to my primary mentor in clinical cytogenetics, Dr. Syed Jalal, whose tutelage and enthusiasm for congenital cytogenetics are unequaled (R.P.K.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shearer, B., Thorland, E., Carlson, A. et al. Reflex fluorescent in situ hybridization testing for unsuccessful product of conception cultures: A retrospective analysis of 5555 samples attempted by conventional cytogenetics and fluorescent in situ hybridization. Genet Med 13, 545–552 (2011). https://doi.org/10.1097/GIM.0b013e31820c685b
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31820c685b
Keywords
This article is cited by
-
Comprehensive analysis of 204 sporadic hydatidiform moles: revisiting risk factors and their correlations with the molar genotypes
Modern Pathology (2020)
-
Fertility after recurrent miscarriages: results of an observational cohort study
Archives of Gynecology and Obstetrics (2018)
-
Chromosomal abnormalities in products of conception of first-trimester miscarriages detected by conventional cytogenetic analysis: a review of 1000 cases
Journal of Assisted Reproduction and Genetics (2018)
-
Correlation analysis between ultrasound findings and abnormal karyotypes in the embryos from early pregnancy loss after in vitro fertilization-embryo transfer
Journal of Assisted Reproduction and Genetics (2017)
-
Chromosomal copy number analysis on chorionic villus samples from early spontaneous miscarriages by high throughput genetic technology
Molecular Cytogenetics (2016)