Abstract
Background: Newborn screening is a complex system of interrelated multidimensional components singly focused on safeguarding the health of our nation's newborns. The long-term health outcome and well-being of individuals identified by newborn screening represents a meaningful measurement of the performance of the newborn screening system. This assessment of long-term follow-up requires a systems approach that connects stakeholders, processes, and outcomes through the collection, integration, evaluation, and sharing of key data and metrics.
Methods: A review of the principles of a systems approach and its application to newborn screening long-term follow-up was performed. Past and current efforts by HRSA/MCHB that address individual components of newborn screening were assessed and utilized to outline lessons learned and suggest next steps.
Results: The principle features of a systems approach applied to the creation and utilization of a health information exchange system for the long-term follow up of screen positive patients is defined. The application of this approach is in progress through the HRSA/MCHB's Effective Follow-up in Newborn Screening project.
Conclusions: While several elements are in place to realize a systems approach, the authors think that the key is an integrated, multidirectional health information exchange system that functions locally, regionally and nationally, and enables information exchange between private and public health sectors.
Similar content being viewed by others
NEWBORN SCREENING
At birth, all newborns receive a variety of clinical services for the prevention and diagnosis of illness. Within the first 1–2 days of life, the infant has received immunizations, undergone screening for hearing loss, has a birth certificate established, and has been registered for Social Security. In addition, the 4.3 million infants born in the United States undergo a blood screening test to identify potentially debilitating or fatal congenital or inherited conditions. Currently, the US Secretary of Health and Human Services' Advisory Committee on Heritable Disorders in Newborns and Children (Secretary's Advisory Committee) recommends that State newborn screening programs screen for 29 disorders, defining a recommended uniform panel. This testing facilitates the timely diagnosis and treatment of affected infants before the onset of disease symptoms. Infants diagnosed with these diseases require lifelong care. Newborn screening programs are state based and involve a variety of caregivers with most residing in public health, specialty, and primary care centers.
Newborn screening programs are a multifaceted system of education, screening, diagnosis and referral (short-term follow-up [STFU]), treatment and care management (long-term follow-up [LTFU]), and ongoing evaluation of the effectiveness of all components. Education about newborn screening optimally begins prenatally, and information is provided to prospective parents by their obstetrician. The screening process for the infant begins in the hospital or birthing facility. Currently, there are two types of screening performed: one requires blood (dried blood spot screening) and the other is physiologic (hearing screening). For dried blood spot screening, blood is obtained from the newborn infant (usually by a heel stick) and applied to special standardized filter paper. The filter paper has an attached sheet of demographic and specimen information forming a card. The infant is tested for hearing deficiencies using electrophysiological measurement of acoustic impedance. In some states, the results of the hearing screen and other information are recorded on the same card, which is sent to the newborn screening laboratory. The laboratory may be located in a public health department, an academic center, or may be privately owned.
The transfer of the specimen to the laboratory begins a sequence of processes that requires careful coordination and communication, both to protect the specimen and honor the privacy of the infant and at the same time to communicate information to assure the well-being of that infant. Infants who have a positive screening test are usually asymptomatic and undergo STFU procedures designed to confirm the positive screen, communicate with the parents and family, establish a diagnosis of the disease, and refer the infant to specialty care and treatment. Confirmatory testing is an important first step in STFU and involves additional testing of the original dried blood spot using a variety of technology platforms that may be more specific and more sensitive than the process used for the initial screen.1 Communication with the family is key, and the process may begin once a positive screen is confirmed. Guidelines for both the pediatrician and subspecialty provider (Action Sheets) directing these short-term activities for each of the 29 disorders and the ultimate diagnosis and referral of affected infants were developed by the American College of Medical Genetics through sponsorship by the Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA).2,3 The duration of the STFU process varies with each disorder but does not usually last longer than a few months.
Once the initial diagnosis and referral has taken place, patients become part of a LTFU system for the care and management of their disease through a medical home. Recently, the Secretary's Advisory Committee defined the primary goal of the LTFU care as insuring the best possible health outcome for patients throughout their lifetime.4 Optimizing the health of newborn screening identified individuals over many years presents a challenge to the health care team and system for several reasons. Because of the rarity of the majority of disorders identified through newborn screening, the evidence base often lacks the number of cases required to statistically determine best practice treatment approaches. The chronic nature of these conditions is often a burden on the patient, their families, and caregivers because adherence to complex treatment regimens and preventive care is necessary to avoid further complications and deterioration of health. Patients often have limited access to specialty care and care coordination, and the existing health care delivery teams may not have mechanisms in place to adapt on the front line to identify and incorporate new treatments and to retire ineffective interventions. To address these challenges and others, the Secretary's Advisory Committee defined the components of LTFU as care coordination through a medical home, evidence-based treatment, continuous quality improvement, and new knowledge discovery. The identification of LTFU components provides a guide as newborn screening programs develop, expand, and improve the health management of children over time.
As the identification, diagnosis, and care of newborn screen identified patients improves, the survival of patients often extends into the adult years. Newborn screening programs typically follow-up patients from birth to 21 years, and transition of these patients to adult services while maintaining access to condition-specific therapy that incorporates the latest medical findings also is very important. Similarly, continuing to track the health outcome of these patients is the key to advancing the knowledge base for each of the newborn screening disorders. It is understood that successful newborn screening systems rely on the collection, sharing and integration of data among the family, clinical care providers, and public health programs, and currently, states do not have the capacity to track newborn screen-identified patients.5
Taken as a whole, improvement in newborn screening since the publication in 2000 of the American Academy of Pediatrics Newborn Screening Task Force's report outlining the framework for state-based newborn screening programs has been substantial.6 State, federal, and industry initiatives (many funded by HRSA/MCHB) have facilitated a number of innovative and important developments including the definition of a minimum uniform panel of disorders appropriate for newborn screening, establishment of a nomination and evidence-based review process that considers new disorders and technologies for inclusion in the uniform panel, and the definition of LTFU goals and components. The definition of a uniform panel provided a common goal for newborn screening programs and led to the successful implementation of screening for all 29 disorders in every state. This system-wide change removed the disparities in screening between states and provided access to best practice testing for our nation's newborns and their families. The state newborn screening programs efforts to expand testing also fostered communication between individual medical practices, state public health departments, the seven MCHB established regional collaboratives (RC), and national groups including the Centers for Disease Control and Prevention, the National Institute for Child Health and Development, and the March of Dimes.
SYSTEMS APPROACH
Recognizing that efforts to optimize and perfect the screening, diagnosis, and STFU of newborns is ongoing and remains a priority; our attention now turns to the lifelong care of newborn screening identified patients and the generation of new knowledge. These LTFU processes require the health management of children over time and multidirectional communication among parents, public health officials, medical subspecialists, primary care physicians, researchers, and policy makers. Ideally, this communication and care coordination would extend to school personnel, employment training programs, and relevant community-based organizations while providing a bridge to adult care and services.
Information exchange is the common thread that connects screening, diagnosis, short-term treatment, referral to specialty care, follow-up over time, and transition to adulthood. Information that captures the key elements of each individual patient and links them to a larger set of data provides the necessary foundation for assessing the optimal health outcome of all newborn screening identified patients on an individual basis and enabling the discovery of new treatment approaches and care management strategies with population wide outcome improvements. The importance of these individual data needs is widely recognized but a systematic approach to the achievement of health information exchange (HIE) is lacking. In short, using information exchange systems allows an iterative and integrated approach to assessment, to new knowledge discovery, and to surveillance.
A systems approach is useful in managing and organizing complex systems and has been successfully used in diverse disciplines including government, the military, business, and science. This approach identifies the objectives of a complex system, develops strategies for achieving the defined objectives, and operationalizes those strategies into a comprehensive program whose success can be measured and maintained (Fig. 1). Recently, several groups have applied a systems approach to improving health care delivery across a variety of settings. One example is the Pittsburgh Regional Healthcare Initiative successfully used a systems approach to organize a collaborative of hospitals, insurers, health care purchasers, and civic leaders and link patient outcomes with processes of care.7
The most important step in a systems approach is the identification of common system-wide goals, and a frequently used method involves a survey of the individuals and groups who are part of and impacted by the system. This stakeholder analysis focuses on the overall goals of the system without considering the steps needed to achieve the proposed objectives. The next step is to develop strategies to meet the objectives, recognizing that it may be helpful to consider multiple strategies with different methodologies. Once the strategic plan is in place, establishing quantifiable measures that accurately reflect the performance of the system and provide an indicator of success is important. Success is defined as meeting the identified objective(s), and it is important to create measures that are reliable and valid. The strategies are then implemented into an operational program whose performance is measurable and enables system-level program revisions when necessary. Using a systems approach to improve the long-term care of newborn screening identified patients will bring us closer to linking “what we discover to what we deliver and, what we know to what we do for all people.”8
Application to long-term follow-up
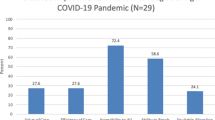
Of more than 4 million newborns screened, approximately 4000 (0.1%) are expected to be identified as having a condition that requires treatment and LTFU. Table 1 estimates the annual and cumulative number of newborn screening identified patients using the uniform panel of 29 disorders. Although this is only an estimate, it is helpful to understand the size of the patient population served by a comprehensive LTFU HIE and management system.
Applying the systems approach to establishing a LTFU data system begins with identifying the system objectives. Although achieving the best possible health outcome for individual patients is the common objective of LTFU, the objectives for a data system are expected to differ across the various system levels (individual practice, state program, RC, and national) due to many differences including information technology capabilities, access to resources, and engagement of stakeholders and funding sources. For example, HRSA/MCHB's primary goal in developing and funding its initiatives was to improve the health outcomes of the infants identified through newborn screening. Other federal agencies envision the creation of large data sets to generate information about diagnostic and treatment approaches that can then be used to assess newborn screening program performance and identify areas for improvement.
The strategies to achieve these objectives are designed to create HIE tools using easily accessible information technology methods and occur in a stepwise fashion. First is the creation of a set of minimum data elements required for managing the health of newborn screening identified patients and determining health outcomes on individual, local, state, and national levels. This is followed by the development of informatics tools and platforms to capture data generated at all system levels including individual medical practices, newborn screening laboratories, public health departments, family history, and medical records. Next is creation of secure data sharing tools using a “need to know” guideline to facilitate timely and effective care of patients and monitoring of newborn screening program. Analysis of data across time to generate performance measurements at all levels of the system results in data dashboards that are useful for day-to-day operations and to enable system-wide performance measurements. Finally, this data system should possess the capacity to implement consensus-driven updates to the system to improve the quality of health care and increase accessibility to quality health care. It is expected that each state and/or region may develop a different strategy based on individual state considerations including access to resources, available information technology infrastructure, and expertise.
The operational program will be a comprehensive HIE system that implements the proposed strategies at individual, local, state, and national levels. In addition, the operational program fosters local, statewide, and national comprehensive care planning to target and achieve optimal health outcomes. The LTFU HIE system enables real-time symptom management and ensures treatment effectiveness by empowering front-line caregivers to implement the most recent evidence-based best practice. Implementation of evolving best practice approaches and the subsequent health outcomes of individual patients provide a continual supply of new data that can be analyzed at a system-wide level ensuring reassessment and revision of program strategies and objectives.
Although treatment and follow-up approaches vary across local, state, and regional boundaries, all seek to improve health outcomes while maximizing the use of health care dollars. This alignment allows the creation of performance-based measurements. Performance measurements can then be used to maintain treatment strategies that are successful and to support measurable improvements in approaches that are not successful. Evaluation of the performance measurements enables system-level revisions to improve timely and appropriate access to care and reinforces the effective utilization of local, regional, and national care plans and guidelines. Identification of patients who do not achieve the best possible health outcome due to minority status, poverty, lack of access to health care, lack of education, and the uninsured or underinsured may also be possible.
PROGRESS TO DATE
HRSA/MCHB began its work in this arena in 1999 with an evaluation of State newborn screening programs and the systems that had been developed to support them. Recommendations from the Newborn Screening Task Force (convened by the American Academy of Pediatrics at the request of HRSA: Report entitled, Serving the Family From Birth to the Medical Home: Newborn Screening: A Blueprint for the Future [A Call for a National Agenda on State Newborn Screening Programs]) recognized that effective newborn screening systems require an adequate public health infrastructure and must be integrated with the health care delivery system to be effective. Furthermore, the Task Force recommended that public health agencies ensure adequate infrastructure and policies for surveillance and research related to newborn screening. Finally, they recommended that grants from HRSA “facilitate and foster the involvement of newborn screening systems in infrastructure development activities in States …” to “… encourage States to consider integration of heelstick programs with a core set of other newborn programs, including birth registration, immunization, newborn hearing screening, and possibly the WIC (Women, Infants, and Children) program,” recognizing that “improved coordination and integration of child health information systems (CHIS) is needed.”
Concurrent to the evaluation by the Newborn Screening Task Force, two surveys of state newborn screening programs and pediatricians were conducted to ascertain the level of communication between the State newborn screening program and pediatric providers. Results from these surveys indicated that there is a need for augmented communication systems to directly interface the primary care pediatrician with the State newborn screening system “to enhance timely retrieval of screen-positive newborns, access follow-up test results and provide documentation for all test results, both positive and negative.”
With this information from the surveys and the recommendations from the Task Force, HRSA/MCHB launched several grant initiatives to encourage the development, to enhance and expand newborn screening programs, and to improve linkages among them and the state and community systems of care. During the years 1999–2006, HRSA/MCHB funded planning grants to 22 states and implementation grants to 16 states, and 13 of the implementation grantees went on to receive additional planning grants.
In addition, HRSA/MCHB began collaborative activities with the Public Health Informatics Institute to focus on specific areas of grantee needs and formed a community of practice, Connections (a group of states, counties, and cities collaborating to promote the health of our nation's children), to assess state efforts to integrate child health information systems; define the business process requirements for the newborn screening system; develop an HL7 implementation guide for electronic sharing of newborn screening results with clinical providers and submission to the Health care Information Technology Standards Panel; and develop an evaluation toolkit for integrated child health information systems.
Building on the preceding activities and in anticipation of the release of the report on newborn screening from the American College of Medical Genetics, calling for uniformity between the States and expansion of screening panels, HRSA/MCHB launched the Regional Genetics and Newborn Screening Collaboratives initiative. Four relevant projects have developed in the RC through this initiative:
Regional Genetic and Newborn Screening Service Collaboratives (2004-present):
-
1
Inborn Errors of Metabolism information System: Region 4 Genetics Collaborative. Develop and implement a comprehensive Inborn Errors of Metabolism Information System and anticipate that the Inborn Errors of Metabolism Information System will result in evidence-based care protocols for children with metabolic disorders and improved health outcomes.
-
2
LTFU: Region 3 Southeast Genetics Collaborative. Development and use of an information system that will include a database to track patient and disease-oriented outcomes detected through tandem mass spectrometry in collaboration, including defining the information system requirements of a LTFU information system through a business process methodology, in collaboration with Public Health Informatics Institute.
-
3
Building on the Foundation of Six New England States' Comprehensive Newborn Screening Programs for Sustainable Follow-up: Region 2 New England Genetics Collaborative. Establishment of a sustainable systematic public health approach to LTFU based on the success of comprehensive newborn screening systems and compatible with national endeavors, with a primary focus on a Regional Charter Agreement for Best Practice and data sharing.
-
4
Pilot Testing Adaptive Turnaround Documents to Link Newborn Screening Programs, Subspecialists, and the Medical Home: Region 4 Genetics Collaborative. The project includes encoding newborn screening test results in Logical Observation Identifiers Names and Codes (LOINC®). This project resulted in coding for all conditions recommended for screening and collaboration with the National Library of Medicine has ensued.
Most recently, HRSA/MCHB began projects under the initiative, Effective Follow-up in Newborn Screening (2009–2012), to implement models of meaningful electronic HIE for attaining effective STFU and LTFU of children and youths with conditions identified by newborn screening, including the evaluation of benefits accrued by the individual throughout his or her life. This initiative's activities focus on the use of electronic HIE to improve the newborn screening system, with attention to both STFU and LTFU, per the guidance offered in the statement on LTFU after diagnosis resulting from newborn screening from the Secretary's Advisory Committee (located: http://www.hrsa.gov/heritabledisorderscommittee/reports/longtermfollowupafternewborn.htm). Three states were funded in September 2009: New York, Indiana, and Utah; an additional state will be funded in October 2010.
LESSONS LEARNED
What began as seemingly simple and straightforward information system integration projects in 1999 has grown into the realization that building the capacity for HIE is extremely complex. Although in some states physicians have the option to check newborn screening results by accessing a secured website, communication is still not multidimensional; most communication continues as hard copy or telephone.
We have garnered many lessons with our grantees over the past 10 years and in no order of priority discuss them here:
-
First, recognize that establishing an integrated HIE system is a difficult and complex undertaking. Often, the project's success will depend on one or two champions; however, strong organizational commitment is crucial. There are many barriers, generally financial or political.
-
Begin your projects in an incremental fashion. Although you need to know where you are headed, outlining a methodical approach with short-term goals allows adaptation to possible changes in technology or the political or financial environment; demonstration of concrete successes; capturing of political support with each success; and ability to be responsive to programs in a tangible fashion. Anticipating the need for or planning for change should be part of the approach to your project.
-
Involve partners necessary to the project from the beginning. Collaboration between the various stakeholders in the newborn screening system is a necessary underpinning for a successful project. Remember that the HIE infrastructure is built to enable communication between people not machines. Therefore, program needs, not HIE technology, must drive the communication system. The requirements for the system should be designed to support users' needs. HIE technology capacity might pose barriers, but the technology should not determine the priorities for the infrastructure to be developed. A necessary component of stakeholder involvement is often presenting a policy or business case for the undertaking.
NEXT STEPS
The infrastructure and the information system to communicate information in an unencumbered manner about newborn screening test results, treatment regimens, and health outcomes to the multiple newborn screening stakeholders is essential for the well-being of the screen-positive infant. The care of the infant requires close communication with the newborn screening program and communication between the family and the program and various health care providers and between the pediatrician and subspecialist. Primary care health care professionals require immediate access to screening results, clinical and diagnostic information, and treatment regimens. Subspecialists are intimately tied to the newborn screening process, participating in diagnostic evaluations and confirmatory testing. Subspecialists often provide the clinical care that might be required immediately by the infant. All are involved in educating the family.
This system of communication must assure and facilitate appropriate and coordinated sample collection, laboratory testing, diagnosis, timely treatment, tracking of outcomes, and, ultimately, referral to a medical home for care coordination. Electronic HIE and interoperability at the point of service delivery are not easy to achieve. Although health information technology has proliferated and advanced dramatically in the last 10 years, the application of information technology to health care and policy formation around health care delivery has not been well coordinated either among public health agencies or between public and private health sectors. Health information systems in the private sector increasingly are exchanging data with other private sector systems to increase efficiencies and quality of care, but they rarely exchange data with the public health sector, which has population-based information.
It is expected that the four projects funded through HRSA/MCHB's latest initiative, Effective Follow-up in Newborn Screening, will serve as a cadre to achieve consensus toward standards development, clarify the business processes involved in HIE within the newborn screening system, and ultimately to achieve multidirectional communication between stakeholders within the newborn screening system.
REFERENCES
Follow-up testing for metabolic diseases identified by expanded newborn screening using tandem mass spectrometry. Clin Chem 2009; 13100v1.
Watson MS, Lloyd-Puryear MA, Mann MY, et al. Newborn screening: Toward a uniform screening panel and system [main report]. Genet Med 2006; 8( suppl): 12S–252S.
Available at: http://www.acmg.net/AM/Template.cfm?Section=ACT_Sheets_and_Confirmatory_Algorithms&Template=/CM/HTMLDisplay.cfm&ContentID=5661. Accessed November 10, 2010.
Kemper A, Boyle CA, Aceves J, et al. Long-term follow-up after diagnosis resulting from newborn screening: statement of the US Secretary of Health and Human Services' Advisory Committee on heritable disorders and genetic diseases in newborns and children. Genet Med 2008; 10: 259–261.
Hinman A, Mann MY, Singh RH, NDBS Business Process Analysis Workgroup. Newborn dried bloodspot screening: mapping the clinical and public health components and activities. Genet Med 2009; 11: 418–424.
Serving the family from birth to the medical home. Newborn screening: a blueprint for the future. A call for a national agenda on state newborn screening programs, Pediatrics 2000; 106: 389–427.
Sirio C, Segel KT, Keyser DJ, et al. Pittsburgh regional healthcare initiative: a systems approach for achieving perfect patient care. Health Aff 2003; 22: 157–165.
Freeman H . Poverty, culture, and social justice: determinants of cancer disparities. CA Cancer. J Clin 2004; 54: 72–77.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lloyd-Puryear, M., Brower, A. Long-term follow-up in newborn screening: A systems approach for improving health outcomes. Genet Med 12 (Suppl 12), S256–S260 (2010). https://doi.org/10.1097/GIM.0b013e3181fe5d9c
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181fe5d9c
Keywords
This article is cited by
-
A population-based registry as a source of health indicators for rare diseases: the ten-year experience of the Veneto Region’s rare diseases registry
Orphanet Journal of Rare Diseases (2014)