Abstract
Background
The perceptions of discharge readiness differ among caregivers and providers. An efficient planning process ensures timely attainment of discharge readiness. Our aim was to increase the percentage of discharge orders placed by 10 a.m. from 0.5% to 10% within 6 months thereby improving discharge readiness.
Methods
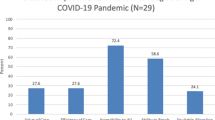
We conducted a quality improvement initiative in the newborn nursery between March 2021 and June 2022 (n = 2307). We implemented a physician-led early discharge huddle and standardized the newborn screen (NBS) and circumcision process.
Results
By 10 a.m., our primary outcome measure, discharge orders, improved from 0.5 to 19%. Our process measures also increased. NBS specimens collected improved from 56 % to 98 % and circumcision rates increased from 66 to 88%. Balancing measure of postpartum hospital days remained stable.
Conclusions
Optimizing family-centered discharge processes by addressing key drivers is essential and can be achieved without an increase in postpartum hospital days.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gonçalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2016;2016:CD000313.
Bernstein HH, Spino C, Finch S, Wasserman R, Slora E, Lalama C, et al. Decision-making for postpartum discharge of 4300 mothers and their healthy infants: the Life Around Newborn Discharge study. Pediatrics 2007;120:e391–e400.
Huber DL, McClelland E. Patient preferences and discharge planning transitions. J Prof Nurs. 2003;19:204–10.
Cadel L, Guilcher SJT, Kokorelias KM, Sutherland J, Glasby J, Kiran T, et al. Initiatives for improving delayed discharge from a hospital setting: a scoping review. BMJ Open. 2021;11:e044291.
Challis D, Hughes J, Xie C, Jolley D. An examination of factors influencing delayed discharge of older people from hospital. Int J Geriatr Psychiatry. 2014;29:160–8.
Mustafa A, Mahgoub S. Understanding and overcoming barriers to timely discharge from the pediatric units. BMJ Qual Improv Rep. 2016;5:u209098.w3772.
Rochester NT, Banach LP, Hoffner W, Zeltser D, Lewis P, Seelbach E, et al. Facilitating the timely discharge of well newborns by using quality improvement methods. Pediatrics 2018;141:e20170872.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25:986–92.
Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458–64.
Benneyan JC. Use and interpretation of statistical quality control charts. Int J Qual Health Care. 1998;10:69–73.
Provost LP, Murray SK. The health care data guide: learning from data for improvement. San Francisco, CA: Jossy-Bass; 2011
Warsame R, Kasi PM, Villasboas-Bisneto JC, Gallenberg D, Wolf R, Ward J, et al. Transition of care for inpatient hematology patients receiving chemotherapy: development of hospital discharge huddle process and effects of implementation. J Oncol Pr. 2016;12:e88–e94.
Tielbur BR, Rice Cella DE, Currie A, Roach JD, Mattingly B, Boone J, et al. Discharge huddle outfitted with mobile technology improves efficiency of transitioning stroke patients into follow-up care. Am J Med Qual. 2015;30:36–44.
Clay AM, Parsh B. Patient- and family-centered care: it’s not just for pediatrics anymore. AMA J Ethics. 2016;18:40–4.
Acknowledgements
We thank Dr Manimaran Ramani and Dr Keith Peevy for critically reviewing the manuscript for important intellectual content. We also thank the entire newborn nursery team who made implementation of this project possible.
Author information
Authors and Affiliations
Contributions
KI conceptualized and designed the initiative, participated in the development and implementation of all phases of the PDSA cycles, managed data, led the statistical analysis developed the control charts and figures, drafted the initial manuscript and reviewed and revised the final manuscript; KN conceptualized and designed the initiative, participated in the development and implementation of all phases of the PDSA cycles, managed data, and reviewed the final manuscript; KD designed the initiative from the earliest stages, participated in the development and implementation of PDSA cycles, and reviewed the final manuscript; TR, AS and CS participated in the development and implementation of all phases of the PDSA cycles, and reviewed the final manuscript; MZ conceptualized and designed the initiative, participated in the development and implementation of all phases of the PDSA cycles contributed to the initial draft of the manuscript, managed data, developed the table, reviewed for critical intellectual content and revised the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ikeri, K., Noles, K., Dolma, K. et al. Optimizing the hospital discharge process to facilitate family-centered care for well newborns. J Perinatol 43, 952–957 (2023). https://doi.org/10.1038/s41372-023-01703-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01703-7