Abstract
Recent automated applanation tonometry can measure radial pulse wave-derived central blood pressure (CBP), which has shown a prognostic value independently of peripheral blood pressure. However, CBP's clinical significance has not been fully established. We examined the associations between CBP and cardiac structure and function by comparing them with those of arterial stiffness assessed by cardio-ankle vascular index (CAVI) in treated hypertensive patients. Enrolled in the study were 102 patients (71±7 years) with treated hypertension. The transmitral early-to-atrial velocity ratio (E/A), peak systolic (S′), early diastolic (E′) mitral annular velocities and the Tei index were measured as indexes of cardiac function derived from conventional and tissue Doppler echocardiography. Left ventricular mass index (LVMI) was measured as an index of LV hypertrophy. CBP and CAVI were measured just after echocardiographic examination. CBP, but not CAVI, correlated with LVMI (r=0.306, P<0.01). Although CBP correlated only with the Tei index (r=0.201, P<0.05), CAVI correlated with E/A (r=−0.387, P<0.001), S′ (r=−0.270, P<0.01), E′ (r=−0.362, P<0.01) and the Tei index (r=0.339, P<0.01). Stepwise regression analysis revealed that neither CBP nor CAVI was independently associated with E/A, S′ or E′. However, CAVI, but not CBP, was independently associated with the Tei index (β coefficient=0.311, P<0.001), reflecting both LV systolic and diastolic function. In conclusion, CBP may be suitable for detecting LV hypertrophy. In contrast, CAVI may be suitable for detecting LV dysfunction. This difference, suggesting the clinical value of each parameter, should be kept in mind when we use CBP and CAVI for assessing arteriosclerosis in treated hypertension.
Similar content being viewed by others
Introduction
It is well known that blood pressure management is important for the prevention of cardiovascular events.1, 2 Brachial blood pressure, which is usually measured in clinical settings, is an essential parameter for the evaluation and management of blood pressure. On the other hand, central blood pressure (CBP), reflecting ascending aortic blood pressure, has also been important because its elevation induces coronary atherosclerosis.3, 4 In addition, CBP is thought to reflect direct stress on the heart because it expresses the pressure-loading condition next to the heart compared with peripheral blood pressure.5, 6 The large-scale ASCOT-CAFÉ study7 reported that CBP may be a determinant of clinical outcomes and that brachial blood pressure is not always a good indicator of a drug's blood pressure-lowering effect on arterial hemodynamics (CAFÉ trial).
Recently, CBP has been evaluated noninvasively by mathematically transforming the radial artery pulse waveform to the aortic pulse waveform,6, 8, 9 and it has been measured widely in clinical settings. However, the clinical significance of CBP, which can be measured easily by automated applanation tonometry, has not been fully elucidated. We hypothesize that CBP may reflect cardiac structure and function better than peripheral blood pressure and that it may show a better correlation with cardiac function compared with the cardio-ankle vascular index (CAVI), which has been an established marker of arterial stiffness from the aortic valve to the ankle.10, 11, 12 In this study, we examined the associations between CBP and cardiac structure and function by comparing them with those of arterial stiffness assessed by CAVI in treated hypertensive patients.
Methods
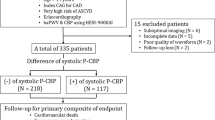
Subjects and protocol
The study subjects were 102 patients (62 males, 40 females; mean age, 71±7 years; range, 55–84 years) who had been diagnosed with hypertension at Kagawa University Hospital and who had regularly visited the outpatient clinic from April 2008 through March 2009. Hypertension was defined as systolic blood pressure ⩾140 mm Hg and/or diastolic blood pressure ⩾90 mm Hg. Blood pressure was determined using the conventional cuff method. All patients were treated with at least one antihypertensive drug. For at least 1 year during their enrollment in this study, the antihypertensive drugs did not change for any patients. Patients with a history of heart failure or obvious heart disease were excluded. None of the patients had a history of atherosclerotic cardiovascular disease or stroke. Echocardiographic examinations were performed to assess cardiac structural changes and cardiac function. CAVI and CBP were measured just after echocardiographic examination. Blood samples were taken in the morning after a 12-h overnight fast. Plasma total cholesterol, triglyceride, high-density lipoprotein cholesterol (HDL-C), serum creatinine, hemoglobin and HbA1c were measured by standard laboratory techniques. The estimated glomerular filtration rate (eGFR) was obtained from the equation for Japanese patients, recently proposed by a working group of the Japanese Chronic Kidney Disease Initiative.13 Relationships between echocardiographic parameters and various clinical characteristics, including blood pressure, CAVI and laboratory data were analyzed. This protocol was approved by the Ethics Committee of Kagawa University. Informed consent was obtained from all participants.
Echocardiographic examination
Two-dimensional and M-mode echocardiography were performed using the Vivid Seven System (GE; Horten, Norway). We first measured the following left ventricular (LV) structural parameters by M-mode echocardiography: ventricular septal thickness (VS) at the chordae tendineae level, LV end-diastolic dimension (LVDd) and LV end-systolic dimension (LVDs) at the chordae tendineae level, LV posterior wall (PW) thickness at the chordae tendineae level, the end-systolic dimension of the left atrium (LAD) and the dimension of the ascending aorta (AO). The LV mass was calculated according to the American Society of Echocardiography convention14 using the following formula: LV mass=0.80 × 1.04 × [(PW+VS+LVDd)3–(LVDd)3]+0.6. The LV mass index (LVMI) was calculated as the LV mass divided by the body surface area. The LV ejection fraction (LVEF) was estimated by Teichholz's method15 and was used as the parameter of LV systolic function. In addition, we assessed the magnitude of aortic regurgitation (AR) by measuring the maximal area of the AR jet on color Doppler echocardiograms from the parasternal view. The maximal area of the AR jet was measured by tracing the jet area on a two-dimensional image when the largest jet during the diastolic phase was observed.
We next measured the parameters of LV diastolic function by recording the transmitral flow velocity using conventional Doppler echocardiography, which measures blood flow velocities in the cardiac cavity.16, 17 The transmitral flow velocity was recorded from the apical transducer position with the sample volume situated between the mitral leaflet tips. The peak velocity of early transmitral flow velocity (E velocity) and the peak velocity of late transmitral flow velocity (A velocity) were recorded, and the E/A ratio was calculated. The deceleration time of E velocity (DcT) was measured as the time interval from the E-wave peak to the decline of the velocity to baseline values.
In addition, we measured the Tei index, which reflects both systolic and diastolic functions of the LV.18 Details of the method for measuring the Tei index have been published by Tei et al.19 The Tei index, defined as the sum of the isovolumic contraction time and isovolumic relaxation time divided by the ejection time, was obtained from Doppler recordings of LV inflow and outflow. The Tei index is derived as (a–b)/b, where ‘a’ is the interval between the cessation and onset of mitral inflow and ‘b’ is the ejection time of LV outflow. In measuring ‘a’ and ‘b’, we confirmed that the preceding RR intervals were the same in each patient.
Furthermore, tissue Doppler echocardiography, which measures the velocities of the regional cardiac wall, was performed by activating the tissue Doppler echocardiographic function in the same machine. Mitral annular velocities were recorded from the apical window. Sample volumes were located at the septal site of the mitral annulus. Peak early diastolic mitral annular velocity (E′) and the ratio of E velocity to E′ velocity (E/E′) were measured and analyzed as parameters of LV diastolic function.20, 21 Furthermore, peak systolic mitral annular velocity (S′) was measured and was used as a parameter of LV systolic function.22, 23
Measurement of CAVI and CBP
All measurements were conducted in a quiet room kept at a constant temperature. CAVI was recorded using a VaseraVS-1000 vascular screening system (Fukuda Denshi, Tokyo, Japan) with the patient resting in a supine position just after the echocardiographic examination. CAVI is clinically used as a parameter reflecting the stiffness of arteries from the aortic valve to the ankle. The principal underlying CAVI has been described.24, 25 ECG electrodes were placed on both wrists, a microphone to detect heart sounds was placed on the sternum, and cuffs were wrapped around both arms and both ankles. After automatic measurements, the obtained data were analyzed using VSS-10 software (Fukuda Denshi), and the right and left CAVI values were calculated. The averages of the right and left CAVIs were used for analysis.
After the CAVI recording, the brachial blood pressure, CBP and the augmentation index were determined with the patient in the sitting position. The radial pulse wave was recorded by using automated applanation tonometry (HEM-9000AI, Omron Healthcare, Kyoto, Japan). Briefly, the device consists of three units: a sensor unit, a pulse measurement unit and a personal computer.8 The wristwatch-shaped sensor unit has a pressure sensor with an array of multiple 40-microtransducer elements on its inner surface. Once the sensor is placed on the left wrist over the radial artery, the device automatically flattens the artery, adjusts the applanation hold-down pressure, and selects an optimal sensing element to record the pulse wave appropriately. The obtained pressure signals are digitized at 500 Hz inside the pulse measurement unit and then transmitted to a personal computer. Continuous steady-state 40-s data were recorded for each patient. According to earlier studies,6, 9 the amplitude of the late systolic peak of the pulse waveform correlates with CBP. Thus, the CBP can be determined noninvasively by mathematically transforming the radial artery pulse waveform to the aortic pulse waveform. In addition, the augmentation index was calculated as the ratio of the amplitude of the late systolic peak to the amplitude of the early systolic peak. The augmentation index depends not only on systemic arterial elasticity but also on arterial geometry and tone.26, 27 In this study, the augmentation index was also used as a parameter reflecting arterial stiffness as well as CAVI. In addition, this machine can measure the brachial blood pressures simultaneously using the conventional cuff method. Thus, we calculated the difference between CBP and systolic brachial blood pressure (CBP—systolic brachial blood pressure) and used it as a parameter derived from the measurement of CBP for analysis.
Statistical analysis
Data are expressed as means±s.d. Statistical analysis was performed using the SPSS software package (SPSS, Chicago, IL, USA). Linear regression analysis was performed to evaluate the associations between CBP, CAVI and other variables. Stepwise multiple regression analysis was performed to determine the correlation between echocardiographic parameters and each independent variable. Values of P<0.05 were considered to indicate statistical significance. Differences in parameters among the three groups treated with different antihypertensive agents were compared by one-way analysis of variance, followed by Bonferroni's post hoc test.
Results
Clinical and echocardiographic characteristics of subjects
The clinical and echocardiographic parameters of the study subjects are summarized in Table 1. All patients were treated with at least one antihypertensive agent. The mean systolic brachial blood pressure of all subjects was not particularly high (138±18 mm Hg) because all patients' blood pressure was appropriately controlled by medication. The mean LVEF was 71±7%; all patients had normal systolic function (LVEF⩾55%). The elevated mean LVMI (117±39 g m−2) indicated the presence of LV hypertrophy in the subjects overall. In addition, the decreased mean E/A (0.75±0.18) and E′ (5.3±1.7 cm s−1) indicated LV diastolic dysfunction accompanying LV hypertrophy. The increased mean E/E′ (11.0±3.5) suggested an increase in left atrial pressure, which is a parameter of LV preload.20, 21 The increased Tei index suggested impaired LV diastolic function, because the LV systolic function was thought to be preserved for all patients.
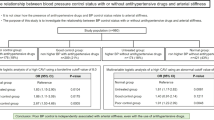
Association between CAVI and parameters derived from blood pressure measurement
Linear regression analysis was performed to examine the relationship between CAVI and other parameters derived from blood pressure measurement in all subjects (Table 2). The CAVI did not correlate with any parameters derived from blood pressure measurement. In contrast, CBP correlated with other parameters of blood pressure and showed the closest correlation with systolic brachial blood pressure (r=0.693, P<0.001). The difference between central and systolic brachial blood pressure correlated with other parameters of blood pressure, and showed the closest correlation with the augmentation index (r=0.868, P<0.001).
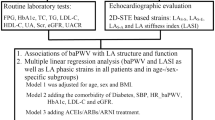
Comparison of CBP and CAVI in terms of their correlation with echocardiographic parameters
Linear regression analysis was performed to examine the relationships between CBP, CAVI and other variables in all subjects (Table 3). The period of hypertension treatment, smoking status, diabetes and dyslipidemia correlated with neither CAVI nor the blood pressure parameters. The systolic brachial blood pressure did not correlate with any parameters. Although CBP correlated with LVMI (r=0.306, P<0.01), CBP correlated only with the Tei index (r=0.201, P<0.05) among all echocardiographic LV functional parameters. The difference between central and systolic brachial blood pressures correlated with LVMI (r=0.212, P<0.05), S′ (r=−0.308, P<0.01), E′ (r=−0.195 P<0.05) and the Tei index (r=0.211, P<0.05). The augmentation index correlated with S′ (r=−0.276, P<0.01) and the Tei index (r=0.207, P<0.05). In contrast, the CAVI did not correlate with LVMI. However, the CAVI correlated with E/A (r=−0.387, P<0.001), S′ (r=−0.270, P<0.01), E′ (r=−0.362 P<0.01) and the Tei index (r=0.339, P<0.01), and these correlations were closer than those of the parameters derived from blood pressure measurement.
Assessment of the factors related to echocardiographic LV functional and morphological parameters
Stepwise multiple regression analysis was performed to identify which clinical and pulse wave-derived parameters were independently associated with echocardiographic LV functional and morphological parameters (S′, E′, Tei index and LVMI), which showed significant correlations with CBP and CAVI in linear regression analysis. Stepwise multiple regression analysis was performed for systolic brachial blood pressure, CBP, the difference between central and systolic brachial blood pressure, augmentation index, CAVI, age, heart rate, BMI, total cholesterol, HDL-C, triglyceride, HbA1c, hemoglobin, eGFR, LVMI, LAD, AO, AR, LVEF, E/A, DcT and E/E′; see Table 3. This analysis indicated that E′ (β coefficient=0.631, P<0.001) and AR (β coefficient=0.255, P=0.001) were independently associated with S′ (Table 4). E/E′ (β coefficient=−0.462, P<0.001), E/A (β coefficient=0.383, P<0.001) and S′ (β coefficient=0.272, P=0.001) were independently associated with E′ (Table 5). AR (β coefficient=0.605, P<0.001), LVEF (β coefficient=−0.375, P<0.001), CAVI (β coefficient=0.311, P<0.001) and augmentation index (β coefficient=0.177, P=0.006) were independently associated with the Tei index (Table 6). AO (β coefficient=0.330, P=0.001) and CBP (β coefficient=0.308, P=0.001) were independently associated with the LVMI (Table 7). Thus, among the pulse wave-derived parameters (systolic brachial blood pressure, CBP, difference between central and systolic brachial blood pressure, augmentation index and CAVI), CAVI and the augmentation index were independently associated with the Tei index. In contrast, only CBP was independently associated with LVMI.
Discussion
This study compares CBP and CAVI data to identify the associations between echocardiographic LV structural and functional parameters in treated hypertensive patients. The data led us to the following conclusions: (1) neither the CBP nor the augmentation index correlated with CAVI in patients with treated hypertension; (2) CBP, but not CAVI, correlated with LVMI in patients with treated hypertension and (3) CAVI showed closer correlations than CBP with LV functional parameters.
Our analysis suggests that although CBP may be superior to CAVI for reflecting LV hypertrophy, CAVI may be superior to CBP for reflecting LV functional parameters. Therefore, CBP may be suitable for detecting LV hypertrophy. In contrast, CAVI may be suitable for detecting LV dysfunction. This difference, suggesting the clinical value of each parameter, should be kept in mind when we use CBP and CAVI for assessing arteriosclerosis in hypertensive patients.
When we initiated this study, we expected that increased CBP would lead to dilation of the ascending aorta and AR in hypertensive patients, because CBP was thought to reflect a direct afterload of the left ventricle. However, in our results, neither CBP nor the augmentation index correlated with the diameter of the ascending aorta or the magnitude of AR. As the patients' blood pressure was under good control when this study was performed, decreased afterload of the left ventricle may have changed the magnitude of AR. However, the magnitude of AR was independently associated with the Tei index (Table 6). The magnitude of AR was mild for all patients in this study, and patients with more than moderate AR were excluded. Therefore, latent LV dysfunction that was detected by an increased Tei index may have been produced by hypertension rather than AR itself. As AR is hardly observed in normal subjects, this relationship between the Tei index and AR may be observed only in patients with treated hypertension.
In this study, S′ showed closer correlations than LVEF with CBP-SBP, AI and CAVI (Table 3). LVEF derived from M-mode echocardiography represents LV systolic function in the direction of the horizontal axis of heart. In contrast, S′ derived from tissue Doppler echocardiography represents longitudinal LV systolic function. Although both S′ and LVEF reflect LV systolic function, S′ may be more sensitive than LVEF for detecting latent LV dysfunction in treated hypertensive patients. As arterial stiffness assessed by CAVI reflects LV afterload, hypertensive patients with increased CAVI may be affected by increased LV afterload during cardiac systolic phase. This may be a reason why LV systolic functional parameters such as S′ and LVEF correlated inversely with CAVI (Table 3). Although an earlier study28 reported that LVEF did not correlate with CAVI, another earlier report reported that S′ correlated inversely with LV afterload assessed by tissue Doppler echocardiography.29 Further studies are needed to elucidate the relationships between LV systolic function and CAVI.
Our results can provide new information regarding how to use CBP in a clinical setting. In this study, the absolute value of CBP showed a correlation, albeit a weak one, only with Tei index among the LV functional parameters. However, the difference between central and systolic brachial blood pressure showed significantly closer correlations with the LV functional parameters. Therefore, LV diastolic dysfunction cannot be assessed by the absolute value of CBP. The difference between central and systolic brachial blood pressure may reflect LV dysfunction. The augmentation index, which correlates well with the difference between the central and systolic brachial blood pressure, may also reflect LV dysfunction. In any case, the parameters related to CBP may be inferior to CAVI in reflecting LV function. This finding may be attributed to the fact that CBP was measured only at the radial artery on the left side. In contrast, CAVI was measured on both sides and was thought to reflect the stiffness of long arteries from the aortic valve to the ankle. The difference in the extent of measured arteries may have led to the difference between CBP and CAVI in this study. This may be a reason why CAVI did not correlate with CBP or the augmentation index (Table 2). This is reasonable because CAVI is thought to be less influenced by blood pressure11, 12 compared with other pulse wave-derived parameters. However, an earlier study30 showed that the augmentation index reflected arterial stiffness and LV hypertrophy. Although CAVI and CBP differ to some degree, close correlations might be observed in other study populations. Further studies are needed to elucidate the associations between CAVI, CBP and the augmentation index.
When we assess the association between arteriosclerosis and LV function, the state of cardiac function of the study participants should be considered. In this study, the mean values of cardiothoracic ratio in chest radiograph, LV end-diastolic diameter, LVEF and LV mass index were 50±2.5%, 46±6 mm, 71±7% and 117±39 g m−2, respectively. The mean value of plasma brain natriuretic peptide level of the 63 patients for whom we were able to measure this value was 33.1±26.0 pg ml−1. The Tei index was 0.58±0.16. These data suggest that the patients of this study have mild LV hypertrophy without dilation of the LV cavity. The LV systolic function is preserved, and the increased Tei index may be mainly attributed to the LV diastolic dysfunction, which leads to the slightly increased plasma brain natriuretic peptide level. Therefore, other study populations with more severe LV dysfunction may yield different results from ours. Our data showed that CAVI has a correlation with only the Tei index among the parameters of LV function after stepwise regression analysis. However, earlier reports31, 32 suggest that brachial ankle pulse wave velocity has a correlation with several LV diastolic functional parameters such as E/A ratio, even after stepwise regression analysis. A recent report33 suggests that brachial ankle pulse wave velocity is an early indicator of LV dysfunction. Further studies are needed to assess the association between arteriosclerosis and LV function in study subjects with various degrees of LV dysfunction.
As antihypertensive agents that were administered to the patients may have affected the arteriosclerosis and LV function in this study, we compared the variables among three groups that were treated with angiotensin II receptor blocker alone (n=48), calcium channel blocker (CCB) alone (n=39) and both angiotensin II receptor blocker and CCB (n=15) (Table 8). No differences in parameters of arteriosclerosis and LV function were observed among the three groups. However, it is difficult to determine the drugs' effects in this study because of the small number of study subjects. Further studies with larger numbers of subjects treated with various antihypertensive agents are needed.
Among the LV functional parameters in this study, only the Tei index was independently associated with CAVI and the augmentation index. It is well known that aging has less influence on the Tei index than on LV functional parameters including E/A and E′.34 Actually, Tei index did not correlate with age (r=0.163, P=0.102) in this study. CAVI and the augmentation index correlated closely with age (Table 3). Therefore, only the Tei index among the LV functional parameters may have been independently associated with CAVI and the augmentation index. We cannot determine the precise mechanism by which LV function assessed by Tei index correlates with arterial stiffness assessed by CAVI. One possible explanation is that arterial and LV stiffening may be epiphenomena accompanied by aging and hypertension. Advanced glycation end products have been reported to deteriorate arterial stiffness and LV diastolic function by cross-linking long-lived proteins, such as collagen and elastin, and altering cellular responses in the tissue.35 The similarity of histological changes in the myocardium and arterial wall may contribute to the correlation between CAVI and LV function assessed by Tei index. Our data indicate that the Tei index may be more useful than other LV functional parameters for comparing cardiac function among hypertensive patients of various age strata. However, we examined the associations between CBP, CAVI and echocardiographic data in treated hypertensive patients whose blood pressure was well controlled. As treatment for hypertension may have improved cardiovascular structure and function, abnormalities that should have been detected by CBP may have been concealed in this study. Actually, CBP did not correlate with LV diastolic functional parameters, even though CBP correlated with LVMI. As treatment for hypertension may have improved LV diastolic function, LV diastolic dysfunction may have not been detected by CBP in this study. Further studies are needed to assess the clinical usefulness of CBP in untreated hypertensive patients or in patients with considerably high blood pressure. CAVI and AI had negative correlations with BMI when linear regression analysis was performed (Table 3) in this study. In this study, considerable old age participants (⩾80 years of age) with high values of CAVI and AI were thin hypertensive patients having low BMI values. This fact may be a reason why CAVI and AI had negative correlations with BMI. However, BMI was not selected as independent determinants of LV structural and functional parameters when stepwise multiple regression analysis was performed (Tables 4, 5, 6 and 7). Therefore, we consider that the characteristic of BMI of the participants had no influences on the conclusion of this study.
In conclusion, CBP may be suitable for detecting LV hypertrophy. In contrast, CAVI may be suitable for detecting LV dysfunction. This difference, suggesting the clinical value of each parameter, should be kept in mind when we use CBP and CAVI for assessing arteriosclerosis in treated hypertension.
References
Muratani H, Kimura Y, Fukiyama K, Kawano Y, Fujii J, Abe K, Kuwajima I, Ishii M, Shiomi T, Mikami H, Ibayashi S, Omae T . Control of blood pressure and lifestyle-related risk factors in elderly Japanese hypertensive subjects. Hypertens Res 2000; 23: 441–449.
Hata Y, Kimura Y, Muratani H, Fukiyama K, Kawano Y, Ashida T, Yokouchi M, Imai Y, Ozawa T, Fujii J, Omae T . Office blood pressure variability as a predictor of brain infarction in elderly hypertensive patients. Hypertens Res 2000; 23: 553–560.
Weber T, Auer J, O'Rourke MF, Kvas E, Lassnig E, Berent R, Eber B . Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation 2004; 109: 184–189.
Chirinos JA, Zambrano JP, Chakko S, Veerani A, Schob A, Willens HJ, Perez G, Mendez AJ . Aortic pressure augmentation predicts adverse cardiovascular events in patients with established coronary artery disease. Hypertension 2005; 45: 980–985.
Yaginuma T, Noda T, Tsuchiya M, Takazawa K, Tanaka H, Kotoda K, Hosoda S . Interaction of left ventricular contraction and aortic input impedance in experimental and clinical studies. Jpn Circ J 1985; 49: 206–214.
Takazawa K, Kobayashi H, Shindo N, Tanaka N, Yamashina A . Relationship between radial and central arterial pulse wave and evaluation of central aortic pressure using the radial arterial pulse wave. Hypertens Res 2007; 30: 219–228.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD, Thurston H, O'Rourke M . CAFE Investigators; Anglo-Scandinavian Cardiac Outcomes Trial Investigators; CAFE Steering Committee and Writing Committee. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation 2006; 113: 1213–1225.
Hashimoto J, Watabe D, Hatanaka R, Hanasawa T, Metoki H, Asayama K, Ohkubo T, Totsune K, Imai Y . Enhanced radial late systolic pressure augmentation in hypertensive patients with left ventricular hypertrophy. Am J Hypertens 2006; 19: 27–32.
Kohara K, Tabara Y, Tomita H, Nagai T, Igase M, Miki T . Clinical usefulness of the second peak of radial systolic blood pressure for estimation of aortic systolic blood pressure. J Hum Hypertens 2009; 23: 538–545.
Okura T, Watanabe S, Kurata M, Manabe S, Koresawa M, Irita J, Enomoto D, Miyoshi K, Fukuoka T, Higaki J . Relationship between cardio-ankle vascular index (CAVI) and carotid atherosclerosis in patients with essential hypertension. Hypertens Res 2007; 30: 335–340.
Takaki A, Ogawa H, Wakeyama T, Iwami T, Kimura M, Hadano Y, Matsuda S, Miyazaki Y, Hiratsuka A, Matsuzaki M . Cardio-ankle vascular index is superior to brachial-ankle pulse wave velocity as an index of arterial stiffness. Hypertens Res 2008; 31: 1347–1355.
Satoh N, Shimatsu A, Kato Y, Araki R, Koyama K, Okajima T, Tanabe M, Ooishi M, Kotani K, Ogawa Y . Evaluation of the cardio-ankle vascular index, a new indicator of arterial stiffness independent of blood pressure, in obesity and metabolic syndrome. Hypertens Res 2008; 31: 1921–1930.
Imai E, Horio M, Nitta K, Yamagata K, Iseki K, Hara S, Ura N, Kiyohara Y, Hirakata H, Watanabe T, Moriyama T, Ando Y, Inaguma D, Narita I, Iso H, Wakai K, Yasuda Y, Tsukamoto Y, Ito S, Makino H, Hishida A, Matsuo S . Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol 2007; 11: 41–50.
Wallerson DC, Devereux RB . Reproducibility of echocardiographic left ventricular measurements. Hypertension 1987; 9 (2 Pt 2): II6–II18.
Teichholz LE, Kreulen T, Herman MV, Gorlin R . Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am J Cardiol 1976; 37: 7–11.
Nishimura RA, Appleton CP . ‘Diastology’: beyond E and A. J Am Coll Cardiol 1996; 27: 372–374.
Nishimura RA, Tajik AJ . Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician's Rosetta Stone. J Am Coll Cardiol 1997; 30: 8–18.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB . New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 1995; 26: 357–366.
Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB . Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis. J Am Coll Cardiol 1996; 28: 658–664.
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW . Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 1997; 30: 474–480.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Redfield MM, Tajik AJ . Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 2000; 102: 1788–1794.
Mogelvang R, Sogaard P, Pedersen SA, Olsen NT, Schnohr P, Jensen JS . Tissue Doppler echocardiography in persons with hypertension, diabetes, or ischaemic heart disease: the Copenhagen City Heart Study. Eur Heart J 2009; 30: 731–739.
Lazar JM, Qureshi G, Qureshi MR, Smith E, Scharf B, Rosenblum LA, Signaevsky M, Kral JG, Salciccioli L . Left ventricular systolic and diastolic function in healthy adult Bonnet Macaques (Macaca radiata). New echocardiographic indices in old world monkeys. Cardiology 2008; 113: 116–121.
Yambe T, Yoshizawa M, Saijo Y, Yamaguchi T, Shibata M, Konno S, Nitta S, Kuwayama T . Brachio-ankle pulse wave velocity and cardio-ankle vascular index (CAVI). Biomed Pharmacother 2004; 58 (Suppl 1): S95–S98.
Shirai K, Utino J, Otsuka K, Takata M . A novel blood pressure-independent arterial wall stiffness parameter; cardio ankle vascular index (CAVI). J Atheroscler Thromb 2006; 13: 101–107.
Pannier BM, Avolio AP, Hoeks A, Mancia G, Takazawa K . Methods and devices for measuring arterial compliance in humans. Am J Hypertens 2002; 15: 743–753.
Davies JI, Struthers AD . Pulse wave analysis and pulse wave velocity: a critical review of their strengths and weaknesses. J Hypertens 2003; 21: 463–472.
Mizuguchi Y, Oishi Y, Tanaka H, Miyoshi H, Ishimoto T, Nagase N, Oki T . Arterial stiffness is associated with left ventricular diastolic function in patients with cardiovascular risk factors: early detection with the use of cardio-ankle vascular index and ultrasonic strain imaging. J Card Fail 2007; 13: 744–751.
Borlaug BA, Melenovsky V, Redfield MM, Kessler K, Chang HJ, Abraham TP, Kass DA . Impact of arterial load and loading sequence on left ventricular tissue velocities in humans. J Am Coll Cardiol 2007; 50: 1570–1577.
Hashimoto J, Nichols WW, O'Rourke MF, Imai Y . Association between wasted pressure effort and left ventricular hypertrophy in hypertension: influence of arterial wave reflection. Am J Hypertens 2008; 21: 329–333.
Nakae I, Matsuo S, Matsumoto T, Mitsunami K, Horie M . Augmentation index and pulse wave velocity as indicators of cardiovascular stiffness. Angiology 2008; 59: 421–426.
Masugata H, Senda S, Yoshikawa K, Yoshihara Y, Daikuhara H, Ayada Y, Matsushita H, Nakamura H, Taoka T, Kohno M . Relationships between echocardiographic findings, pulse wave velocity, and carotid atherosclerosis in type 2 diabetic patients. Hypertens Res 2005; 28: 965–971.
Wang CP, Hung WC, Yu TH, Hsu HL, Chen YH, Chiu CA, Lu LF, Chung FM, Cheng YA, Lee YJ . Brachial-ankle pulse wave velocity as an early indicator of left ventricular diastolic function among hypertensive subjects. Clin Exp Hypertens 2009; 31: 31–43.
Daimon M, Watanabe H, Abe Y, Hirata K, Hozumi T, Ishii K, Ito H, Iwakura K, Izumi C, Matsuzaki M, Minagoe S, Abe H, Murata K, Nakatani S, Negishi K, Yoshida K, Tanabe K, Tanaka N, Tokai K, Yoshikawa J . The JAMP Study Investigators. Normal values of echocardiographic parameters in relation to age in a healthy Japanese population. Circ J 2008; 72: 1859–1866.
Aronson D . Cross-linking of glycated collagen in the pathogenesis of arterial and myocardial stiffening of aging and diabetes. J Hypertens 2003; 21: 3–12.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Masugata, H., Senda, S., Okuyama, H. et al. Comparison of central blood pressure and cardio-ankle vascular index for association with cardiac function in treated hypertensive patients. Hypertens Res 32, 1136–1142 (2009). https://doi.org/10.1038/hr.2009.157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.157
Keywords
This article is cited by
-
Associations between measurements of central blood pressure and target organ damage in high-risk patients
Clinical Hypertension (2021)
-
Gender-specific association of serum uric acid levels and cardio-ankle vascular index in Chinese adults
Lipids in Health and Disease (2018)
-
Cardio-ankle vascular index and subclinical heart disease
Hypertension Research (2015)
-
Assessment of arterial stiffness in chronic obstructive pulmonary disease by a novel method
Herz (2014)
-
Association between arterial stiffness and pulmonary function in hypertensive patients
Hypertension Research (2012)