Summary:
The occurrence of toxic complications following hematopoietic stem cell transplantation (HSCT) is highly variable and dependent on a multitude of host, donor, and treatment factors. The increasingly broad indications for HSCT and the need to provide this treatment option to older and/or more debilitated patients emphasizes the importance of refining our methods of predicting and ameliorating these toxicities. Late complications (occurring after day 100) also pose a threat to quality of life after HSCT. Genetic polymorphisms in key molecular pathways in the host are likely to contribute significantly to the observed variability in the development HSCT-associated complications. Hepatic veno-occlusive disease and acute lung injury, two of the most serious organ toxicities that occur, represent useful paradigms for the identification of genetic polymorphisms in enzyme systems that modulate local and systemic responses to oxidant stress during transplant conditioning therapy. Ongoing studies in this area are providing clues to the prevention of adverse clinical outcomes based on the genetic milieu. This review of studies in HSCT that explore genetic risk factors for transplant complications indicates that significant progress is being made in this rapidly evolving area. However, further large-scale clinical and translational studies are needed before genomic screening can be widely used to individualize treatment.
Similar content being viewed by others
Main
Clinicians are continually challenged by the need to predict the responses of individual patients to potentially toxic treatments. The increasing promise of cure for patients who undergo hematopoietic stem cell transplantation (HSCT) for life-threatening disorders is overshadowed by the very real threat of short-term, often fatal, complications resulting from the transplant regimen and graft-versus-host disease (GVHD). However, significant variation is observed between similarly treated individuals in the development of complications. It is an appealing concept, therefore, and one to which many clinicians now subscribe, that a significant portion of this variability has a genetic basis. Identifying important genetic variables will allow for better prediction of HSCT-related outcomes, and in the process of identifying these susceptibilities, it may also be possible to gain sufficient knowledge of the underlying pathophysiology of these toxicities to develop targeted interventions.
This review will focus on genomic screening of the host for the prediction of specific complications, touching briefly on selected donor factors. Other rapidly evolving areas that are not covered include molecular genetic testing to predict graft failure and disease relapse after HSCT. The role of clinical and biochemical risk factors in the pre-transplant evaluation of HSCT candidates has also been reviewed recently in this journal.1
Importance of context-dependent genetic effects
The study of uncommon disease-associated mutations has been invaluable to our understanding of basic pathophysiology and to the development of rational treatment strategies for diseases such as chronic myelogenous leukemia, acute promyelocytic leukemia, sickle cell anemia, and metabolic disorders. These disorders result from genetic mutations that drastically alter or abolish the function of a key cellular protein. However, more common DNA variants, or polymorphisms (generally defined as >1% prevalence in a specific population), may have more subtle functional consequences. Single-nucleotide polymorphisms (SNPs) are by far the most prevalent type of variant in the human genome, occurring on average every several hundred bases, and they are amenable to high-throughput genotyping methods.2,3 Most SNPs have no known effect on gene function, but a proportion of them may alter the expression and/or biological activity of encoded proteins, contributing to variation in disease susceptibility and treatment toxicity. Since millions of SNPs have already been identified in the human genome, this phenotypic variation is most likely the result of interactions between SNPs at many different loci (genetic epistasis) and from context-dependent effects rather than single-gene effects.4
While the knowledge that genetic factors and environmental factors (context) interact is not new, the study of such interactions is in its infancy. The concept of environmentally determined genetic expression (EDGE) provides a framework for considering the combinations of exposures, genetic and environmental, that define the thresholds for expression of specific phenotypes in an individual (Figure 1).5 This concept is based on the following observations: (1) genetically encoded variations in expressed proteins have different effects in different environmental contexts; (2) a disease phenotype is determined by both the functional magnitude of the genetic change and the severity of the environmental change; (3) rare genetic disorders (eg inborn errors of metabolism) represent one extreme with little contribution from the environment, while massive environmental insults result in phenotypes independent of genetic variation; and (4) most diseases/phenotypes fall between these extremes. Exposure to high-dose chemotherapy is a significant insult that may unmask the effects of normally silent genetic polymorphisms, and HSCT is an ideal setting in which to study these effects.
Concept of EDGE. An inborn error of metabolism, such as complete deficiency of a critical enzyme, has catastrophic consequences, whereas mildly diminished enzyme levels may be clinically silent except under stress conditions (eg high-dose chemoradiotherapy). HSCT=hematopoietic stem cell transplantation; HVOD=hepatic veno-occlusive disease (modified with permission from Summar et al5).
Approaches to the identification of susceptibility genes in HSCT
Genetic modifiers in complex diseases have been identified using linkage analysis (combined with positional cloning), association studies, and recently, genome-wide and microarray-based studies in unrelated affected and unaffected individuals. Linkage analyses, historically favored by geneticists, are pedigree-based and therefore unhelpful in the study of phenotypes associated with sporadic exposures (eg HSCT). Association studies (case–control and cohort studies) are popular with investigators whose knowledge of the phenotype(s) under study suggests obvious hypotheses and candidate genes. The major criticism of association studies using this ‘candidate-gene approach’, however, has been their frequently inconsistent or nongeneralizable results due to poor selection of the study population, racial/ethnic and geographic factors that influence the genetic background on which modifier genes act, low statistical power, and linkage disequilibrium (the problem of distinguishing the effects of closely linked genes).2,6,7 Genome-wide approaches suffer from some of the same drawbacks but are considerably more time-efficient, less prone to bias, and capable of identifying novel genes. Their chief disadvantage is that in the absence of a priori hypotheses, the very large number of statistical tests performed makes it difficult to distinguish true associations from random effects.
Genetic and molecular epidemiologic studies in HSCT
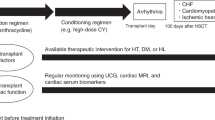
Complications occurring after HSCT may be divided into early, regimen-related organ toxicities such as hepatic veno-occlusive disease (HVOD), acute lung injury (ALI), and mucositis, and late complications that occur after post transplant day 100. Before considering the genes that have been associated with specific complications, it is instructive to review the role of oxidant stress in chemotherapy-related organ injury.
Oxidant stress is defined by the increased production of free radicals and other reactive oxygen/nitrogen species that damage cellular constituents.8 The chemoradiotherapy conditioning regimens used in HSCT represent a tremendous oxidant stress on vital organs, and their intensity is the principal determinant of both HVOD and ALI.9,10,11,12,13,14 Infection, accompanied by the release of inflammatory mediators, is a frequent contributor to oxidant stress in the post transplant period.15,16 Nonmyeloablative regimens are now widely used in allogeneic HSCT with a significantly lower risk of acute organ toxicity, but some patients still develop complications, and myeloablative conditioning may be preferable in certain hematological malignancies.17,18,19 Genetic polymorphisms in enzyme systems that normally constrain oxidant damage may partly explain the variation in the incidence and/or outcome of regimen-related complications.
Hepatic veno-occlusive disease and acute lung injury
The pathophysiology of HVOD (also called sinusoidal obstruction syndrome) involves microvascular obliteration resulting from injury to hepatic sinusoidal and venular endothelium and zone 3 hepatocytes.15 Nitric oxide (NO), a molecule with important roles as an antioxidant and in maintaining vascular patency, is produced in hepatocytes via the hepatic urea cycle exclusively (Figure 2). The hepatic urea cycle is the only nondietary source of arginine, the essential substrate for endothelial NO synthesis throughout the body. The enzyme carbamyl-phosphate synthetase I (CPSI) catalyzes the rate-limiting step of the urea cycle, thereby controlling the availability of NO precursors.20,21,22 A common SNP in the CPSI gene causes the substitution of asparagine (Asn) for threonine (Thr) at position 1405 (T1405N) in the critical cofactor-binding domain of the enzyme.23 Summar et al studied urea cycle function and the prevalence of this SNP in relation to HVOD, ALI, and oxidant stress in 200 patients undergoing myeloablative HSCT at Vanderbilt Medical Center. Both toxicities were strictly defined and determined prospectively, before genetic testing.15,24 In this cohort, citrulline levels fell by 57% (P<0.05) during conditioning chemotherapy, and ornithine/citrulline (O/C) ratios rose nearly four-fold (P<0.05), indicating impaired urea cycle function (Figure 2). Individuals with the Asn1405 variant of CPSI (encoded by the AA genotype) had significantly higher plasma levels of citrulline and NO metabolites at baseline (reflecting superior urea cycle function) than those with the Thr1405 variant (CC genotype). These data are consistent with in vitro studies of recombinant CPSI enzyme kinetics showing that the AA-encoded Asn1405 variant is 20–30% more efficient than the CC-encoded variant.5 The CPSI AA genotype was protective against HVOD and fatal lung injury after HSCT in the 195 patients analyzed (Table 1). These effects persisted after adjustment for other important risk factors (manuscript submitted). The antioxidant effects of NO may explain these findings, because plasma levels of 8-iso PGF2-isoprostanes, the most sensitive and specific measures of oxidant stress in vivo, were significantly higher in patients who developed HVOD and/or ALI and in those who died by post transplant day 60 than in patients who did not suffer from these complications (Figure 3).25 Consistent with these findings, the CPSI T1405N SNP appears to play a similar role in other phenotypes characterized by oxidant stress and vascular injury.21,26,27
The hepatic urea cycle. Urea cycle enzymes are localized to either the mitochondrial or cytoplasmic spaces. Dysfunction of either CPSI or OTC results in a fall in citrulline, a rise in ornithine levels, and potentially reduced NO production. CPSI=carbamyl-phosphate synthetase 1; OTC=ornithine transcarbamylase; ASS=arginosuccinate synthetase; ASL=arginosuccinate lyase; ARG=arginase; NOS=nitric oxide synthetase (modified with permission from Summar et al).21
Oxidant stress in HVOD, ALI, and early mortality after HSCT. After conditioning therapy, plasma 8-iso PGF2α (isoprostane) levels reach maximal levels during engraftment (measured at day 14). (a) Plasma isoprostane levels are significantly higher in patients who develop HVOD or ALI (b) and in nonsurvivors to day 60 (c) than in patients who do not have early complications (all P-values <0.05). BL=baseline.24
Nitric oxide is also a regulator of intracellular iron metabolism during inflammation.28 Iron augments oxidant liver injury.29 Homozygotes and heterozygotes for the common hemochromatosis (HFE) mutation C282Y have increased mean liver iron content and circulating levels of reactive iron.30,31 Another study in 166 patients from the same HSCT cohort found that HFE C282Y potentiates HVOD and that the CPSI SNP counterbalances this effect32,33 (manuscript submitted). Multivariable analysis adjusting for other risk factors showed a significantly increased risk of HVOD in the presence of one or two C282Y alleles (relative risk 3.7, 95% confidence interval 1.2–12.1). The risk of HVOD also increased progressively with the number of C282Y alleles present. A nonsignificant increase in day 60 mortality was noted in carriers of at least one HFE C282Y allele. A stratified analysis by CPSI genotype also showed that the CPSI A allele may reduce the impact of HFE C282Y on risk of HVOD in accord with its previously observed beneficial effect (Table 2). This study was limited primarily by the lack of quantitative data regarding iron stores in most patients, leaving unanswered the question of the mechanism of increased HVOD in carriers of HFE C282Y. However, carriage of one or two C282Y alleles was strongly associated with the need for vancomycin therapy during the conditioning phase (P<0.001), and pre transplant vancomycin therapy is a recognized HVOD risk factor.15 Controlling for vancomycin use abolished the effect of HFE C282Y on HVOD, suggesting that infection may in fact be on the causal pathway. Since the HFE gene is on chromosome 6, another HLA class I-linked gene could conceivably be responsible for the observed effects. The HFE C282Y allele had no detectable effect on the incidence of ALI in this cohort.
Glutathione (GSH) is perhaps the single most important cellular antioxidant in the liver and lungs, and considerable variation has been described in glutathione-metabolizing enzymes. A polymorphism in the GST gene that encodes glutathione S-transferase, which catalyzes the conjugation of busulfan and the active metabolite of cyclophosphamide to glutathione, has been reported to result in a significantly increased incidence of HVOD in thalassemic patients undergoing HSCT.34 Pharmacokinetic studies suggest that this effect is due either to depletion of reduced glutathione or toxicity of GSH-conjugated busulfan metabolites.
Lung injury frequently follows HVOD, and shares with it many important features (Figure 4).35,36,37 The final common pathway in ALI involves inflammatory cell activation, proteolytic enzyme and cytokine release, and damage to lung parenchyma, vascular endothelium, and airways. This sequence of events, combined with exuberant activation of the coagulation cascade and surfactant dysfunction, leads to reduced gas exchange. In mouse models, ALI is associated with enhanced expression of genes involved in oxidant stress and antioxidant responses, for example, antiproteases and extracellular matrix repair proteins. The expression of proteins involved in surfactant production is markedly reduced, whereas expression of procoagulant and antifibrinolytic proteins is consistently increased.38 Polymorphisms in the glutamate-L-cysteine ligase catalytic subunit gene (GCLC), which encodes the rate-limiting enzyme in glutathione synthesis, are potentially important in recovery from ALI, and studies to determine their functional importance are currently in progress at Vanderbilt39,40 (manuscript submitted). Other than these studies of HSCT-related lung injury conducted at our institution, a few studies of candidate genes in ALI have been conducted in the setting of sepsis, trauma, or lung transplantation, and in mouse models of allogeneic HSCT.41,42,43 These genes, and others that have been implicated in chronic obstructive pulmonary disease and pulmonary hypertension, deserve further study as potential modifiers of both acute and chronic pulmonary complications after HSCT.2,44,45 Polymorphisms in many of these genes, such as those encoding coagulation factors, matrix metalloproteinases, and inflammatory mediators, may also be relevant to HVOD.29,46,47,48 Functional classes of genes that may influence oxidant toxicities after HSCT are listed in Table 3.
Other early complications
Studies that have demonstrated associations between specific genetic variants and early complications of chemotherapy and HSCT are summarized in Table 4.
Mucositis: methylenetetrahydrofolate reductase polymorphisms and methotrexate toxicity
In HSCT, mucositis is largely due to the conditioning regimen, particularly regimens that incorporate total-body irradiation (TBI) and methotrexate (MTX) administration for acute GVHD (aGVHD) prophylaxis. The enzyme methylenetetrahydrofolate reductase (MTHFR), which catalyzes the reduction of 5,10-methyleneTHF to 5-methylTHF, provides the carbon donor for methionine synthesis and regulates folate metabolism. This enzyme is therefore critical for normal DNA synthesis, methylation, and repair.49 MTX inhibits MTHFR activity and independently inhibits DNA methylation. A common thermolabile polymorphism in the MTHFR gene, designated C677T, results in heterozygous (CT) or homozygous (TT) enzyme variants with significantly reduced activities when compared to the CC variant (30% in TT homozygotes). The frequencies of CT and TT genotypes in the HSCT population are estimated to be 43 and 10–12%, respectively. This SNP has been associated with increased oral mucositis and delayed platelet recovery in patients undergoing allogeneic HSCT for chronic myelogenous leukemia who received cyclophosphamide/TBI or busulfan/cyclophosphamide conditioning and MTX prophylaxis for GVHD.50 Controlling for other risk factors, patients with lower MTHFR activity and the TT genotype had significantly higher mean mucositis scores. These results were confirmed by Robien et al51 after excluding patients who required leucovorin rescue and adjusting for pre-transplant vitamin use. Whether the effect of genotype on mucositis is independent of MTX administration is unclear, however, since only patients receiving MTX were included in these studies, and approximately 10% of patients receiving the same regimens without MTX experience severe mucositis.52 Moreover, the relative risk for development of severe (grade III–IV) mucositis in patients with the TT genotype as compared to the CC genotype was not reported, and the effect of genotype was not stratified by vitamin use. Of two other smaller studies, one found no significant difference in mucositis severity or in engraftment times by MTHFR genotype, and the other study showed an association between the TT genotype and intolerance to MTX in leukemia patients.53,54 These associations need to be validated in larger prospective studies that incorporate assessment of pre-transplant nutritional status and the incidence of aGVHD across MTHFR genotypes before MTX dose adjustment based on MTHFR genotype can be recommended.
Acute graft-versus-host disease
Recent interest has focused on the role of killer immunoglobulin-like receptors (KIRs) present on NK cells and some T cells, in modulating lymphocyte responses and hence the risk of aGVHD after HSCT. Encoded by highly polymorphic genes in the leukocyte receptor cluster on chromosome 19, KIRs bind to class I HLA molecules that are expressed on most nucleated cells. Recipient cells that lack the appropriate HLA class I ligand fail to bind and inhibit KIR-expressing donor cells, becoming targets for donor NK and T-cell alloreactivity. Since NK cells also express activating KIRs, a delicate balance between activating and inhibitory stimuli on donor vs host NK and T cells seems to dictate whether graft rejection or GVHD predominates after HSCT. The natural ligands for activating KIRs are unknown. Binding of the HLA-C molecule to inhibitory KIRs is sensitive to a polymorphism in the HLA-C alpha-helix. Group 1 HLA-C molecules carry an asparagine residue at position 80 (encoded by the C1 allele), whereas group 2 molecules possess a lysine at this position (encoded by the C2 allele). Two studies reported a reduced incidence of aGVHD and improved overall survival in haploidentical and unrelated-donor HSCT when there was KIR incompatibility in the graft-versus-host direction (defined as the absence in the recipient of class I allele group(s) recognized by donor KIRs).55,56 In haploidentical transplants for high-risk acute myeloid leukemia, lower rates of graft failure, relapse, and surprisingly, a reduced incidence of severe aGVHD may contribute to improved survival.55 A third study showed conflicting results and no differences in survival or aGVHD between KIR-compatible and KIR-incompatible transplants.57 These studies, however, did not directly assess KIR/HLA genotypes in donors and recipients and instead used a variety of methods to infer them.58 A more recent genetic study by Gagne et al59 did show that donor–recipient KIR genotype combinations are important determinants of aGVHD in both sibling and unrelated-donor HSCT. Cook et al58 further demonstrated by donor/recipient KIR genotyping that the HLA-C group of the recipient is also a major factor in determining outcome in HLA-identical sibling-donor HSCT if the recipient has a myeloid leukemia. Patients homozygous for the group 2 HLA-C allele (C2) who by definition lack the C1 allele (ligands for an inhibitory KIR) had reduced overall survival when compared with recipients who possessed at least one C1 allele (31.6 vs 56.1% at 4 years, respectively, P<0.005). This difference in survival was only significant when the donor also had the activating KIR2DS2 genotype; in this case, unopposed donor alloreactivity might occur even in the absence of HLA mismatch. No significant differences in the rates of aGVHD higher than grade II or in causes of mortality were noted between recipient C1/donor KIR combinations, and method of GVHD prophylaxis had no effect on outcome. The preponderance of evidence therefore suggests that KIR ligand incompatibility is a favorable factor in HLA-mismatched, unrelated-donor HSCT and HLA-identical sibling HSCT for myeloid leukemias (Table 4). Further studies are needed to clarify these effects in different HSCT scenarios. Independent of HLA matching, KIR and HLA-C genotyping of donor–recipient pairs may prove to be helpful in prioritizing HSCT among treatment options, in selecting donors, and in predicting clinical outcome in sibling- and unrelated-donor HSCT.
Given the role of cytokines in inflammation and tissue damage, prominent features of the graft-versus-host response, it is not surprising that a growing body of research has uncovered cytokine gene polymorphisms that affect cytokine levels during stress and hence outcomes after allogeneic HSCT. Lin et al60 analyzed SNPs in several cytokine genes (interleukin-1β, interleukin-1-receptor antagonist, interleukin-6, interleukin-10 and tumor necrosis factor-α) in allogeneic HSCT recipients and their HLA-identical sibling donors in relation to the risk of aGVHD. Homozygosity for an SNP in the IL-10 promoter region (−592 AA genotype) in the recipient was protective against grade III–IV aGVHD (hazard ratio 0.4, 95% CI 0.2–0.9, P=0.02) and death in remission (hazard ratio 0.6, 95% CI 0.3–1.0) compared with the CC genotype. Intermediate risks of aGVHD and death in remission were observed in AC heterozygotes. All patients received the same GVHD prophylaxis, and the analysis of GVHD was controlled for age at HSCT, sex of the donor–recipient pair, use of TBI, year of transplant, and diagnosis. Probability of overall survival at 3 years, adjusted for age at HSCT, duration of disease, and diagnosis, similarly correlated with genotype (71, 56, and 57% for AA, AC, and CC genotypes, respectively). The incidence of chronic GVHD (cGVHD) was unaffected. Although IL-10 levels were not measured in this study, correlations between genetic variants in the promoter region, higher IL-10 levels, and reduced aGVHD have been demonstrated in other smaller studies.61,62,63,64,65 Indeed, higher levels of IL-10 produced by antigen-presenting cells in the host may induce greater tolerance in donor T lymphocytes to alloantigens expressed on host cells. Variations in the other cytokine genes tested in either the donor or the recipient have not shown these associations with outcome. Since clusters of SNPs in the IL-10 promoter region (haplotypes) are in linkage disequilibrium (ie there is a nonrandom distribution of individual SNPs within these clusters in the population), individual IL-10 promoter haplotypes have been investigated. Since the beneficial effect on GVHD and survival was tied to the T-C-A-T-A haplotype defined by five SNPs, including the one at position −592, it is unclear whether the −592A allele or the entire haplotype is responsible for this effect.60 A higher frequency of the −592A allele in some Asian populations (67% in Japanese) as compared to Caucasian populations (24%) may account for lower incidence and severity of aGVHD in the Japanese and for differences between other racial/ethnic groups. Knowledge of the recipient's IL-10 promoter-region genotype would substantially inform the pre-transplant risk assessment, prioritization of HSCT among the available treatment options, and selection of conditioning regimens to minimize the risk of severe aGVHD in individual patients.
Some studies suggest that recipient SNPs in the TNF-α gene (putative high-producer TNF d3 and d4 alleles) and IFN-γ gene may also predict moderate to severe aGVHD in HLA-matched sibling HSCT, but some data are inconsistent.61,62,65,66,67 Weak associations with aGVHD are reported for other IL-10 microsatellite promoter-region SNPs (−1082, −1064, −3575 genotypes), but these effects are difficult to distinguish from those of the −592 SNP or the entire IL-10 haplotype, as previously mentioned. Since TNF-α and HLA haplotypes are tightly linked, the effects of TNF-α polymorphisms are also difficult to resolve from those of other immune response genes. Furthermore, these effects appear to be confined to HLA-identical sibling HSCTs. One study that was unable to show an effect of SNPs in the IL-10 gene may have been underpowered due to a large proportion of unrelated-donor transplants.66
Studies of polymorphisms in genes encoding the adhesion molecules PECAM-1 and CD31 in relation to aGVHD have also been conflicting.67
Susceptibility to infection
Polymorphisms in several genes involved in host defense and the inflammatory response have been investigated in relation to the risk of infection in immunocompromised populations (Table 4).68,69,70 These genes include TNF-α, TNF-β, IL-1β receptor antagonist, IL-6, IL-10, adhesion molecules, myeloperoxidase, Fc-γ receptors, mannose-binding lectin, and toll-like receptor genes. One study documented independent associations of both donor and recipient polymorphisms in the mannose-binding lectin gene MBL2 (coding and promoter regions) and risk of major infection after allogeneic HSCT.69 The time to neutrophil recovery, number of febrile days, incidence and severity of GVHD, and incidence of clinically significant, culture-confirmed infections were monitored in 97 HSCT recipients who received standard supportive care and GVHD prophylaxis. The MBL protein participates in the innate immune response by binding to carbohydrate moieties on microbial pathogens, leading to their opsonization and phagocytosis. Low, intermediate, and high MBL levels correlated with specific MBL2 haplotypes defined by several combinations of coding and promoter-region SNPs. There were no associations with GVHD overall, neutrophil recovery, length of hospitalization, early death, or duration of neutropenic fever, but a nonsignificant trend toward more febrile days was observed in donor–recipient pairs with MBL2 mutations. Replacement with purified MBL has been found to be safe and may be beneficial in MBL-deficient patients.71,72
Late complications
Chronic graft-versus-host disease
Although cGVHD is largely predicted by the occurrence of aGVHD, the results of genetic studies in this area have been discordant. Polymorphisms in TNF-α and IL-10 genes that associate with aGVHD have not generally been reported to predict cGVHD, with rare exceptions.68 However, the IL-6−174 G allele, which correlates with lower in vitro and in vivo IL-6 production, leads to a dose-dependent increase in risk of cGVHD (highest risk with homozygosity for the G allele). After adjustment for other risk factors, homozygosity for the promoter-region IL-6−174GG genotype does not predict increased aGVHD, but it is significantly associated with incident cGVHD.73 These discrepancies may be due to different effects of proinflammatory cytokines at different stages in the evolution of aGVHD and cGVHD and warrant further study.
Chronic renal failure
Damage to the renal microvasculature and parenchyma due to the preparatory regimen, aggravated by the use of nephrotoxic medications and in some cases, by sepsis, is implicated in the pathophysiology of chronic renal failure occurring after HSCT. Angiotensin-converting enzyme (ACE) inhibitors have proven effective in preventing and treating this syndrome in animal models, and an association between decline of renal function in patients after HSCT and polymorphisms within the ACE gene has been reported.74 The ACE gene encodes the enzyme responsible for cleaving angiotensin I to angiotensin II, which in turn has important effects on vascular tone, growth, and remodeling. A common polymorphism in the ACE gene, identified in 1990, is based on the insertion (I allele) or deletion (D allele) of a 287-base-pair intron. Individuals homozygous for the D allele have consistently (∼60%) higher plasma ACE activity, and progressively decreasing amounts of immunoreactive ACE are associated with the other two genotypes, DI and II, respectively.75 The DD genotype has also been associated with more rapid progression and increased severity of diabetic nephropathy, another form of renal disease in which oxidant injury is implicated. Juckett et al examined the effects of ACE genotype and other factors in a cohort of adult recipients of allogeneic HSCT between 1985 and 1996. Patients surviving at least 1 year and whose renal function was assessed for up to 3 years post transplant were studied. The strength of this study was that all patients received T-cell-depleted grafts, aGVHD prophylaxis with cyclosporine, and the same conditioning regimen. Independent of renal shielding and other clinical factors, the DD genotype predicted a slower decline in creatinine clearance during the year following transplant than the II genotype (P=0.040 for a difference in slope of 1.13 ml/min/month). Importantly, ACE genotype did not affect survival over the course of the study, and genotype distribution was in Hardy–Weinberg equilibrium. The preservation of renal function in HSCT patients with the DD genotype contrasts with studies in patients with diabetic nephropathy, in whom the II genotype tends to be protective and correlates with improved response to ACE inhibition. It is speculated that the deleterious remodeling effects of angiotensin on the kidney in other chronic renal diseases may be offset in HSCT patients by other protective effects of ACE involving tissue repair, free-radical scavenging, responses to nephrotoxic medications, etc.76 The use of ACE inhibitors is beneficial in animal models of BMT nephropathy and in transplant patients with nephropathy, however, and the reasons for this are unclear. Activation of the renin–angiotensin-activating system may initially preserve renal perfusion during hypotensive episodes but later contribute to progression of radiation-induced renal injury, which is amenable to ACE inhibition. Selection bias was a concern in this study, because only a fraction of the eligible patients survived to participate, had adequate follow-up data, and conditioning was not standard.74 Doses of TBI were higher than those used than at most centers, and the development of renal failure in patients who receive 12 Gy TBI or less, with or without renal shielding, may be less dependent on ACE genotype. Furthermore, ACE inhibitors are widely used to treat hypertension after HSCT, and this study did not control for the use of ACE inhibitors. Therefore, the significance of polymorphisms in the ACE gene in chronic renal failure developing after HSCT remains unclear.
Future directions
Genetic predisposition to other organ toxicities in the HSCT setting remains unexplored, including hemorrhagic cystitis and the bronchiolitis obliterans syndrome (BOS). Numerous studies of chronic obstructive pulmonary disease in animal models and in humans have identified genes that modulate the inflammatory response in the lung to oxidant insults, promoting damage to the airways and lung parenchyma.2 These include the matrix metalloproteinases (MMP1, MMP9, and MMP12), heme oxygenase-1, and α-1-antitrypsin genes. Similarly, polymorphisms in IL-6 and IFN-γ genes that regulate the production of these cytokines have been shown to correlate with the development of BOS after lung transplantation, consistent with a proinflammatory role for IL-6 in the pathogenesis of this disease.77 The role of these genes in both early and late pulmonary complications of HSCT setting should be evaluated. Polymorphisms that increase the risk of cGVHD might also be expected to increase the incidence of BOS.78
Common variations in the genes encoding drug-metabolizing enzymes, drug receptors, and drug transporters may give rise to individual variability in the toxicity of chemotherapeutic drugs.79 The role of genetic polymorphisms in the cytochrome P-450 enzyme system in the liver in transplant toxicity has not been sufficiently explored.80,81
Larger cohort studies are needed to confirm the associations that have been observed between specific genetic variants and HSCT-related complications and to identify other genes that modify risk. The benefits of these studies to patients are obvious: the potential for improved risk stratification and development of more effective interventions that target high-risk individuals. The value of oral supplementation with citrulline, bypassing CPSI in the generation of NO precursors, is currently being tested prospectively in a randomized, placebo-controlled trial in patients undergoing myeloablative HSCT at our institution. If supplementation is effective, it will constitute a significant addition to our armamentarium in supporting these critically ill patients.
Adverse effects of iron
There is growing evidence that elevated iron stores are detrimental to organ function in patients undergoing HSCT.82,83,84,85,86,87,88,89 Iron present in excess amounts or in reactive forms is a potent pro-oxidant and probably a radiosensitizing agent, because it can rapidly generate highly toxic free radicals in vivo (Figure 5).8,90,91,92 Iron overload is common in this population due to red cell transfusion and/or dyserythropoiesis.93,94,95 Prevalent iron-loading genetic mutations such as HFE C282Y may also augment organ toxicity (eg HVOD) by promoting infection, increasing reactive iron levels, and/or impairing the re-uptake of iron that is released during myeloablation.32,96,97,98,99,100,101,102,103 These mutations may also predispose HSCT survivors to secondary myelodysplasia and other malignancies.104,105,106,107,108,109 The effects of iron in the HSCT setting deserve further investigation, since they contribute to long-term morbidity and are potentially modifiable by antioxidant therapy, phlebotomy, and chelation.110,111,112,113,114
Autoimmune disease and heritable malignancy
The risk of transmission of genetic disease from donor to host is neither well recognized nor routinely considered during screening of potential HSCT donors. The urgency of finding suitable HLA-matched donors for the treatment of life-threatening diseases has taken precedence over such concerns, but this may change as the donor pool grows. Case reports in allogeneic transplant recipients have suggested that the adoptive transfer of autoimmune diseases such as vitiligo, thyroid disease, psoriasis, and even fulminant inflammatory bowel disease, may occur.115 Currently, however, there is no donor screening based on a positive personal or family history of autoimmune disease. Heritable cancer syndromes also constitute an important category of potentially transmissible genetic disease, and the absence of a positive family history in the donor is unhelpful. Genetic disorders associated with an increased risk of hematopoietic malignancy that are relatively common include Down's syndrome, Noonan's syndrome, and type 1 neurofibromatosis.116 Furthermore, the prevalence of mutations underlying many autosomal recessive genetic diseases (eg ataxia-telangiectasia, Fanconi's anemia, hereditary hemochromatosis), if not the prevalence of the diseases themselves, is higher than was reported before genetic testing became available. Carriers of these mutations may be at increased risk of leukemia and other malignancies. For most such genetic disorders, however, the nature and magnitude of the risk to recipients remain poorly defined. Clinical factors that increase the risk of aGVHD have been associated with secondary malignancies after HSCT, but whether this correlation extends to genetic risk factors for aGVHD is unknown.
Use of DNA microarray technology
Microarray technology employs immobilized DNA probes to detect complementary gene sequences and may be used to analyze the expression patterns of thousands of genes simultaneously. Genome-wide analyses and functional genomic approaches that evaluate the expression of sets of related genes can provide insights into the genetic basis of HSCT-related toxicities. In this context, the SNP profiles obtained from microarrays can provide clues to the molecular pathways involved in the development of specific complications. Ultimately, they might be used for individual risk stratification and treatment planning. Microarrays may be prone to inconsistent results, however.117 At present, both the statistical tools to handle large genetic studies and our understanding of proteomics lag significantly behind our ability to generate complex genetic data. At present, microarray technology may be most valuable as a tool to validate and refine (eg using multiplexed PCR assays) small, predictive panels of genes that are initially identified by other means.117,118
Translational studies
The EDGE model, while clearly an oversimplification of gene–environment interactions, illustrates for the CPSI gene example the value of moving beyond simple genetic association studies to relate qualitative and quantitative genetic changes to observed pathophysiology. This may involve a combination of in vivo and in vitro studies, as in the case of CPSI. Whereas common functional polymorphisms in CPSI that decrease urea cycle efficiency may be clinically silent under normal conditions, a shortage of NO substrates during the stress of HSCT may result in a deficiency of NO, thereby promoting severe oxidant damage in susceptible tissues (eg liver and lungs). The genetic axis for many disease states (eg the toxicities of HSCT) will consist of several genetic modifiers, such as polymorphisms in CPSI, MTHFR, GST and the major HFE locus. The different functional forms of each gene product will further subdivide this axis. Indeed, the complexity of this model for many phenotypes will require not just larger study populations but also increasingly sophisticated probabilistic models. Conventional logistic regression and multiple linear regression models rapidly lose power in multilocus studies due to empty cells, and they may often miss significant gene–gene or gene–environment effects. Newer, evolving statistical tools, such as multifactor dimensionality reduction (MDR), may provide better modeling of these complex interactions.119,120
It is premature to recommend changes in treatment for patients based on the results of genetic tests that need further validation of their utility in the clinical arena. Given the weight of evidence favoring some genotype–phenotype associations, however, fine-tuning of care might begin with testing for common polymorphisms in patients who are already at high risk of complications based on other criteria. Genetic polymorphisms (eg MTHFR, MBL2, CPSI, HFE) for which potential interventions exist are listed in Table 5. Protein or enzyme levels correlate well in some cases with genotype, and direct measurement of these levels rather than genotyping may be more readily performed (eg MBL2). Since the benefits of supportive interventions during HSCT such as oral or parenteral glutamine, citrulline, and chelation to reduce the iron load are currently unclear, their use in the context of genetic testing should be studied on formal protocols.
Conclusion
There are relatively few published studies that investigate host genetic susceptibilities in the development of common organ toxicities after HSCT, probably due to the difficulty of studying toxicities for which the underlying pathophysiologic mechanisms are not well defined. We have also learned from the literature concerning clinical predictive factors in HSCT that differences in patient selection, treatment regimens, supportive care, and definitions of toxicity between transplant centers may make it hard to interpret and generalize the results of single-center studies.
The compensatory response to oxidant stress is a useful example of the candidate-gene approach to complications of HSCT that should be exploited further. As the studies reviewed here illustrate, mutations that cause uncommon diseases may, at lower ‘allele dosages’ (eg heterozygosity for the CPSI T1405N or the HFE C282Y mutation), display important phenotypes under stress conditions. Varying degrees of functional CPSI deficiency, for example, give rise to phenotypes ranging from overwhelming hyperammonemia in the newborn period (complete CPSI deficiency) to marginal urea cycle reserve that is unmasked in the context of high-dose chemoradiotherapy (diminished CPSI efficiency).
Finally, due to the likelihood that combinations of SNPs comprising individual haplotypes, rather than individual SNPs, hold the key to understanding genetically determined variability in risk, and due to the statistical limitations of multilocus genetic analyses, large-scale and carefully designed studies are needed to address these issues. Currently, the only solution to the problems with gene–disease association studies is to prospectively validate multivariable predictive models that are generated from these studies in independent patient cohorts. An important first step is for transplant clinicians to recognize this new opportunity for clinical investigation and to initiate multicenter collaborations to develop large clinical/DNA databases for such studies. Haplotype- or SNP-based analyses in patients with well-characterized responses (phenotypes) to standardized regimens, including patients who participate in cooperative-group trials, may ultimately enable investigators to identify panels of genes that modulate responses to and toxicity from chemotherapy and determine the risk of specific complications. To be successful, these efforts will require interdisciplinary collaboration among transplant clinicians, molecular epidemiologists, statistical geneticists, and informatics specialists, a novel paradigm in clinical research. Further research to identify at-risk genetic haplotypes will enable clinicians to predict with far greater accuracy than before the likelihood of complications from HSCT and to individualize treatment approaches. As in other areas of clinical medicine in which genetic studies are gaining momentum, the expectation is that an individualized approach to HSCT that incorporates genetic data will ultimately lead to reduced transplant toxicity, reduced cost of care, and improved outcomes.
References
Bolwell BJ . Are predictive factors clinically useful in bone marrow transplantation? Bone Marrow Transplant 2003; 32: 853–861.
Wallace AM, Sandford AJ . Genetic polymorphisms of matrix metalloproteinases: Functional importance in the development of chronic obstructive pulmonary disease? Am J Pharmacogenomics 2002; 2: 167–175.
Ghosh S, Collins FS . The geneticist's approach to complex disease. Annu Rev Med 1996; 47: 333–353.
Rannala B . Finding genes influencing susceptibility to complex diseases in the post-genome era. Am J Pharmacogenomics 2001; 1: 203–221.
Summar ML, Hall L, Christman B et al. Environmentally determined genetic expression: clinical correlates with molecular variants of carbamyl phosphate synthetase I. Mol Genet Metab 2004; 81: S12–S19.
Little J, Bradley L, Bray MS et al. Reporting, appraising, and integrating data on genotype prevalence and gene–disease associations. Am J Epidemiol 2002; 156: 300–310.
Hirschhorn JN, Lohmueller K, Byrne E, Hirschhorn K . A comprehensive review of genetic association studies. Genet Med 2002; 4: 45–61.
Symons MCR, Gutteridge JMC . Free Radicals and Iron: Chemistry, Biology and Medicine. Oxford University Press Inc.: New York, 1998.
De Leve LD . Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease). Semin Liver Dis 2002; 22: 27–42.
McDonald GB, Slattery JT, Bouvier ME et al. Cyclophosphamide metabolism, liver toxicity, and mortality following hematopoietic stem cell transplantation. Blood 2003; 101: 2043–2048.
Umegaki K, Sugisawa A, Shin SJ et al. Different onsets of oxidative damage to DNA and lipids in bone marrow and liver in rats given total body irradiation. Free Radic Biol Med 2001; 31: 1066–1074.
Cooke KR, Yanik G . Acute lung injury after allogeneic stem cell transplantation: is the lung a target of acute graft-versus-host disease? Bone Marrow Transplant 2004, in press (Epub ahead of print).
Blackwell TS, Christman JW, Hagan T et al. Oxidative stress and NF-kappaB activation: correlation in patients following allogeneic bone marrow transplantation. Antioxid Redox Signal 2000; 2: 93–102.
Dürken M, Agbenu J, Finckh B et al. Deteriorating free radical-trapping capacity and antioxidant status in plasma during bone marrow transplantation. Bone Marrow Transplant 1995; 15: 757–762.
Kumar S, DeLeve LD, Kamath PS, Tefferi A . Hepatic veno-occlusive disease (sinusoidal obstruction syndrome) after hematopoietic stem cell transplantation. Mayo Clin Proc 2003; 78: 589–598.
Coppell JA, Brown SA, Perry DJ . Veno-occlusive disease: cytokines, genetics and haemostasis. Blood Rev 2003; 17: 63–70.
Djulbegovic B, Seidenfeld J, Bonnell C, Kumar A . Nonmyeloablative allogeneic stem-cell transplantation for hematological malignancies: a systematic review. Cancer Control 2003; 10: 17–41.
Anagnastopoulos A, Aleman A, Giralt S . Nonmyeloablative reduced-intensity transplantation in multiple myeloma. Semin Oncol 2004; 31: 33–36.
Sloand E, Childs RW, Solomon S et al. Graft versus leukaemia. The graft-versus-leukemia effect of nonmyeloablative stem cell allografts may not be sufficient to cure chronic myelogenous leukemia. Bone Marrow Transplant 2003; 32: 897–901.
Moncada S, Higgs A . The L-arginine–nitric oxide pathway. N Engl J Med 1993; 329: 2002–2012.
Pearson DL, Dawling S, Walsh WF et al. Neonatal pulmonary hypertension. Urea cycle intermediates, nitric oxide production, and carbamoyl-phosphate synthetase function. N Engl J Med 2001; 344: 1832–1838.
Jackson MJ, Beaudet AL, O'Brien WE . Mammalian urea cycle enzymes. Annu Rev Genet 1986; 20: 431–464.
Summar ML, Hall LD, Eeds AM et al. Characterization of genomic structure and polymorphisms in the human carbamyl phosphate synthetase I gene. Gene 2003; 311: 51–57.
Summar ML, Scott N, Cummings E et al. Analysis of 200 patients undergoing bone marrow transplant shows allelic disequilibrium between drug related toxicity and a common exonic polymorphism in the CPSI gene and correlates with disruption of urea cycle intermediates. Am J Hum Genet 1999; 65 (Suppl.): A25.
Roberts LJ, Morrow JD . Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic Biol Med 2000; 28: 505–513.
Barr FE, Beverley K, VanHook E et al. Effect of cardiopulmonary bypass on urea cycle intermediates and nitric oxide levels after congenital heart surgery. J Pediatr 2003; 142: 26–30.
Summar ML, Gainer JV, Pretorius M et al. Relationship between carbamoyl-phosphate synthetase genotype and systemic vascular function. Hypertension 2004; 43: 186–191.
Kim S, Ponka P . Role of nitric oxide in cellular iron metabolism. Biometals 2003; 16: 125–135.
Pietrangelo A . Iron, oxidative stress and liver fibrogenesis. J Hepatol 1998; 28 (Suppl. 1): 8–13.
Bulaj ZJ, Griffen LM, Jorde LB et al. Clinical and biochemical abnormalities in people heterozygous for hemochromatosis. N Engl J Med 1996; 335: 1799–1805.
De Valk B, Addicks MA, Gosriwatana I et al. Non-transferrin-bound iron is present in serum of hereditary haemochromatosis heterozygotes. Eur J Clin Invest 2000; 30: 248–251.
Kallianpur AR, Hall LD, Yadav M et al. The hemochromatosis (HFE) C282Y allele and complications of hematopoietic cell transplantation. Blood 2003; 194a: A677.
Kallianpur AR, Hall LD, Yadav M et al. Hepatic veno-occlusive disease (HVOD) after high-dose chemotherapy and blood cell transplant (BCT): association with the major hemochromatosis (HFE) mutation C282Y and modification by polymorphisms of the hepatic urea cycle enzyme, carbamyl-phosphate synthetase 1 (CPS-1). Am J Hum Genet 2002; 7: 414 (A1424).
Srivastava A, Poonkuzhali B, Shaji RV et al. Glutathione S-transferase M1 polymorphisms: a risk factor or hepatic veno-occlusive disease in bone marrow transplantation. Blood 2004; 104: 15747 Epub 2004 May 13.
Wingard JR, Mellits ED, Jones RJ et al. Association of hepatic veno-occlusive disease with interstitial pneumonitis in bone marrow transplant recipients. Bone Marrow Transplant 1989; 4: 685–689.
Rubenfeld GD, Crawford SW . Withdrawing life support from mechanically ventilated recipients of bone marrow transplants; a case for evidence-based guidelines (see comments). Ann Intern Med 1996; 125: 625–633.
Matuschak GM, Tinaldo JE . Organ interactions in the adult respiratory distress syndrome during sepsis. Role of the liver in host defense. Chest 1988; 94: 400–406.
Leikauf GD, McDowell SA, Wesselkamper SC et al. Acute lung injury: functional genomics and genetic susceptibility. Chest 2002; 121: 70S–75S.
Willis AS, Freeman ML, Summar SR et al. Ethnic diversity in a critical gene responsible for glutathione synthesis. Free Radic Biol Med 2003; 34: 72–76.
Kallianpur AR, Willis AS, Christman BW et al. Short-term survival following high-dose chemotherapy and bone marrow transplant and association with a triplet repeat in the glutamate-cysteine ligase catalytic subunit gene. Am J Hum Genet 2003; 73: 176 (A71).
Russell JA . Genetics of coagulation factors in acute lung injury. Crit Care Med 2003; 31: S243–S247.
Wunderink RG, Waterer GW . Genetics of sepsis and pneumonia. Curr Opin Crit Care 2003; 9: 384–389.
Hildebrandt GC, Duffner UA, Olkiewicz KM et al. A critical role for CCR2/MCP-1 interactions in the development of idiopathic pneumonia syndrome after allogeneic bone marrow transplantation. Blood 2004; 103: 2417–2426.
Marcos E, Fadel E, Sanchez O et al. Serotonin-induced smooth muscle hyperplasia in various forms of human pulmonary hypertension. Circ Res 2004; 94: 1263–1270.
Runo JR, Vnencak-Jones CL, Prince M et al. Pulmonary veno-occlusive disease caused by an inherited mutation in bone morphogenetic protein receptor II. Am J Respir Crit Care Med 2003; 167: 889–894.
Ertem M, Akar N . Factor V Leiden mutation as a predisposing factor for veno-occlusive disease following BMT. Bone Marrow Transplant 2000; 25: 1110–1111 (Letter).
Duggan C, Schmidt M, Lawler M et al. The prothrombin gene variant G20210A but not factor V Leiden may be associated with veno-occlusive disease following BMT. Bone Marrow Transplant 1999; 24: 693–694 (Letter).
Hildebrandt GC, Olkiewicz KM, Corrion LA et al. Donor-derived TNF-{alpha} regulates pulmonary chemokine expression and the development of idiopathic pneumonia syndrome after allogeneic bone marrow transplantation. Blood 2004; 104: 586–593.
Toffoli G, Russo A, Innocenti F et al. Effect of methylenetetrahydrofolate reductase 677C*T polymorphism on toxicity and homocysteine plasma level after chronic methotrexate treatment of ovarian cancer patients. Int J Cancer 2003; 103: 294–299.
Ulrich CM, Yasui Y, Storb R et al. Pharmacogenetics of methotrexate: toxicity among marrow transplantation patients varies with the methylenetetrahydrofolate reductase C677T polymorphism. Blood 2001; 98: 231–234.
Robien K, Schubert MM, Bruemmer B et al. Predictors of oral mucositis in patients receiving hematopoietic cell transplants for chronic myelogenous leukemia. J Clin Oncol 2004; 22: 1268–1275.
Matsuo K, Suzuki R, Morishima Y, Hamajima N . Attribution of posttransplantation toxicity to methotrexate regarding genotype of methylenetetrahydrofolate reductase gene (MTHFR) polymorphism needs further clarification. Blood 2001; 98: 2283 (Letter).
Kalayoglu-Besisik S, Caliskan Y, Sargin D et al. Methylenetetrahydrofolate reductase C677T polymorphism and toxicity in allogeneic hematopoietic cell transplantation. Transplantation 2003; 76: 1775–1777 (Letter).
Chiusolo P, Reddiconto G, Casorelli I et al. Preponderance of methylenetetrahydrofolate reductase C677T homozygosity among leukemia patients intolerant to methotrexate. Ann Oncol 2002; 13: 1915–1918.
Ruggeri L, Capanni M, Urbani E et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Giebel S, Locatelli F, Lamparelli T et al. Survival advantage with KIR ligand incompatibility in hematopoietic stem cell transplantation from unrelated donors. Blood 2003; 102: 814–819.
Davies SM, Ruggieri L, DeFor T et al. Evaluation of KIR ligand incompatibility in mismatched unrelated donor hematopoietic transplants. Blood 2002; 100: 3825–3827.
Cook MA, Milligan DW, Fegan CD et al. The impact of donor KIR and patient HLA-C genotypes on outcome following HLA-identical sibling hematopoietic stem cell transplantation for myeloid leukemia. Blood 2004; 103: 1521–1526.
Gagne K, Brizard G, Gueglia B et al. Relevance of KIR gene polymorphisms in bone marrow transplantation outcome. Hum Immunol 2002; 63: 271–280.
Lin M-T, Storer B, Martin PJ et al. Relation of an interleukin-10 promoter polymorphism to graft-versus-host disease and survival after hematopoietic-cell transplantation. N Engl J Med 2003; 349: 2201–2210.
Socié G, Loiseau P, Tamouza R et al. Both genetic and clinical factors predict the development of graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Transplantation 2001; 72: 699–706.
Middleton PG, Taylor PRA, Jackson GH et al. Cytokine gene polymorphisms associating with severe acute graft-versus host disease in HLA-identical sibling transplants. Blood 1998; 92: 3943–3948.
Cooke KR, Ferrara JLM . A protective gene for graft-versus-host disease. N Engl J Med 2003; 349: 2183–2184.
Takahashi H, Furukawa T, Hashimoto S et al. Contribution of TNF-alpha and IL-10 gene polymorphisms to graft-versus-host disease following allo-hematopoietic stem cell transplantation. Bone Marrow Transplant 2000; 26: 1317–1323.
Remberger M, Jaksch M, Uzunel M, Mattson J . Serum levels of cytokines correlate to donor chimerism and acute graft-vs-host disease after haematopoietic stem cell transplantation. Eur J Haematol 2003; 70: 384–391.
Nordlander A, Uzunel M, Mattson J, Remberger M . The TNF d4 allele is correlated to moderate-to-severe acute graft-versus-host disease after allogeneic stem cell transplantation. Br J Haematol 2002; 119: 1133–1136.
Kögler G, Middleton PG, Wilke M et al. Recipient cytokine genotypes for TNF-[alpha] and IL-10 and the minor histocompatibility antigens HY and CD31 codon 125 are not associated with occurrence or severity of acute GVHD in unrelated cord blood transplantation: a retrospective analysis. Transplantation 2002; 74: 1167–1175.
Rocha V, Franco RF, Porcher R et al. Host defense and inflammatory gene polymorphisms are associated with outcomes after HLA-identical sibling bone marrow transplantation. Blood 2002; 100: 3908–3918.
Mullighan CG, Heatley S, Doherty K et al. Mannose-binding lectin gene polymorphisms are associated with major infection following allogeneic hemopoietic stem cell transplantation. Blood 2002; 99: 3524–3529.
Holmes CL, Russel JA, Walley KR . Genetic polymorphisms in sepsis and septic shock: Role in prognosis and potential for therapy. Chest 2003; 124: 1103–1115.
Valdimarsson H, Stefansson M, Vikingsdottir T et al. Reconstitution of opsonizing activity by infusion of mannan-binding lectin (MBL) to MBL-deficient humans. Scand J Immunol 1998; 48: 116–123.
Valdimarsson H, Vikingsdottir T, Bang P et al. Human plasma-derived mannose-binding lectin: a phase I safety and pharmacokinetic study. Scand J Immunol 2004; 59: 97–102.
Cavet J, Dickinson AM, Norden J et al. Interferon-γ and interleukin-6 gene polymorphisms associate with graft-versus-host disease in HLA-matched sibling bone marrow transplantation. Blood 2001; 98: 1594–1600.
Juckett MB, Cohen EP, Keever-Taylor CA et al. Loss of renal function following bone marrow transplantation: an analysis of angiotensin converting enzyme D/I polymorphism and other clinical risk factors. Bone Marrow Transplant 2001; 27: 451–456.
Rigat B, Hubert C, Alhenc-Gelas F et al. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest 1990; 86: 1343–1346.
Bagchi D, Prasad R, Das DK . Direct scavenging of free radicals by captopril, an antiotensin converting enzyme inhibitor. Biochem Biophys Res Commun 1989; 158: 52–57.
Lu KC, Jaramillo A, Lecha RL et al. Interleukin-6 and interferon-γ gene polymorphisms in the development of bronchiolitis obliterans syndrome after lung transplantation. Transplantation 2002; 74: 1297–1302.
Khurshid I, Anderson LC . Non-infectious pulmonary complications after bone marrow transplantation. Postgrad Med J 2002; 78: 257–262.
Aplenc R, Vachani A, Han P et al. Pharmacogenetics of gemtuzumab-associated hepatic sinusoidal occlusion syndrome after hematopoietic stem cell transplant. Acta Haematol 2003; 110: 207–210.
Leather HL . Drug interactions in the hematopoietic stem cell transplant (HSCT) recipient: what every transplanter needs to know. Bone Marrow Transplant 2004; 33: 137–152.
Goetz MP, Ames MM, Weinshilboum RM . Primer on medical genomics. Part XII: Pharmacogenomics – general principles with cancer as a model. Mayo Clin Proc 2004; 79: 376–384.
Altes A, Remacha AF, Sureda A et al. Iron overload might increase transplant-related mortality in haematopoietic stem cell transplantation. Bone Marrow Transplant 2002; 29: 987–989.
Evens AM, Mehta J, Gordon LI . Rust and corrosion in hematopoietic stem cell transplantation: the problem of iron and oxidative stress. Bone Marrow Transplant 2004; 34: 561–571.
Ho GT, Parker A, MacKenzie JF et al. Abnormal liver function tests following bone marrow transplantation: aetiology and role of liver biopsy. Eur J Gastreoenterol Hepatol 2004; 16: 157–162.
Morado M, Ojeda F, Garcia-Bustos J et al. BMT: serum ferritin as risk factor for veno-occlusive disease of the liver. Prospective cohort study. Hematology 2000; 4: 505–512.
Or R, Matzner U, Konijn AM . Serum ferritin in patients undergoing bone marrow transplantation. Cancer 1987; 60: 1127–1131.
Azar N, Valla D, Abdel-Samad I et al. Liver dysfunction in allogeneic bone marrow transplantation recipients. Transplantation 1996; 62: 56–61.
Lichtman SM, Attivissimo L, Goldman IS et al. Secondary hemochromatosis as a long-term complication of the treatment of hematologic malignancies. Am J Hematol 1999; 61: 262–264.
Mahendra P, Hood IM, Bass G et al. Severe hemosiderosis post allogeneic bone marrow transplantation. Hematol Oncol 1996; 14: 33–35.
Stevens RG, Morris JE, Anderson LE . Commentary: hemochromatosis heterozygotes may constitute a radiation-sensitive subpopulation. Radiat Res 2000; 153: 844–847.
Anderson GJ . Non-transferrin-bound iron and cellular toxicity. J Gastroenterol Hepatol 1999; 14: 126–132.
Videla LA, Fernandez V, Tapia G, Varela P . Oxidative stress-mediated hepatotoxicity of iron and copper: role of Kupffer cells. Biometals 2003; 16: 103–111.
McKay PJ, Murphy JA, Cameron S et al. Iron overload and liver dysfunction after allogeneic or autologous bone marrow transplantation. Bone Marrow Transplant 1996; 17: 63–66.
Harrison P, Neilson JR, Marwah SS et al. Role of non-transferrin-bound iron in iron overload and liver dysfunction in long-term survivors of acute leukaemia and bone marrow transplantation. J Clin Pathol 1996; 49: 853–856.
Strasser SI, Kowdley KV, Sale GE, McDonald GB . Iron overload in bone marrow transplant recipients. Bone Marrow Transplant 1998; 22: 167–173.
Grigg AP, Bhathal PS . Compound heterozygosity for haemochromatosis gene mutations in hepatic iron overload in allogeneic bone marrow transplant recipients. Pathology 2001; 33: 44–49.
Weinberg ED . Microbial pathogens with impaired ability to acquire host iron. Biometals 2000; 13: 85–89.
Hunter RL, Bennett B, Towns M, Vogler WR . Transferrin in disease II: defects in the regulation of transferrin saturation with iron contribute to susceptibility to infection. Am J Clin Pathol 1984; 81: 748–753.
Iglesias-Osma C, Gonzalez-Villaron L, San Miguel JF et al. Iron metabolism and fungal infections in patients with haematological malignancies. J Clin Pathol 1995; 48: 223–225.
Gordon LI, Brown SG, Tallman MS et al. Sequential changes in serum iron and ferritin in patients undergoing high-dose chemotherapy and radiation with autologous bone marrow transplantation: possible implications for treatment related toxicity. Free Radic Biol Med 1995; 18: 383–389.
Dürken M, Herrnring C, Finckh B et al. Impaired plasma antioxidative defense and increased non-transferrin-bound iron during high-dose chemotherapy and radiochemotherapy preceding bone marrow transplantation. Free Radic Biol Med 2000; 28: 887–894.
Bradley SJ, Gosriwatana I, Srichairatanakool S et al. Non-transferrin-bound iron induced by myeloablative chemotherapy. Br J Haematol 1997; 99: 337–343.
Recalcati S, Pometta R, Levi S et al. Response of monocyte iron regulatory protein activity to inflammation: abnormal behavior in genetic hemochromatosis. Blood 1998; 91: 2565–2572.
Witherspoon RP, Fisher LD, Schoch G et al. Secondary cancers after bone marrow transplantation for leukemia or aplastic anemia. N Engl J Med 1989; 321: 784–789.
Stevens RG, Graubard BI, Micozzi MS et al. Moderate elevation of body iron level and increased risk of cancer occurrence and death. Int J Cancer 1994; 56: 364–369.
Nelson RL, Davis FG, Persky V, Becker E . Risk of neoplastic and other diseases among people with heterozygosity for hereditary hemochromatosis. Cancer 1995; 76: 875–879.
Kallianpur AR, Hall LD, Yadav M et al. Increased prevalence of the HFE C282Y hemochromatosis allele in women with breast cancer. Cancer Epidemiol Biomarkers Prev 2004; 13: 205–212.
Varkonyi J, Tarkovacs G, Karadi I et al. High incidence of hemochromatosis gene mutations in the myelodysplastic syndrome: the Budapest study on 50 patients. Acta Haematol 2003; 109: 64–67.
Andrews NC . Disorders of iron metabolism. N Engl J Med 1999; 341: 1986–1995.
Butt NM, Clark RE . Autografting as a risk factor for persisting iron overload in long-term survivors of acute myeloid leukaemia. Bone Marrow Transplant 2003; 32: 909–913.
Tomas JF, Pinilla I, Garcia-Buey ML et al. Long-term liver dysfunction after allogeneic bone marrow transplantation: clinical features and course in 61 patients. Bone marrow Transplant 2000; 26: 649–655.
Buss JL, Torti FM, Torti SV . The role of iron chelation in cancer therapy. Curr Med Chem 2003; 10: 1021–1034.
Gaziev D, Giardini C, Angelucci E et al. Intravenous chelation therapy during transplantation for thalassemia. Haematologica 1995; 80: 300–304.
Sahlstedt L, von Bonsdorff L, Ebeling F et al. Effective binding of free iron by a single intravenous dose of human apotransferrin in haematological stem cell transplant patients. Br J Haematol 2002; 119: 547–553.
Sonwalkar SA, James RM, Ahmad T et al. Fulminant Crohn's colitis after allogeneic stem cell transplantation. Gut 2003; 52: 1518–1521.
McMilin K . Allogeneic hematopoietic stem cell transplantation and the risk for transmission of heritable malignancy. Transfusion 2002; 42: 495–504.
Ramaswamy S . Translating cancer genomics into clinical oncology. N Engl J Med 2004; 350: 1814–1816.
Lossos IS, Czerwinski DK, Alizadeh AA et al. Prediction of survival in diffuse large-B-cell lymphoma based on the expression of six genes. N Engl J Med 2004; 350: 1828–1837.
Ritchie MD, Moore JH . Power of multifactor dimensionality reduction for detecting gene–gene interactions in the presence of genotyping error, missing data, phenocopy, and genetic heterogeneity. Genet Epidemiol 2003; 24: 150–157.
Hahn LW, Ritchie MD, Moore JH . Multifactor dimensionality reduction software for detecting gene–gene and gene–environment interactions. Bioinformatics 2003; 19: 376–382.
Schots R, Kaufman L, Van Riet I et al. Pro-inflammatory cytokines and their role in the development of major transplant-related complications in the early phase after allogeneic bone marrow transplantation. Leukemia 2003; 17: 1150–1156.
Baker KS, Roncarolo MG, Peters C et al. High spontaneous IL-10 production in unrelated bone marrow transplant recipients is associated with fewer transplant-related complications and early deaths. Bone Marrow Transplant 1999; 23: 1123–1129.
Anscher MS, Peters WP, Reisenbichler H et al. Transforming growth factor beta as a predictor of liver and lung fibrosis after autologous bone marrow transplantation for advanced breast cancer. N Engl J Med 1993; 328: 1592–1598.
Miranda CJ, Makui H, Soares RJ et al. HFE deficiency increases susceptibility to cardiotoxicity and exacerbates changes in iron metabolism induced by doxorubicin. Blood 2003; 102: 2574–2580.
Aplenc R, Glatfelter W, Han P et al. CYP3A genotypes and treatment response in paediatric acute lymphoblastic leukaemia. Br J Haematol 2003; 122: 240–244.
Cederbaum AI, Wu D, Mari M, Bai J . CYP2E1-dependent toxicity and oxidative stress in HepG2 cells. Free Radic Biol Med 2001; 31: 1539–1543.
Kuwano K, Hagimoto N, Maeyama T et al. Mitochondria-mediated apoptosis of lung epithelial cells in idiopathic interstitial pneumonias. Lab Invest 2002; 82: 1695–1706.
Toffoli G, Veronesi A, Boiocchi M et al. MTHFR gene polymorphism and severe toxicity during adjuvant treatment of early breast cancer with cyclophosphamide, methotrexate, and fluorouracil (CMF). Ann Oncol 2000; 11: 373–374 (Letter).
Cavet J, Middleton PG, Segall M et al. Recipient tumor necrosis factor-α and interleukin-10 gene polymorphisms associate with early mortality and acute graft-versus-host disease severity in HLA-matched sibling bone marrow transplants. Blood 1999; 94: 3941–3946.
Brittenham GM, Griffith PM, Nienhuis AW et al. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med 1994; 331: 567–573.
Savarese DMF, Savy G, Vahdat L et al. Prevention of chemotherapy and radiation toxicity with glutamine. Cancer Treat Rev 2003; 29: 501–513.
Ziegler TR . Glutamine supplementation in bone marrow transplantation. Br J Nutr 2002; 87 (Suppl. 1): S9–S15.
Jonas CR, Puckett AB, Jones DP et al. Plasma antioxidant status after high-dose chemotherapy: a randomized trial of parenteral nutrition in bone marrow transplantation patients. Am J Clin Nutr 2000; 72: 181–189.
Chalandon Y, Roosnek E, Mermillod B et al. Prevention of veno-occlusive disease with defibrotide after allogeneic stem cell transplantation. Biol Blood Marrow Transplant 2004; 10: 347–354.
Gabriel D, Shea T, Oludamilola O et al. The effect of oral mucositis on morbidity and mortality in bone marrow transplant. Semin Oncol 2003; 30 (Suppl. 18): 76–83.
Hwang WY, Koh LP, Ng HJ et al. A randomized trial of amifostine as a cytoprotectant for patients receiving myeloablative therapy for allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2004; 34: 51–56.
Haddad IY . Idiopathic pneumonia after marrow transplantation: when are antioxidants effective? Am J Respir Crit Care Med 2002; 166: 1532–1534.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kallianpur, A. Genomic screening and complications of hematopoietic stem cell transplantation: has the time come?. Bone Marrow Transplant 35, 1–16 (2005). https://doi.org/10.1038/sj.bmt.1704716
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704716
Keywords
This article is cited by
-
The prognostic role of hemochromatosis H63D allele in allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2012)
-
Donor single nucleotide polymorphism in the CCR9 gene affects the incidence of skin GVHD
Bone Marrow Transplantation (2010)
-
The impact of methylenetetrahydrofolate reductase (MTHFR) C677T gene polymorphism on transplant-related variables after allogeneic hematopoietic cell transplantation in patients receiving MTX as GVHD prophylaxis
Bone Marrow Transplantation (2008)
-
Decreased risk of acute graft-versus-host disease following allogeneic hematopoietic stem cell transplantation in patients with the 5,10-methylenetetrahydrofolate reductase 677TT genotype
International Journal of Hematology (2008)
-
Mapping of susceptibility and protective loci for acute GVHD in unrelated HLA-matched bone marrow transplantation donors and recipients using 155 microsatellite markers on chromosome 22
Immunogenetics (2007)