Abstract
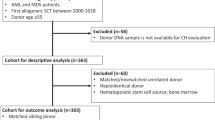
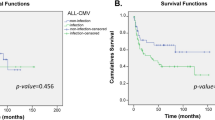
The most frequent complication of allogeneic hematopoietic stem cell transplantation is acute Graft versus Host Disease (aGVHD). Proliferation and differentiation of donor T cells initiate inflammatory response affecting the skin, liver, and gastrointestinal tract. Besides recipient–donor HLA disparities, disease type, and the conditioning regimen, variability in the non-HLA genotype have an impact on aGVHD onset, and genetic variability of key cytokines and chemokines was associated with increased risk of aGVHD. To get further insight into the recipient genetic component of aGVHD grades 2–4 in pediatric patients, we performed an exome-wide association study in a discovery cohort (n = 87). Nine loci sustained correction for multiple testing and were analyzed in a validation group (n = 168). Significant associations were replicated for ERC1 rs1046473, PLEK rs3816281, NOP9 rs2332320 and SPRED1 rs11634702 variants through the interaction with non-genetic factors. The ERC1 variant was significant among patients that received the transplant from HLA-matched related individuals (p = 0.03), bone marrow stem cells recipients (p = 0.007), and serotherapy-negative patients (p = 0.004). NOP9, PLEK, and SPRED1 effects were modulated by stem cell source, and serotherapy (p < 0.05). Furthermore, ERC1 and PLEK SNPs correlated with aGVHD 3-4 independently of non-genetic covariates (p = 0.02 and p = 0.003). This study provides additional insight into the genetic component of moderate to severe aGVHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available upon request. The request should be made to the data access committee composed of senior authors of this study: Dr. M. Krajinovic, maja.krajinovic@umontreal.ca; Dr. H. Bittencourt, henrique.bittencourt.hsj@ssss.gouv.qc.ca; Dr. M. Ansari, marc.ansari@hcuge.ch, and President of Ethics committee at SJUHC, G. Cardinal, genevieve.cardinal@recherche-ste-justine.qc.ca.
References
Adom D, Rowan C, Adeniyan T, Yang J, Paczesny S. Biomarkers for allogeneic HCT outcomes. Front Immunol. 2020;11:673.
Shaw PJ, Kan F, Woo Ahn K, Spellman SR, Aljurf M, Ayas M, et al. Outcomes of pediatric bone marrow transplantation for leukemia and myelodysplasia using matched sibling, mismatched related, or matched unrelated donors. Blood. 2010;116:4007–15.
Eapen M, Horowitz MM, Klein JP, Champlin RE, Loberiza FR Jr., Ringdén O, et al. Higher mortality after allogeneic peripheral-blood transplantation compared with bone marrow in children and adolescents: the Histocompatibility and Alternate Stem Cell Source Working Committee of the International Bone Marrow Transplant Registry. J Clin Oncol. 2004;22:4872–80.
Alsultan A, Giller RH, Gao D, Bathurst J, Hild E, Gore L, et al. GVHD after unrelated cord blood transplant in children: characteristics, severity, risk factors and influence on outcome. Bone Marrow Transplant. 2011;46:668–75.
Zeiser R, Blazar BR. Acute graft-versus-host disease—biologic process, prevention, and therapy. N Engl J Med. 2017;377:2167–79.
Martínez-Laperche C, Buces E, Aguilera-Morillo MC, Picornell A, González-Rivera M, Lillo R, et al. A novel predictive approach for GVHD after allogeneic SCT based on clinical variables and cytokine gene polymorphisms. Blood Adv. 2018;2:1719–37.
Ferrara JLM, Levine JE, Reddy P, Holler E. Graft-versus-host disease. Lancet. 2009;373:1550–61.
Dzierzak-Mietla M, Markiewicz M, Siekiera U, Mizia S, Koclega A, Zielinska P, et al. Occurrence and impact of minor histocompatibility antigens’ disparities on outcomes of hematopoietic stem cell transplantation from HLA-matched sibling donors. Bone Marrow Res. 2012;2012:257086.
Martin PJ, Levine DM, Storer BE, Warren EH, Zheng X, Nelson SC, et al. Genome-wide minor histocompatibility matching as related to the risk of graft-versus-host disease. Blood. 2017;129:791–8.
Kim DDH, Yun J, Won H-H, Cheng L, Su J, Xu W, et al. Multiple single-nucleotide polymorphism-based risk model for clinical outcomes after allogeneic stem-cell transplantation, especially for acute graft-versus-host disease. Transplantation. 2012;94:1250–7.
Ansari M, Curtis PH, Uppugunduri CRS, Rezgui MA, Nava T, Mlakar V, et al. GSTA1 diplotypes affect busulfan clearance and toxicity in children undergoing allogeneic hematopoietic stem cell transplantation: a multicenter study. Oncotarget. 2017;8:90852–67.
Ansari M, Petrykey K, Rezgui MA, Del Vecchio V, Cortyl J, Ralph RO, et al. Genetic susceptibility to hepatic sinusoidal obstruction syndrome in pediatric patients undergoing hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. 2020;26:920–7.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–8.
Holtan SG, Khera N, Levine JE, Chai X, Storer B, Liu HD, et al. Late acute graft-versus-host disease: a prospective analysis of clinical outcomes and circulating angiogenic factors. Blood. 2016;128:2350–8.
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
Adzhubei I, Jordan DM, Sunyaev SR. Predicting functional effect of human missense mutations using PolyPhen-2. Curr Protoc Hum Genet. 2013;Chapter 7:Unit7 20.
Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009;4:1073–81.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75.
Benjamini YH, Controlling Y. the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B: Methodol. 1995;57:289–300.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Labuda D, Krajinovic M, Richer C, Skoll A, Sinnett H, Yotova V, et al. Rapid detection of CYP1A1, CYP2D6, and NAT variants by multiplex polymerase chain reaction and allele-specific oligonucleotide assay. Anal Biochem. 1999;275:84–92.
Huezo-Diaz P, Uppugunduri CR, Tyagi AK, Krajinovic M, Ansari M. Pharmacogenetic aspects of drug metabolizing enzymes in busulfan based conditioning prior to allogenic hematopoietic stem cell transplantation in children. Curr Drug Metab. 2014;15:251–64.
Zhu Q, Yan L, Liu Q, Zhang C, Wei L, Hu Q, et al. Exome chip analyses identify genes affecting mortality after HLA-matched unrelated-donor blood and marrow transplantation. Blood. 2018;131:2490–9.
Liu T, Zhang L, Joo D, Sun SC. NF-κB signaling in inflammation. Signal Transduct Target Ther. 2017;2:17023-.
Magenau J, Runaas L, Reddy P. Advances in understanding the pathogenesis of graft-versus-host disease. Br J Haematol. 2016;173:190–205.
Jeanette LDS, Bottero V, Young DB, Shevchenko A, Mercurio F, Verma IM. Activation of transcription factor NF-κB requires ELKS, an IκB kinase regulatory subunit. Science. 2004;304:1963–7.
Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461:1071–8.
Kuba A, Raida L, Mrazek F, Schneiderova P, Kriegova E, Langova K, et al. NFKB1 gene single-nucleotide polymorphisms: implications for graft-versus-host disease in allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2020;99:609–18.
Alpay M, Backman LR, Cheng X, Dukel M, Kim WJ, Ai L, et al. Oxidative stress shapes breast cancer phenotype through chronic activation of ATM-dependent signaling. Breast Cancer Res Treatment. 2015;151:75–87.
Liu CJ, Fu X, Xia M, Zhang Q, Gu Z, Guo AY. miRNASNP-v3: a comprehensive database for SNPs and disease-related variations in miRNAs and miRNA targets. Nucleic Acids Res. 2020;49:D1276–81.
Gong J, Tong Y, Zhang HM, Wang K, Hu T, Shan G, et al. Genome-wide identification of SNPs in microRNA genes and the SNP effects on microRNA target binding and biogenesis. Hum Mutat. 2012;33:254–63.
Medrano LM, Pascual V, Bodas A, López-Palacios N, Salazar I, Espino-Paisán L, et al. Expression patterns common and unique to ulcerative colitis and celiac disease. Ann Hum Genet. 2019;83:86–94.
Hoppmann N, Graetz C, Paterka M, Poisa-Beiro L, Larochelle C, Hasan M, et al. New candidates for CD4 T cell pathogenicity in experimental neuroinflammation and multiple sclerosis. Brain. 2015;138(Pt 4):902–17.
Lundmark A, Davanian H, Båge T, Johannsen G, Koro C, Lundeberg J, et al. Transcriptome analysis reveals mucin 4 to be highly associated with periodontitis and identifies pleckstrin as a link to systemic diseases. Sci Rep. 2015;5:18475.
Ding Y, Kantarci A, Badwey JA, Hasturk H, Malabanan A, Van Dyke TE. Phosphorylation of Pleckstrin increases proinflammatory cytokine secretion by mononuclear phagocytes in diabetes mellitus. J Immunol. 2007;179:647–54.
Hasturk H, Kantarci A, Van Dyke TE. Oral inflammatory diseases and systemic inflammation: role of the macrophage. Front Immunol. 2012;3:118.
Battle A, Brown CD, Engelhardt BE, Montgomery SB. Genetic effects on gene expression across human tissues. Nature. 2017;550:204–13.
Pasmant E, Gilbert-Dussardier B, Petit A, de Laval B, Luscan A, Gruber A, et al. SPRED1, a RAS MAPK pathway inhibitor that causes Legius syndrome, is a tumour suppressor downregulated in paediatric acute myeloblastic leukaemia. Oncogene. 2015;34:631–8.
Olsson L, Castor A, Behrendtz M, Biloglav A, Forestier E, Paulsson K, et al. Deletions of IKZF1 and SPRED1 are associated with poor prognosis in a population-based series of pediatric B-cell precursor acute lymphoblastic leukemia diagnosed between 1992 and 2011. Leukemia. 2014;28:302–10.
Jansen F, Yang X, Hoelscher M, Cattelan A, Schmitz T, Proebsting S, et al. Endothelial microparticle-mediated transfer of MicroRNA-126 promotes vascular endothelial cell repair via SPRED1 and is abrogated in glucose-damaged endothelial microparticles. Circulation. 2013;128:2026–38.
Biedermann BC. Vascular endothelium and graft-versus-host disease. Best Practice Res Clin Haematol. 2008;21:129–38.
Tichelli A, Gratwohl A. Vascular endothelium as ‘novel’ target of graft-versus-host disease. Best Practice Res Clin Haematol. 2008;21:139–48.
Cao X-N, Kong Y, Song Y, Shi M-M, Zhao H-Y, Wen Q, et al. Impairment of bone marrow endothelial progenitor cells in acute graft-versus-host disease patients after allotransplant. Br J Haematol. 2018;182:870–86.
Galli SJ, Grimbaldeston M, Tsai M. Immunomodulatory mast cells: negative, as well as positive, regulators of immunity. Nat Rev Immunol. 2008;8:478–86.
Leveson-Gower DB, Sega EI, Kalesnikoff J, Florek M, Pan Y, Pierini A, et al. Mast cells suppress murine GVHD in a mechanism independent of CD4+CD25+ regulatory T cells. Blood. 2013;122:3659–65.
Ishizaki T, Tamiya T, Taniguchi K, Morita R, Kato R, Okamoto F, et al. miR126 positively regulates mast cell proliferation and cytokine production through suppressing Spred1. Genes Cells. 2011;16:803–14.
Suzuki M, Morita R, Hirata Y, Shichita T, Yoshimura A. Spred1, a suppressor of the Ras-ERK pathway, negatively regulates expansion and function of group 2 innate lymphoid cells. J Immunol. 2015;195:1273–81.
Munneke JM, Björklund AT, Mjösberg JM, Garming-Legert K, Bernink JH, Blom B, et al. Activated innate lymphoid cells are associated with a reduced susceptibility to graft-versus-host disease. Blood. 2014;124:812–21.
Thomson E, Rappsilber J, Tollervey D. Nop9 is an RNA binding protein present in pre-40S ribosomes and required for 18S rRNA synthesis in yeast. RNA. 2007;13(12):2165–74.
Zhang J, Teramoto T, Qiu C, Wine RN, Gonzalez LE, Baserga SJ, et al. Nop9 recognizes structured and single-stranded RNA elements of preribosomal RNA. RNA. 2020;26(8):1049–59.
Nudel R, Simpson NH, Baird G, O’Hare A, Conti-Ramsden G, Bolton PF, et al. Genome-wide association analyses of child genotype effects and parent-of-origin effects in specific language impairment. Genes Brain Behav. 2014;13(4):418–29.
Turpeinen H, Ojala PJ, Ojala K, Miettinen M, Volin L, Partanen J. Minor histocompatibility antigens as determinants for graft-versus-host disease after allogeneic haematopoietic stem cell transplantation. Int J Immunogenet. 2013;40(6):495–501.
Akatsuka Y, Warren EH, Gooley TA, Brickner AG, Lin M-T, Hansen JA, et al. Disparity for a newly identified minor histocompatibility antigen, HA-8, correlates with acute graft-versus-host disease after haematopoietic stem cell transplantation from an HLA-identical sibling. Br J Haematol. 2003;123:671–5.
Sharma SB, Lin CC, Farrugia MK, McLaughlin SL, Ellis EJ, Brundage KM, et al. MicroRNAs 206 and 21 cooperate to promote RAS-extracellular signal-regulated kinase signaling by suppressing the translation of RASA1 and SPRED1. Mol Cell Biol. 2014;34:4143–64.
Acknowledgements
Reported On Behalf of the Pediatric Disease Working Party of the European Society for Blood and Marrow Transplantation. The authors would like to thank all patients and their parents for the participation in the study, as well as all study collaborators for their valuable contribution.
Funding
This investigation was supported by grants from the Swiss National Science Foundation (Grant No. 153389), CANSEARCH Foundation, AOK Foundation, and Foundation of Charles-Bruneau.
Author information
Authors and Affiliations
Contributions
M.A., H.B., and M.K. designed the study; D.S. supervised WES analyses; P.S.-O. and P.B. contributed to bioinformatics analyses; Y.T., I.H.B., J.J.B., R.G.M.B., J.H.D., V.L., B.S.K., S.C., M.A., H.B., M.A.R. contributed to patients’ sample and data processing; K.P., J.C., V.D.V., and M.K. executed computational and statistical analysis; T.N., S.J.M., C.R.S.U. contributed to interpretation of results; M.A.R. and M.A. performed the replication analysis; M.K. drafted the manuscript and all authors revised it critically.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent
Written informed consent was obtained from every patient or parent/legal guardian. The study was conducted in accordance with the Declaration of Helsinki and was approved by Research Ethics Board of SJUHC.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ansari, M., Petrykey, K., Rezgui, M.A. et al. Genetic susceptibility to acute graft versus host disease in pediatric patients undergoing HSCT. Bone Marrow Transplant 56, 2697–2704 (2021). https://doi.org/10.1038/s41409-021-01386-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01386-8