Summary:
Severe metabolic abnormalities occurring within 100 days after allogeneic hematopoietic cell transplantation (HCT) were investigated in 311 patients. The metabolic abnormalities included hyper- and hypocalcemia, hypophosphatemia, hyper- and hypokalemia, hyper- and hyponatremia, hyper- and hypomagnesemia, hypercholesterolemia, hyper- and hypoglycemia, and hyperuricemia. Severe abnormalities, defined as grades III–V by NCI CTCAE v3.0, occurred in 269 patients (86.5%). Multivariate analysis revealed that patients with moderate-to-severe hepatic veno-occlusive disease had significantly higher risk for the occurrence of severe metabolic abnormalities. Grades III–IV acute graft-versus-host disease was the most frequently associated with individual metabolic abnormalities. Patients with at least one severe metabolic abnormality had significantly higher day 100 nonrelapse mortality (P=0.015) and lower 5-year overall survival (P=0.002) than those without severe abnormalities. The number of metabolic abnormalities also stratified the patients with different clinical outcomes. In conclusion, severe metabolic abnormalities occurring within 100 days after allogeneic HCT were common, and their occurrence was significantly associated with inferior clinical outcomes. These results indicate that metabolic parameters should be monitored in patients undergoing allogeneic HCT and that the occurrence of severe metabolic abnormalities should be considered an important toxicity parameter in prospective clinical trials regarding allogeneic HCT.
Similar content being viewed by others
Main
Patients undergoing allogeneic hematopoietic cell transplantation (HCT) are prone to develop a variety of metabolic abnormalities, which vary in severity from mild to life-threatening. Most of these metabolic abnormalities occur during the early post-transplant period.1 Various metabolic derangements are associated with high dose-conditioning therapy,1,2 immunosuppressants used to prevent or treat graft-versus-host disease (GVHD),3,4,5 total parenteral nutrition (TPN),6,7 infective or inflammatory processes,1 and other etiologies. These metabolic abnormalities may be accompanied by other post-transplant complications, including GVHD and hepatic veno-occlusive disease (VOD).
Severe metabolic abnormalities may have an adverse effect on clinical outcomes after allogeneic HCT. There is little information about the risk factors associated with severe metabolic abnormalities and the clinical outcomes of patients with these abnormalities. Although there have been several studies reporting metabolic abnormalities after allogeneic HCT, only one or two abnormalities were investigated or metabolic abnormalities were not the main subject in most of the studies. We therefore investigated the severe metabolic abnormalities that occurred within 100 days after allogeneic HCT in 311 patients to determine the frequency, risk factors, and clinical significance of the abnormalities. We found that metabolic abnormalities were very common after allogeneic HCT and that patients with severe metabolic abnormalities had inferior clinical outcomes.
Patients and methods
Patients
Between December 1993 and August 2003, 315 adult patients underwent allogeneic HCT at the Asan Medical Center, Seoul, Korea. Four of these patients were excluded due to inadequate data regarding metabolic abnormalities. We collected clinical and laboratory data on the remaining 311 patients from the HCT database of the Asan Medical Center.
The 311 patients consisted of 181 males and 130 females, with a median age of 32 years (range, 15–59 years) (Table 1). In all, 103 patients had acute myelogenous or mixed leukemia, 57 had acute lymphoblastic leukemia, 57 had chronic myelogenous leukemia, 26 had myelodysplastic syndrome, 34 had severe aplastic anemia, and 34 had other diagnoses. The median time from diagnosis to HCT was 141 days (range, 8–5706 days). At the time of HCT, 95 patients had high-risk features, defined as having acute leukemia in relapse or in second or subsequent remission (n=35), chronic myelogenous leukemia in accelerated or blastic phase (n=11), chemotherapy resistant or relapsed lymphoma, myeloma or solid tumor (n=27), advanced myelodysplastic syndrome (MDS) (chronic myelomonocytic leukemia, refractory anemia with excess of blasts, or refractory anemia with excess of blasts in transformation; n=16), and nonmalignant hematological disorder with active infection or bleeding (n=6). The hematopoietic cell donor for 238 patients was a sibling, and for 73 an unrelated volunteer.
Transplantation procedure
A conditioning regimen of busulfan plus cyclophosphamide was given to 243 patients with malignant disorders, including MDS. Four of these patients each received an additional agent: cytarabine, etoposide, melphalan, or antithymocyte globulin (ATG), respectively. For the regimen of busulfan plus cyclophosphamide, oral busulfan (1 mg/kg every 6 h for a total of 16 doses from days −7 to −4; n=188) was administered before August 2002, whereas intravenous busulfan (0.8 mg/kg every 6 h for a total of 16 doses from days −7 to −4; n=55) was administered thereafter. Cyclophosphamide was administered to all patients at a dose of 60 mg/kg intravenously on days −3 and −2. In all, 32 patients with severe aplastic anemia were conditioned with cyclophosphamide (50 mg/kg intravenously on days −5 to −2) plus ATG (30 mg/kg intravenously on days −4 to −2). Two patients with severe aplastic anemia were conditioned with cyclophosphamide (50 mg/kg intravenously on days −3 and −2), ATG (30 mg/kg intravenously on days −4 to −2), and fludarabine (30 mg/m2 intravenously on days −6 to −2). In all, 34 patients received reduced-intensity regimens, with 30 receiving busulfan (1 mg/kg orally every 6 h for a total of eight doses on days −7 and −6), fludarabine (30 mg/m2 intravenously on days −7 to −2), and ATG (10–20 mg/kg intravenously on days −5 to −2), two receiving melphalan (100 mg/m2 intravenously on day −2) and fludarabine (30 mg/m2 intravenously on days −6 to −2), and two receiving cyclophosphamide (60 mg/kg intravenously on days −3 and −2), fludarabine (30 mg/m2 intravenously on days −7 to −3), and ATG (10 mg/kg intravenously on days −5 to −2).
In all, 277 patients received donor bone marrow grafts on day 0, whereas 34 patients received peripheral donor blood hematopoietic cells mobilized with granulocyte colony-stimulating factor (G-CSF, 10 μg/kg/day subcutaneously for 4 days) on days 0 and 1. All patients received non-T-cell depleted grafts, except for one who received G-CSF-mobilized peripheral blood hematopoietic cells from a haplo-identical donor. All patients received prophylactic therapy for GVHD with cyclosporine only (n=72) or cyclosporine plus methotrexate (n=239). Cyclosporine (1.5 mg/kg) was given intravenously every 12 h starting on day −1 and switched to an oral dose when oral intake became feasible. Intravenous methotrexate was given at a dose of 15 mg/m2 on day 1 and at 10 mg/m2 on days 3, 6, and 11. For patients conditioned with the reduced-intensity regimen, the day 11 methotrexate dose was omitted. Patients conditioned with busulfan plus cyclophosphamide were administered heparin (100 U/kg/day) on days −7 to 30. All patients received 450 μg of G-CSF intravenously once daily starting on day 0 or 5, until peripheral blood absolute neutrophil count was over 3000/μl. Patients who received cyclophosphamide as a conditioning therapy were treated with mesna and hyperhydration of normal saline to prevent hemorrhagic cystitis.
Monitoring of patients
Blood was drawn every day for complete blood counts, including reticulocyte counts. Blood chemistry and electrolytes, including magnesium level, were determined twice weekly, or more frequently if necessary. All patients were prospectively monitored for the occurrence of hepatic VOD and GVHD. Hepatic VOD was diagnosed in patients having at least two of the following before day 30: (1) hyperbilirubinemia (bilirubin ⩾2.0 mg/dl), (2) painful hepatomegaly, and (3) unexplained weight gain (>2% from baseline),8 with no other explanation for these signs and symptoms present at the time of diagnosis. Severity of VOD was classified as mild, moderate or severe.9 Patients who met the criteria of VOD, but who were not treated and whose illness was self-limiting, were considered to have mild VOD. Those whose VOD resolved but who received treatment, such as diuretics for fluid retention or narcotic analgesics for painful hepatomegaly, were considered to have moderate VOD. Patients who died of VOD or whose VOD did not resolve by post-transplant day 100 were considered to have severe VOD.
A diagnosis of acute GVHD was made on the basis of clinical symptoms, laboratory tests, and whenever possible, histopathological findings of the skin, oral mucosa, and gastrointestinal tract,10 and classified according to clinical criteria.11 Acute GVHD was initially treated with methylprednisolone of 1–2 mg/kg/day.
Statistical analysis
Metabolic abnormalities analyzed in this study included hyper- and hypocalcemia, hypophosphatemia, hyper- and hypokalemia, hyper- and hyponatremia, hyper- and hypomagnesemia, hypercholesterolemia, hyper- and hypoglycemia, and hyperuricemia. For each patient, the worst laboratory value for each abnormality within 100 days after HCT was recorded. Since calcium can be falsely low if hypoalbuminemia (ie serum albumin <4.0 g/dl) is present, hypocalcemia was corrected according to the formula, corrected calcium (mg/dl)=total calcium (mg/dl)−0.8 × (serum albumin (g/dl)−4).12
Metabolic abnormalities were graded according to NCI Common Terminology Criteria for Adverse Events (CTCAE) v3.0, which classifies each toxicity as grades I–V. In this study, grades III–V toxicities were defined as severe abnormalities.
Individual patient characteristics and occurrence of hepatic VOD or acute GVHD were analyzed for their association with severe metabolic abnormalities using the χ2 test. Variables with P<0.1 were entered into subsequent multiple logistic regression analysis. Nonrelapse mortality at post-transplant day 100 (D100 NRM) and 5-year overall survival were calculated by the Kaplan–Meier method and compared by a log-rank test. The Cox proportional hazards regression model was used to assess the ability of number of metabolic abnormalities to predict D100 NRM or 5-year overall survival when grades III–IV acute GVHD and moderate-to-severe hepatic VOD were analyzed together because these variables were frequently associated with the occurrence of severe metabolic abnormalities.
Results
Frequencies of severe metabolic abnormalities within 100 days after HCT
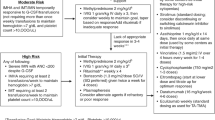
Of the 311 patients, 269 (86.5%) developed at least one severe metabolic abnormality within 100 days after allogeneic HCT (Figure 1). In all, 196 patients (63.0%) had one to three metabolic abnormalities, whereas 73 (23.5%) had four to seven abnormalities. Frequencies of individual abnormalities within 100 days after HCT were hypercalcemia in one patient (0.3%), hypocalcemia in one (0.3%), hypophosphatemia in 105 (33.8%), hyperkalemia in 25 (8.0%), hypokalemia in 149 (47.9%), hypernatremia in 13 (4.2%), hyponatremia in 185 (59.5%), hypermagnesemia in nine (2.9%), hypomagnesemia in 52 (16.7%), hypercholesterolemia in three (1.0%), hyperglycemia in 138 (44.4%), hypoglycemia in 12 (3.9%), and hyperuricemia in 22 (7.1%).
Risk factors associated with severe metabolic abnormalities
Pre-transplant patient and donor characteristics and post-transplant complications, such as acute GVHD and hepatic VOD, were analyzed for their association with severe metabolic abnormalities within 100 days after allogeneic HCT (Table 2). Multivariate analysis revealed that patients with moderate-to-severe hepatic VOD had significantly higher risk for the development of at least one abnormality after HCT (P=0.042; odds ratio (OR), 4.747; 95% confidence interval (CI), 1.060–21.259). Risk factors for each metabolic abnormality were also analyzed (Table 2). Grades III–IV acute GVHD was the most frequently associated with individual metabolic abnormalities, being an independent risk factor for the occurrence of hypophosphatemia (P<0.001; OR, 6.692; 95% CI, 2.913–15.373), hypernatremia (P=0.002; OR, 10.390; 95% CI, 2.344–46.049), hyponatremia (P=0.001; OR, 6.910; 95% CI, 2.284–20.900), hypermagnesemia (P=0.038; OR, 5.831; 95% CI, 1.100–30.894), and hyperglycemia (P<0.001; OR, 16.021; 95% CI, 5.827–44.049). Moderate-to-severe hepatic VOD was significantly associated with the occurrence of hyponatremia (P=0.009; OR, 2.808; 95% CI, 1.295–6.089), hyperglycemia (P=0.045; OR, 2.019; 95% CI, 1.017–4.009), and hyperuricemia (P<0.001; OR, 14.109; 95% CI, 6.008–33.133). When the donor–recipient pair was female–male, the incidence of hypophosphatemia (P=0.013; OR, 0.379; 95% CI, 0.176–0.817) was significantly lower and that of hyponatremia (P=0.020; OR, 2.193; 95% CI, 1.133–4.245) was significantly higher than observed with the other donor–recipient sex pairs. Patients with time from diagnosis to HCT of 140 days or more had significantly higher risk for the occurrence of hypophosphatemia (P=0.005; OR, 2.587; 95% CI, 1.341–4.990). When the status of the underlying disease was high risk at the time of HCT, hyperkalemia was significantly more frequent (P=0.002; OR, 5.288; 95% CI, 1.837–15.223). Age over 40 years (P=0.002; OR, 2.974; 95% CI, 1.477–5.989) and conditioning regimen (P=0.001) were additional risk factors for the occurrence of hyponatremia. When the conditioning regimens were compared, intravenous busulfan plus cyclophosphamide showed a significantly lower incidence of hyponatremia than oral busulfan plus cyclophosphamide (P<0.001; OR, 0.274; 95% CI, 0.135–0.558).
D100 NRM and overall survival according to the occurrence of severe metabolic abnormalities
For all patients, D100 NRM was 11.5%, and 5-year overall survival was 57.7%. Patients with at least one severe metabolic abnormality showed significantly higher D100 NRM (P=0.015) and lower 5-year overall survival (P=0.002) than those with no severe metabolic abnormalities (Table 3). Most individual metabolic abnormalities had significantly negative impacts on D100 NRM and overall survival. Hypophosphatemia (P=0.042 for D100 NRM, P=0.006 for overall survival), hyperkalemia (P<0.001 for D100 NRM, P<0.001 for overall survival), hypokalemia (P=0.001 for D100 NRM, P<0.001 for overall survival), hypernatremia (P<0.001 for D100 NRM, P<0.001 for overall survival), hyponatremia (P=0.004 for D100 NRM, P=0.001 for overall survival), hypermagnesemia (P<0.001 for D100 NRM, P=0.001 for overall survival), and hyperglycemia (P<0.001 for D100 NRM, P<0.001 for overall survival) were each significantly associated with higher D100 NRM and inferior overall survival. D100 NRM and overall survival differed significantly according to the number of severe metabolic abnormalities. Patients with no severe metabolic abnormality had a D100 NRM of zero, whereas those with one to three abnormalities had a D100 NRM of 7.3% and those with four to seven abnormalities had a D100 NRM of 29.6% (P<0.001, Figure 2a). The 5-year overall survival was 78.4% in patients with no metabolic abnormalities, 60.42% in those with one to three abnormalities, and 39.4% in those with four to seven abnormalities (P<0.001, Figure 2b). The Cox proportional hazards regression model showed that increasing number of severe metabolic abnormalities were independently associated with significantly inferior clinical outcomes in terms of D100 NRM (P=0.004) and 5-year overall survival (P=0.003) when grades III–IV acute GVHD and moderate-to-severe hepatic VOD were analyzed together (data not shown).
D100 nonrelapse mortality (D100 NRM) and overall survival differed significantly according to the number of severe metabolic abnormalities. (a) Patients without no abnormality had D100 NRM of zero, while those with one to three abnormalities had a D100 NRM of 7.3% and those with four to seven abnormalities had a D100 NRM of 29.6% (P<0.001). (b) The 5-year overall survival was 78.4% in patients with no abnormalities, 60.4% in patients with one to three abnormalities, and 39.4% in patients with four to seven metabolic abnormalities (P<0.001).
Discussion
We observed a high frequency of various metabolic abnormalities after allogeneic HCT, with 86.5% of patients having at least one severe metabolic abnormality. These abnormalities were associated with various risk factors, among which moderate-to-severe hepatic VOD and grades III–IV acute GVHD were the most frequent. Patients with hepatic VOD are liable to develop hyponatremia due to expansion of extracellular volume, use of diuretics, and impairment of renal function. Secretion of inappropriate antidiuretic hormone has also been reported to cause hyponatremia in HCT recipients and it has been found to be a side effect of conditioning therapy, especially with cyclophosphamide.1,2 Acute GVHD can cause various metabolic derangements because it requires systemic immunosuppressive treatments, which may be complicated by gastrointestinal symptoms or severe infections. Cyclosporine and tacrolimus, the most widely used immunosuppressants for the prophylaxis and treatment of GVHD, have been associated with hyperkalemia,3,4,13,14 hyperglycemia,3,4,15,16 hypomagnesemia,17,18,19 and hypertriglyceridemia20,21 in HCT recipients. Glucocorticoid, another frequently used immunosuppressant for GVHD, also causes hyperglycemia.5,22 Acute GVHD was the major indication for the use of glucocorticoid in our study. Other than hepatic VOD and acute GVHD, the occurrence of severe metabolic abnormalities were also associated with age (hyponatremia), duration of disease before HCT (hypophosphatemia), disease status at the time of HCT (hyperkalemia), type of donor (hyponatremia), donor–recipient sex pair (hypophosphatemia, hyponatremia), and conditioning regimen (hyponatremia). Presence of severe metabolic abnormalities may reflect various underlying conditions on the whole.
Gastrointestinal symptoms such as vomiting or diarrhea can cause electrolyte disturbances, and inflammatory or infective processes may lead to insulin resistance by increasing tumor necrosis factor (TNF)-α.23 Pentamidine, which is used for the prevention or treatment of pneumocystis pneumonitis, may cause acute release of insulin due to pancreatic β cell damage, resulting in severe hypoglycemia followed by hyperglycemia.24 There was a case report of hypoglycemia induced by antibodies to insulin receptor following HCT.25 Although TPN is important in supportive therapy of patients undergoing HCT, it is frequently associated with various metabolic abnormalities, especially electrolyte and glucose disturbances.6,7 We could not analyze the role of TPN use in metabolic abnormalities in our study, however, because almost all our patients received TPN during the early post-transplant period.
Hypophosphatemia is a common abnormality after HCT,26 with 33.8% of our patients developing severe hypophosphatemia. Increased phosphate uptake by replicating neutrophils during the peri-engraftment period is thought to play a role in the occurrence of hypophosphatemia in HCT recipients.27,28,29 Hypokalemia was also frequently encountered after HCT. This condition may be due to renal potassium wasting, which may result from long-term use of aminoglycoside antibiotics and amphotericin B, concomitant hypomagnesemia, and vomiting. Disturbances of calcium or lipids, which have been rarely reported in patients undergoing HCT,30,31,32 were also uncommon (1.0% or less) in our study. Hypomagnesemia was relatively frequent (16.7%), whereas hypermagnesemia was infrequent (2.9%). A case of hypermagnesemia was reported as a complication of antacid administration after HCT.33
Severe metabolic abnormalities were associated with inferior clinical outcomes, as determined by D100 NRM and overall survival. It is unlikely that the higher nonrelapse mortality in patients with metabolic abnormalities resulted from direct effects of these abnormalities. No metabolic abnormality was recorded as cause of death in any patient included in this study. The poor prognosis of patients with metabolic abnormalities may be due to underlying serious problems, such as acute GVHD and hepatic VOD, both of which were significantly associated with the occurrence of severe metabolic abnormalities. However, increasing number of metabolic abnormalities showed independently significant adverse impact on D100 NRM and overall survival when grades III–IV acute GVHD and moderate-to-severe hepatic VOD were analyzed together. The number of metabolic abnormalities also stratified the patients with different clinical outcomes. These results suggest that metabolic abnormalities during the early post-transplant period may serve as prognostic indicators for patients undergoing allogeneic HCT.
In conclusion, severe metabolic abnormalities within 100 days of allogeneic HCT were common, and the presence of those abnormalities was significantly associated with inferior clinical outcomes. These findings suggest that metabolic parameters should be monitored in the patients undergoing allogeneic HCT, and that metabolic abnormalities should be considered an important toxicity parameter in prospective clinical trials regarding allogeneic HCT.
References
Chisholm DJ . Endocrine abnormalities. In: Atkinson K (ed.). Clinical Bone Marrow and Blood Stem Cell Transplantation, 2nd edn. Cambridge University Press: Cambridge, UK, 2000; pp 980–987.
Abe T, Takaue Y, Okamoto Y et al. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) in children undergoing high-dose chemotherapy and autologous peripheral blood stem cell transplantation. Pediatr Hematolol Oncol 1995; 12: 363–369.
Przepiorka D, Khouri I, Ippoliti C et al. Tacrolimus and minidose methotrexate for prevention of acute graft-versus-host disease after HLA-mismatched marrow or blood stem cell transplantation. Bone Marrow Transplant 1999; 24: 763–768.
Woo M, Przepiorka D, Ippoliti C et al. Toxicities of tacrolimus and cyclosporin A after allogeneic blood stem cell transplantation. Bone Marrow Transplant 1997; 20: 1095–1098.
Van Lint MT, Uderzo C, Locasciulli A et al. Early treatment of acute graft-versus-host disease with high- or low-dose 6-methylprednisolone: a multicenter randomized trial from the Italian Group for Bone Marrow Transplantation. Blood 1998; 92: 2288–2293.
Muscaritoli M, Conversano L, Torelli GF et al. Clinical and metabolic effects of different parenteral nutrition regimens in patients undergoing allogeneic bone marrow transplantation. Transplantation 1998; 66: 610–616.
Szeluga DJ, Stuart RK, Brookmeyer R et al. Nutritional support of bone marrow transplant recipients: a prospective, randomized clinical trial comparing total parenteral nutrition to an enteral feeding program. Cancer Res 1987; 47: 3309–3316.
McDonald GB, Hinds MS, Fisher LD et al. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med 1993; 118: 255–267.
Bearman SI . The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood 1995; 85: 3005–3020.
Tutschka PJ, Beschorner WE, Hess AD, Santos GW . Cyclosporin-A to prevent graft-versus-host disease: a pilot study in 22 patients receiving allogeneic marrow transplants. Blood 1983; 61: 318–325.
Przepiorka D, Weisdorf D, Martin P et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Johnson KR, Mascall GC, Howarth AT . Differential laboratory diagnosis of hypercalcemia. Crit Rev Clin Lab Sci 1984; 21: 51–97.
Fleming DR, Ouseph R, Herrington J . Hyperkalemia associated with cyclosporine (CsA) use in bone marrow transplantation. Bone Marrow Transplant 1997; 19: 289–291.
Caliskan Y, Kalayoglu-Besisik S, Sargin D, Ecder T . Cyclosporine-associated hyperkalemia: report of four allogeneic blood stem-cell transplant cases. Transplantation 2003; 75: 1069–1072.
Yanik G, Levine JE, Ratanatharathorn V et al. Tacrolimus (FK506) and methotrexate as prophylaxis for acute graft-versus-host disease in pediatric allogeneic stem cell transplantation. Bone Marrow Transplant 2000; 26: 161–167.
Nash RA, Pineiro LA, Storb R et al. FK506 in combination with methotrexate for the prevention of graft-versus-host disease after marrow transplantation from matched unrelated donors. Blood 1996; 88: 3634–3641.
June CH, Thompson CB, Kennedy MS et al. Correlation of hypomagnesemia with the onset of cyclosporine-associated hypertension in marrow transplant patients. Transplantation 1986; 41: 47–51.
June CH, Thompson CB, Kennedy MS et al. Profound hypomagnesemia and renal magnesium wasting associated with the use of cyclosporine for marrow transplantation. Transplantation 1985; 39: 620–624.
Kone BC, Whelton A, Santos G et al. Hypertension and renal dysfunction in bone marrow transplant recipients. Q J Med 1988; 69: 985–995.
Carreras E, Villamor N, Reverter JC et al. Hypertriglyceridemia in bone marrow transplant recipients: another side effect of cyclosporine A. Bone Marrow Transplant 1989; 4: 385–388.
Valbonesi M, Occhini D, Frisoni R et al. Cyclosporin-induced hypertriglyceridemia with prompt response to plasma exchange therapy. J Clin Apheresis 1991; 6: 158–160.
Matsuoka S, Okamoto S, Watanabe R et al. Granisetron plus dexamethasone versus granisetron alone in the prevention of vomiting induced by conditioning for stem cell transplantation: a prospective randomized study. Int J Hematol 2003; 77: 86–90.
Hotamisligil GS, Peraldi P, Budavari A et al. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science 1996; 271: 665–668.
Bouchard P, Sai P, Reach G et al. Diabetes mellitus following pentamidine-induced hypoglycemia in humans. Diabetes 1982; 31: 40–45.
Rochet N, Blanche S, Carel JC et al. Hypoglycaemia induced by antibodies to insulin receptor following a bone marrow transplantation in an immunodeficient child. Diabetologia 1989; 32: 167–172.
Crook M, Swaminathan R, Schey S . Hypophosphataemia in patients undergoing bone marrow transplantation. Leuk Lymphoma 1996; 22: 335–337.
Steiner M, Steiner B, Wilhelm S et al. Severe hypophosphatemia during hematopoietic reconstitution after allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant 2000; 25: 1015–1016.
Raanani P, Levi I, Holzman F et al. Engraftment-associated hypophosphatemia—the role of cytokine release and steep leukocyte rise post stem cell transplantation. Bone Marrow Transplant 2001; 27: 311–317.
Uckan D, Cetin M, Dida A et al. Hypophosphatemia and hypouricemia in pediatric allogeneic bone marrow transplant recipients. Pediatr Transplant 2003; 7: 98–101.
Montoliu J, Macia J, Salamero P et al. Severe hypercalcemia indicating relapse of acute myelocytic leukemia after bone marrow transplantation. Nephron 1992; 62: 357–358.
Toren A, Nagler A . Solitary pulmonary cholesteroloma, multiple xanthelasmas and lipemia retinalis complicating hypercholesterolemia after bone marrow transplantation. Bone Marrow Transplant 1996; 18: 457–459.
Lin J, Markowitz GS, Nicolaides M et al. Membranous glomerulopathy associated with graft-versus-host disease following allogeneic stem cell transplantation. Report of 2 cases and review of the literature. Am J Nephrol 2001; 21: 351–356.
Jaing TH, Hung IJ, Chung HT et al. Acute hypermagnesemia: a rare abnormality of antacid administration after bone marrow transplantation. Clin Chim Acta 2002; 326: 201–203.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JH., Choi, SJ., Lee, JH. et al. Severe metabolic abnormalities after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 35, 63–69 (2005). https://doi.org/10.1038/sj.bmt.1704708
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704708
Keywords
This article is cited by
-
Low urinary sodium-to-potassium ratio in the early phase following single-unit cord blood transplantation is a predictive factor for poor non-relapse mortality in adults
Scientific Reports (2024)
-
Prolonged versus short infusion rates for intravenous magnesium sulfate administration in hematopoietic cell transplant patients
Supportive Care in Cancer (2018)
-
Impact of intravenous magnesium infusion rate during ambulatory replacements on serum magnesium concentrations after allogeneic stem cell transplant
Supportive Care in Cancer (2016)
-
Brain imaging findings in symptomatic patients after allogeneic haematopoietic stem cell transplantation: correlation with clinical outcome
European Radiology (2012)
-
Blood and marrow transplantation and nutritional support
Supportive Care in Cancer (2010)