Key Points
-
Provides an understanding of alloys used in dentistry.
-
Outlines NHS regulations relevant to the use of materials in cast restorations.
-
Discusses cost and material differences between alloys used in dentistry.
-
Provides an awareness of appropriate alloys to use in dental restorations.
-
Compares clinical and technical qualities of different alloys to aid treatment planning.
Abstract
Background Gold alloy has long been used in dentistry for the fabrication of cast restorations due to its material and clinical properties and known excellent longevity over long-term follow-up. The cost of gold has increased dramatically in recent years (by 450% in the past ten years). The use of base metal alloys as an alternative would lead to a considerable cost saving: a cobalt chromium alloy is around 98% cheaper than gold alloy at the time of writing. NHS regulations state which alloys are permissible for use in cast restorations in dentistry, and certain 'non-precious gold' alloys should not be used.
Materials and methods A prospective audit was carried out in our unit into the standard of cast restorations in cobalt-chromium alloy. The standard set before the audit was established by a prior audit of gold alloy restorations with measures of clinical and technical factors.
Results Base-metal alloy restorations were considerably cheaper; but were of a poorer clinical standard than gold-alloy and required more frequent adjustment and remake (17% compared to 5%).
Similar content being viewed by others
Introduction
Material selection of a cast restoration is derived from the collaborative decision of the dentist and patient. The need to consider several factors, such as quality, aesthetics and cost, can at times make this decision challenging. This paper aims to review the alloys used for cast restorations, the current NHS regulations and describes an audit on the quality of base metal cast restorations, which was conducted following a proposal to switch to base metal alloy from gold.
Alloys
Metal alloys have long been used in dentistry, both in wrought forms (for example, wires, endodontic files, implants) and via casting for inlays, onlays, crowns, bridges and denture frameworks.1 Alloys may contain noble (precious) or base (non-precious) metals, and can be classified accordingly (Table 1). Noble metals are defined by their resistance to corrosion, which is desirable in dentistry due to the extreme conditions within the mouth. Inclusion of base metals is required to provide adequate strength, flexibility and wear resistance. Gold, palladium and platinum are noble metals used in dentistry. The most commonly used base metals include titanium, cobalt, chromium, silver, zinc, tin and nickel.
Noble metal alloys
Gold is traditionally used in cast restorations because of its excellent corrosion resistance, good malleability and relatively low melting point (1,064°C).1 Historically, cast restorations have been fabricated using ADA specification high-gold alloy,2 containing at least 40% gold and 60% total noble metal. These were categorised according to their content of gold versus base metal (Table 2). High gold content improves the reliability and accuracy of casting via improved penetration into the mould, and its higher density (18 g/cm3 or more) allows gravity to accelerate the molten metal more readily into the casting mould under centrifugal forces.1,2
Anecdotally, cast gold restorations are known for their excellent longevity. However, there is little robust evidence in this respect and studies in relation to survival rates vary in quality. It has been shown that 90%, 72% and 45% of gold restorations survive for over nine, 20 and 25 years respectively.5
Base metal alloys
Base metal alloys commonly used in dentistry include nickel-chromium (NiCr), cobalt-chromium (CoCr), stainless steel and titanium alloys. NiCr alloys were introduced in the 1930s as a lower-cost alternative to gold alloy,6 though are now used less due to concerns regarding biocompatibility.
Cobalt-chromium alloy
Cobalt-chromium alloys have been used in dentistry since 1929 in removable denture frameworks and more recently in cast restorations.6
Cobalt increases the elastic modulus and strength of an alloy. Chromium provides resistance to tarnish and corrosion, although above 29% in an alloy can lead to brittleness and difficulty in casting.6 CoCr alloys exhibit better corrosion resistance than NiCr alloys.6
The CoCr alloy used in cast restorations in this audit is Heraenium® Pw, which has been used for some time as the bonding alloy for resin-retained bridges. It should be noted that an alloy of different composition (Sheralit-Cylindra, Shera GMBH & Co, Espohlstrasse 53, Lemforde, Germany) is used for removable denture frameworks, which is harder, more rigid and has a lower tensile strength.7 A comparison of these alloys is detailed in Table 3.
Alloy selection
Material properties
Base metal alloys, in comparison to gold, have:
-
A higher modulus of elasticity (that is, are more rigid)2
-
Very high yield strength (level of force required to permanently distort a material)1
-
Greater hardness (resistance to indentation)1 which makes these alloys harder to polish and adjust, but resistant to wear in function
-
Relatively low density; which reduces the ease of casting.
Biocompatibility
Base metal alloys have been associated with concerns regarding contact dermatitis (a localised reaction of the skin or mucosa associated with repeated contact with a material). Nickel is a common cause of contact dermatitis. Nickel allergy affects up to 20% of females and 2% of males, although there are few reports of reactions to dental restorations.9
Chromium does not cause adverse reactions in its metal form. Although allergy to chromium-containing compounds does occur, chromium alloys do not usually cause a reaction.9
Gold and cobalt are generally regarded as biocompatible, although confirmed sensitivity has been reported.9
Costs of gold
Up to the end of 2011, it is estimated that 171,300 metric tonnes of gold have ever been mined, with 165,000 tonnes of stock in existence today: this is sufficient only to form a cube with sides measuring 20 metres.10 More than half was extracted within the last 50 years; around 2,500 metric tonnes are currently mined annually.11 Of the demand for gold, 55.3% is for jewellery; 32.7% for investments and 12.0% is for technology (including dentistry).10
There has been an upward trend in the market price of gold, with an approximately 450% increase since 2003.12 Gold alloy for use in dental castings has also increased in price. In January 2013, 60% gold alloy used in our dental laboratory cost £24.49/g, compared to £8.34/g in 2006. In comparison, CoCr alloy cost £0.47/g; 98% cheaper than gold alloy.
'Non-precious gold' alloy
Yellow base metal alloys containing copper, aluminium, zinc and nickel are available, oxymoronically marketed as 'non-precious gold.' These alloys tarnish readily and anecdotally may have an adverse taste. These are available in the UK and through overseas laboratory services, and while the alloy possesses a CE mark, their use is not permitted in the UK under NHS regulations.13
NHS regulations
The NHS charges regulations in England and Scotland specify the alloys that may be used in each type of cast restoration in dentistry (Table 4).13,14,15 The use of other alloys technically constitutes a breach of contract under the new NHS regulations. It should be noted that the use of non-precious alloys is only permissible in full-coverage restorations and resin-retained bridges.
There has been some negative UK press coverage16 regarding the use of inappropriate alloys in dentistry. Statements have been made by the Chief Dental Officer, Mr Barry Cockcroft,17 and by Mr John Stacey, President of the Dental Technologists Association,18 reiterating that the use of alloys such as 'non-precious gold' would constitute a breach of NHS contract. Dental technicians, as GDC registrants, should not offer or agree to fabricate restorations using inappropriate alloys under the NHS.
When providing metal crowns, the alloy used must be clear to the patient, in their records and through the NHS fee claim. The restoration claimed or charged for must contain an alloy appropriate to the regulations. Technicians must maintain a documented record of the non-precious or precious metals used in the fabrication of a restoration.18
It should be noted that these regulations apply to NHS treatment only, not to restorations provided privately.
Overseas laboratories
There has been a recent increase in the use of overseas laboratory services, such as those in China. Work provided outside the UK may be cheaper, but some evidence suggests that the gold alloy requested may not be provided, and that the cobalt-chromium alloy may contain small amounts of nickel.19
Alloy use
NHS dental hospital budgets are largely fixed, but expenditure continues to increase, for example due to increasing costs of gold, leading to exercises to reduce expenses.
To the authors' knowledge, there are currently no published studies investigating all-metal cast CoCr crowns. A retrospective study, based in dental practice, evaluated the clinical performance of CoCr-based metal-ceramic crowns and found a 90.3% 5-year survival rate.20 Of these, 2% failed through loss of the crown and 1% through caries. Other modes of failure included porcelain fracture, which is not applicable to all-metal crowns. This study did not include a control group, so comparison with other alloys could not be drawn; although the author concluded that CoCr alloys are a 'promising alternative' to other alloys.
No comparison or evaluation of marginal fit of CoCr alloy crowns could be found. Older studies21,22 have found that gold alloys (particularly high-gold) exhibit better marginal fit than base metal alloys including NiCr.
Audit within a UK dental institute
Background
Within the Restorative Department of the Leeds Dental Institute, it was proposed that cobalt-chromium (CoCr) alloy should be used instead of the traditionally-used gold alloy (Au) for full-coverage restorations. This change was proposed on the basis of cost: a move away from gold alloy would result in a considerable saving of tens of thousands of pounds per year. For quality control it was thought important to audit non-precious restorations, and reference this to the quality of gold restorations.
Audit standards
There are no published standards for cast restorations; so an audit of Au restorations was done to set a standard before the introduction of the CoCr alloy. A number of subjective clinical and technical qualities were audited. Restorations fabricated from CoCr alloy were then audited in terms of the same qualities, and the results compared against the standards for Au alloy. A repeat audit of the non-precious alloy was done six months later.
Method
The audit was carried out prospectively, and included all consecutive cast all-metal restorations prescribed by staff, postgraduate and undergraduate students within the restorative department. The restorations were fabricated by qualified dental technicians.
Assessment was via questionnaires completed by the technician fabricating the restoration and by the clinician prescribing and fitting it. A number of qualities were subjectively assessed as adequate or inadequate, as well as a record of the following: whether any adjustment or remake was required; the time taken for fabrication or fitting the restoration and the cost of alloy used (Table 5). Fifty-one consecutively prescribed Au restorations fabricated within the laboratory were included in the initial audit, followed by 48 consecutive restorations in CoCr alloy.
Results
Fifty-one technician questionnaires were completed for Au restorations and 48 for CoCr. Forty-two clinician questionnaires were returned for Au restorations (82% response rate) and 35 for CoCr (73% response rate). A further cycle of the audit was carried out six months later, as it was felt that the 'learning curve' associated with the use of the new alloy may account for some of the errors in casting (see below). In the re-audit, 50 questionnaires were completed by technicians (100% response rate) and 42 by clinicians (84% response rate).
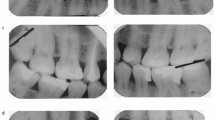
The results of the Technician feedback are detailed in Table 6. The results of the clinician feedback are detailed in Table 7 and summarised in Figure 1.
Cost
The mean cost of CoCr restorations was £1.10 (range £0.45-1.85) in the first audit cycle, and £1.19 (range £0.56-2.24) in the re-audit, compared to a mean cost of £83.80 for Au (range £38.20-141.06).
Technical standards
Au and CoCr restorations appeared to be of the same technical standard except for casting errors: no casting errors occurred with Au, compared to 6% (n = 3) with CoCr; with 2% (n = 1) of CoCr restorations requiring remake in the first cycle. The technical staff felt that these errors were at least partly related to the use of a new alloy, such as selection of incorrect sprue size or casting porosity; and indeed there were no casting errors in the second audit cycle.
Clinical standards
The reported standards of all clinical properties of CoCr restorations were poorer than those of Au in the first cycle with the exception of occlusal detail. In the second cycle, some properties were improved but still remained poorer than that of gold, except that fewer restorations required adjustment.
Adjustment of restorations
Chair-side adjustment was required for 50% (n = 20) of Au restorations, and reported to be difficult in 5% (n = 1). In the first audit cycle, 66% (n = 19) of CoCr restorations required adjustment, reported to be difficult in 16% (n = 3).
Posters were displayed in clinical areas to provide information on suitable burs to use for adjustment of the alloy. Suitable burs include fine diamond polishing burs and polishing burs such as tungsten carbide finishing burs and the Ceramisté polisher (Shofu Dental Corporation, 1225 Stone Drive, San Marcos, CA, USA).
In the second cycle, fewer crowns required adjustment (40%) (n = 17), where 24% (n = 4) reported difficulty. This figure was less than that reported for gold alloy.
Remake
Remake on clinical grounds was more frequently needed with CoCr: in the first cycle 17% (n = 6) and in the second cycle 18% (n = 7) of crowns had to be remade compared to 5% of Au (n = 2).
Appearance
The two negative comments (6%) from patients in the first CoCr cycle related to appearance. One of these crowns was remade in gold and the other was fitted. In the second cycle, 7% (n = 3) of patients made negative comments regarding the appearance of CoCr restorations. Two of these patients had their crowns remade, one in gold and one in metal ceramic. The other patient stated they would have preferred a gold crown but allowed the base metal one to be fitted. There were no negative comments about the appearance of the gold restorations.
Discussion
An audit can only provide low-level evidence; this was not a randomised controlled trial. The restorations were fabricated and assessed by a number of technicians, and clinicians ranged from undergraduate students to consultants in restorative dentistry. There was no attempt to look at quality of tooth preparation or to standardise assessment.
Long-term randomised controlled clinical trials would obviously provide better evidence on which to base decision-making, but the authors are not aware of any at present; and feel that this audit can provide a starting point for discussion. This audit can provide a subjective guide to quality of the restoration at fit, but there still remains no data on longevity of these restorations in use.
Undeniably, the use of base-metal alloys is considerably cheaper than gold. However, the cost associated with more frequent remake should also be considered: including the cost of clinical and laboratory time, in addition to the extra alloy. There were some technical problems associated with the use of the base-metal alloy, although these could be attributed to the use of a new alloy, as they were not seen in the second audit cycle.
It is interesting to note that while the technician feedback reported that marginal fit on the model was satisfactory in all restorations, clinician feedback reported that this was the case in only 98% (n = 41) of Au and 89% (n = 31) of CoCr restorations in the first cycle and 95% (n = 38) in the re-audit. The reasons for this discrepancy are difficult to ascertain and would require further data collection. However, as the technician fabricating the restoration assessed it, there is a likelihood of bias.
In the current economic climate, cost-effectiveness must be considered. However, this needs to be in conjunction with good clinical practice, and take account of clinical and technical time required: not just the material costs. It is essential that practitioners and technicians are aware of the NHS regulations and work accordingly within them. In the first cycle of the CoCr audit, 4% (n = 2) of the CoCr restorations fabricated were three quarter coverage or onlays and in the second cycle 4% (n = 2) were three quarter or seven eighth crowns.
The NHS regulations permit these restorations to be fabricated from gold alloy only in the general dental services. This serves as emphasis of the need for awareness of the relevant NHS regulations.
Conclusions
CoCr alloy restorations were not of as high a standard as gold-alloy. While more frequent remake was initially required, this limitation appears to resolve with experience. While clinicians found adjustment of CoCr alloy more difficult than gold, the use of appropriate burs should facilitate this.
Restorations fabricated from base-metal are significantly cheaper than gold-alloy.
The use of cheap but inappropriate alloys must be avoided, and members of the dental team should be aware of the relevant NHS regulations relating to the use of alloys in practice.
Further investigation of alternative alloys to gold is desirable in order to provide a high-quality evidence base.
References
Powers J M W, Wataha J C . Dental materials, properties and manipulation. 10th ed. Missouri, USA: Elsevier, 2012.
Wassell R W, Walls A W, Steele J G . Crowns and extra-coronal restorations: materials selection. Br Dent J 2002; 192: 199–202, 205–211.
McCabe J F, Walls A W . Applied dental materials. 9 ed. Oxford: Blackwell Publishing, 2008.
International Organization for Standardization. Dentistry - metallic materials for fixed and removable restorations and appliances. ISO, 2006.
Donovan T, Simonsen R J, Guertin G, Tucker R V . Retrospective clinical evaluation of 1,314 cast gold restorations in service from 1 to 52 years. J Esthet Restor Dent 2004; 16: 194–204.
Roach M . Base metal alloys used for dental restorations and implants. Dent Clin North Am 2007; 51: 603–627.
Durham K F, Sackley C M, Wright C C, Wing A M, Edwards MG, van Vliet P . Attentional focus of feedback for improving performance of reach-to-grasp after stroke: a randomised crossover study. Physiotherapy 2014; 100: 108–115.
Heraenium materials data booklet. 2011.
Wiltshire W A, Ferreira M R, Ligthelm A J . Allergies to dental materials. Quintessence Int 1996; 27: 513–520.
World Gold Council. Facts about gold. World Gold Council, 2010. Online facts available at www.gold.org/about_gold (accessed July 2014).
The real price of gold. National Geographic, 2009.
Kitco. Online information available at www.kitco.com. (accessed July 2013).
Scottish Government Health and Social Care Directorate. Statement of dental remuneration amendment, amendment no. 118. NHS Scotland, 2010. Online statement available at http://www.sehd.scot.nhs.uk/pca/PCA2010(D)08SDR.pdf (accessed July 2014).
National Health Service England. The National Health Service (dental charges) regulations 2005. NHS, 2005 Online regulations avilable at http://www.legislation.gov.uk/uksi/2005/3477/schedule/3/made (accessed July 2014).
National Health Service England. The National Health Service (dental charges) amendment regulations 2006. No. 1837. NHS, 2006.
Lakhani N . Dental patients put at risk by banned fake-gold implants. The Independent, 2010. Online article available at http://www.independent.co.uk/life-style/health-and-families/health-news/dental-patients-put-at-risk-by-banned-fakegold-implants-1999198.html (accessed July 2014).
Cockcroft B . The use and misuse of non-precious gold in restorations. CDO Update, 2010: 4.
Providing clarification on materials confusion. Online article available at http://www.dentalrepublic.co.uk/the-probe/blog/providing-clarification-on-materials-confusion/page/blog-list/2 (accessed July 2013).
Ekblom K, Smedberg J I, Moberg L E . Clinical evaluation of fixed partial dentures made in Sweden and China. Swed Dent J 2011; 35: 111–121.
Ortorp A, Ascher A, Svanborg P . A 5-year retrospective study of cobalt-chromium-based single crowns inserted in a private practice. Int J Prosthodont 2012; 25: 480–483.
Tjan A H, Li T, Logan G I, Baum L . Marginal accuracy of complete crowns made from alternative casting alloys. J Prosthet Dent 1991; 66: 157–164.
Nitkin D A, Asgar K . Evaluation of alternative alloys to type III gold for use in fixed prosthodontics. J Am Dent Assoc 1976; 93: 622–629.
Acknowledgements
The authors would like to thank Mr Anthony Cox, Chief Technician at the Leeds Dental Institute, for his help with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beddis, H., Ridsdale, L., Chin, J. et al. An audit of the quality of base metal cast restorations provided within the restorative department of a UK dental institute. Br Dent J 217, E11 (2014). https://doi.org/10.1038/sj.bdj.2014.855
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.855