Key Points
-
Describes the risks and complications associated with the new anticoagulants.
-
Explains the mechanism of action to allow a better understanding of how they work.
-
Discusses the modifications required for treatment in general dental practice.
-
Explains the extra care required when undertaking dental treatment.
Abstract
All clinicians, whether in primary or secondary care settings, are likely to encounter patients on this new anticoagulant. Therefore, it is imperative that clinicians are aware of the risks and benefits associated with dabigatran.
Similar content being viewed by others
Introduction
In the UK, up to 800,000 people have been diagnosed with atrial fibrillation1 (AF) and may be prescribed warfarin for its management. AF is the most common heart arrhythmia affecting 10% of those over 75 years of age in the UK. It is a potentially dangerous arrhythmia due to the absence of organised atrial contraction, promoting blood stasis in the atria, which in turn increases the risk of thrombus formations particularly in the left atrial appendage. This poses a significant risk factor for the development of a stroke.2
Dabigatran (Pradaxa®) is a recently licensed anticoagulant that decreases the risk of stroke or systemic emboli in patients with AF, and those undergoing joint replacement surgery, when compared with warfarin, as shown in the Randomised Evaluation of Long Term Anticoagulant Therapy (RE-LY) study.3 It is currently only licensed for the treatment of AF and joint replacement surgery. It is indicated in adult patients with non-valvular AF, which is defined as a disruption in the rhythm of the heart which is not associated with the valves and who have one or more of the following risk factors:4
-
Previous stroke
-
Transient ischaemic attack (TIA) or systemic embolism
-
Left ventricular ejection fraction <40%
-
Symptomatic heart failure > New York heart association class 2, which indicates the patient is slightly symptomatic with ordinary activities but is comfortable at rest5
-
Age >65 associated with one of the following: diabetes mellitus (DM), coronary artery disease (CAD), hypertension (HTN).
With such significant numbers of patients being treated for AF in the UK, general dental practitioners will be faced with the prospect of managing patients taking either warfarin or dabigatran in the immediate future. Understanding how to treat this specific category of patients in the primary care setting is therefore extremely important.
Mechanism of Action
It is important to consider the pharmacology of both warfarin and dabigatran as this may directly influence the patient's management.
Warfarin acts on the vitamin K dependent clotting factors, factor II, VII, IX and X, as well as protein C, S and Z. Warfarin and related 4-hydroxycoumarin-containing molecules decrease blood coagulation by inhibiting vitamin K epoxide reductase. This enzyme recycles oxidised vitamin K to its reduced form after it has taken part in the carboxylation of several blood coagulation proteins, mainly factor II (prothrombin) and factor VII. The clotting factors that are produced by the liver take between 24–48 hours before they are naturally metabolised by the body. This accounts for warfarin's 48 hour delay in mechanism of action.
Dabigatran acts by directly inhibiting thrombin in the coagulation cascade, thus preventing clot formation by inhibiting the conversion of fibrinogen to fibrin, during the common coagulation pathway. Free thrombin, clot bound thrombin and thrombin-induced platelet aggregation are inhibited by the active molecules. Thrombin also activates coagulation factors V, VIII and XI as part of a feedback loop, generating more thrombin and activating factor XIII which stabilise the clot by cross linking fibrin. Dabigatran takes two to three days to have the full required anti-thrombin effect and is excreted renally, primarily in urine.6
At the recommended therapeutic dose, dabigatran prolongs the coagulation markers such as the activated partial thromboplastin time (APTT), ecarin clotting time which is a laboratory test to measure the anticoagulation time for direct thrombin inhibitors, and thrombin time.7 International normalised ratio (INR) is relatively insensitive to dabigatran exposure and cannot be used to monitor therapeutic levels as it would with warfarin. Dabigatran prolongs the activated prothrombin and thrombin time with no effect on vitamin K dependent clotting factors8 (Fig. 1).
At therapeutic doses, dabigatran has been shown to prolong the activated prothrombin time (APTT), ecarin clotting time and thrombin time. The RELY study3 has shown that the standard dose increases the median value of APTT two-fold. In healthy fasting individuals, the maximum serum concentration (cmax) was reached in one hour. In individuals who have ingested a high fat content when taking the drug, the cmax is reached in two hours.6,8
The overall bioavailability of dabigatran is 3–7%. This is not altered by the timing of ingestion. However, it is worth noting that should the capsule be crushed or active ingredient removed from its capsule, the bioavailability increases to 75%.6,9 Therefore, it is imperative that the outer shell of the capsule remains intact. If the outer layer is damaged, this may lead to an unintentional overdose. This may be even more significant as there is no proper reversal pathway.
Dabigatran prolongs the activated prothrombin and thrombin time with no effect on vitamin K dependent clotting factors. Decisions on when to stop dabigatran pre-surgery are based on creatinine clearance and supplemented with a coagulation screen. When compared to warfarin use, dabigatran has many beneficial aspects. The initial effects of dabigatran occur in hours rather than days and are more predictable than that of warfarin. There are few interactions with other medications and food, negating the need for monitoring.
Dosing
Warfarin dosing should be prescribed on an individual basis. Each patient has the potential to react differently to the same dosing regime and therefore caution and careful monitoring is required when prescribing.
Patients commencing warfarin initially start with a loading dose regime. They receive high doses of warfarin, usually 10 mg for the first two days with the dose being titrated according to their international normalised ratio (INR). It is worth noting that it takes 48 hours for a dose to be therapeutic. Once a therapeutic INR is reached, a maintenance dose of warfarin is prescribed. This is dictated by how the individual patient has responded to the previous doses. The patient then requires their INR to be checked on a regular basis, usually every one to two weeks. Particular care is required when patients commence other medications or develop other medical conditions. If this occurs, the effects of warfarin can no longer be predicted and the patient can end up with a higher or lower INR than desired while taking their normal dosage, therefore highlighting the need for monitoring.
It is important to note that certain commonly used drugs can interact with warfarin leading to an increased INR. These include all antibiotics, especially metronidazole and clarithromycin, which reduce warfarin metabolism. Broad spectrum antibiotics can reduce normal bacterial flora in the gut, altering vitamin K levels. Certain food and drink, such as alcohol and cranberry juice, also affect warfarin metabolism which can lead to non-therapeutic or a raised INR. It is worthwhile, before undertaking surgical procedures, to enquire about any change to the patient's diet or medications.
Dosing of dabigatran is simpler to manage and is dictated by the patient's creatinine clearance (CrCl), a measure of the renal function and the patient's age. Creatinine clearance is calculated using the patient's age, weight and creatinine level. Creatinine clearance varies with renal function.
In a normal healthy individual the recommended daily dose of dabigatran is 300 mg, taken as a 150 mg capsule twice daily. If the patient is over 80 years of age with a normal CrCl, the dose should ideally be 220 mg daily, taken as a 110 mg capsule twice daily. If the patient has a CrCl of 30–50 ml/min, 300 mg daily is still the recommended dose. If the CrCl is between 15–30 ml/min then the dose should be decreased to 220 mg daily. For CrCl under 15 ml/min, dabigatran is contraindicated. This is summarised in the Table 1.8
A reduced dose of dabigatran should be prescribed in certain groups of patients deemed high risk, including patients receiving verapamil or those who suffer from gastritis, oesophagitis or gastrooesophageal reflux. In these cases the dose should be reduced to 220 mg per day.11
Invasive Procedures
An important consideration with both warfarin and dabigatran is when to stop them before surgical procedures.
When considering warfarin, the most important factor in deciding whether extraction of teeth or surgical procedures can be completed in the primary care setting is the INR. The British Committeee for Standards in Haematology released guidelines in 2007 stating that patients with a stable INR of less than four could be safely treated in general practice for simple dental procedures. However, it is recommended that local guidelines are consulted before undertaking such treatment.12
If the surgical procedures are required for patients with mechanical heart valves warfarin may need to be stopped before surgery and alternative anti-coagulation prescribed. The medical indication for taking warfarin will dictate whether a substitute is required, such as a heparin infusion in order for anticoagulation to be tightly controlled. Warfarin can then be restarted once haemostasis has been achieved and the heparin infusion ceased once the therapeutic INR has been achieved.
Use of dabigatran in patients undergoing dental treatment requires careful consideration. It is recommended that routine dental treatment, including up to three extractions may be carried out in general practice without any adjustment to dabigatran dose.13 However, it does advise that the post-operative risk of bleeding should be considered alongside the thromboembolic risk. The guidelines also recommend the following post-operative measures to minimise the risk of haemorrhage:
-
The procedure should ideally be performed 12 hours after the last dose
-
The procedure should be performed with the least amount of trauma
-
The post-operative wound should be sutured
-
The patient should gently rinse his mouth with 10 ml of 5% tranexamic acid four times a day for five days
-
The operator or colleague should be accessible after hours
-
The patient should be presented with written instructions.
If a high risk procedure has to be performed such as more than three dental extractions or procedures with a high risk of bleeding, the creatinine clearance dictates when dabigatran should be stopped. The clinician overseeing patient care has a degree of discretion in applying the following recommendations. The risk of intra and post-operative bleeding is divided into two categories: high risk of bleeding/major surgery or standard risk. Although high risk surgery is not clarified, it may be taken as procedures with an increased risk of bleeding or haemorrhage (Table 2).
Once haemostasis is successfully achieved and the risk of any bleeding assessed as negligible, dabigitran can be recommenced with caution. Patients should carry a patient alert card, documenting the dose, reason for prescription of dabigatran including contact details for the prescribing physician. This is similar to the yellow anti-coagulation/INR book that most patients should carry, recording INR, but is smaller and more practical for patients to carry.
Therapeutic effect
The randomised evaluation of long term anticoagulation therapy (RE-LY)3 has demonstrated that dabigatran is generally tolerated comparibly to warfarin. The primary results indicate that dabigatran is superior in stroke prevention when directly compared with warfarin. However, dabigatran is shown to increase the annual myocardial infarction (MI) rate from 0.64% with warfarin to 0.80% with dabigatran, with a non-significant p-value. RELY provided evidence that the rate of any adverse bleeding was lower with dabigatran but did indicate that gastro-intestinal (GI) bleeds were significantly higher with dabigatran than warfarin and therefore care should be taken in at risk patients, such as those suffering from gastritis, reflux or oesophagitis.3
Overall, in comparison with warfarin, dabigatran was initially shown to decrease the overall risk of stroke and systemic emboli by approximately 35% and the risk of developing an intracranial bleed by 59%.3
Reversal
As with all anticoagulation therapy, care must be taken to ensure that unwanted haemorrhage does not occur. Should a patient present with bleeding, whether it is spontaneous or directly due to a invasive procedure, the source of the bleeding should be located and managed with local measures. Dabigitran/warfarin should be discontinued during this process until haemostasis is achieved. Coagulation tests are important to determine if dabigatran or warfarin were the cause of bleeding.
Bleeding due to warfarin can be reversed by administering factor IV or vitamin K which in turn affects coagulation factors II, VII, IX and X. It is important to understand that it can take up to 12 hours for the effects of warfarin to be reversed. In urgent cases fresh frozen plasma (FFP) or prothrombin complex concentrate (PCC) can also be used.14cstyle:>
In comparison, there is no direct reversal agent available for dabigatran. Dabigatran is excreted renally, therefore it is important that adequate diuresis is maintained. In the hypovalaemic patient this may be difficult due to inadequate renal perfusion leading to a decrease in the creatinine clearance and leading on from that the rate of excretion of dabigatran and the timely use of blood products for resuscitation is essential. The use of FFP should be considered as part of any major haemorrhage protocol. There is some experimental evidence that agents such as activated prothrombin complex concentrates, recombinant factor VIIa or concentrates of coagulation factors II, IX or X may be useful in the reversal of dabigatran. At present it is recommended that reversal agents be used at the discretion of the surgeon.14
This should not be undertaken in a dental setting and should be carefully managed by the patient's medical team. However, it is useful to understand the conversion process, if a patient presents for treatment during this period.
When converting patients from warfarin therapy to dabigatran, the warfarin is discontinued and as soon as the INR falls below two, dabigatran should be commenced as per the guidance stated above.6,7
When converting from dabigatran to warfarin, the CrCl will dictate when dabigatran should be discontinued and warfarin commenced, see table below.
As the INR can also be affected by dabigatran, the effect of warfarin on the INR will only be reflected after dabigatran has been stopped for two days.
Disadvantages
Although dabigatran has been shown to have benefits over warfarin, there are disadvantages. It is contraindicated for certain groups and conditions. It cannot be prescribed for patients under 18 years of age or patients with marked hepatic impairment whose liver enzymes are greater than twice the normal limit.
Dabigatran is also contraindicated for patients taking certain medications, such as phenytoin or carbamazepine. Care should be taken with drugs such as clopidogrel, aspirin and NSAIDS, all of which increase the risk of bleeding and patients should be made aware of the risks and the need to present to the healthcare professional should they experience any of the adverse reactions. Patients with an increased risk of spontaneous bleeding should not be prescribed dabigatran. It is also not recommended during pregnancy or breast feeding.6
Conclusion
Dabigatran is part of a new generation of anticoagulants which appear to offer significant benefits over its counterpart warfarin. It does not require routine coagulation monitoring like warfarin and with set dosing will be easier to manage for the both the clinician and patient.
However, the limitations and inability to reverse anticoagulation due to dabigatran has implications for both the patient and surgeons involved in their care. It is extremely important that clinicians are aware of the lack of a recognised reversal agent for dabigatran. The reversal agents mentioned above have not yet been proven clinically in human studies. This will have implications for treatment of patients in both primary and secondary care settings.
While dabigatran has been shown to decrease the risk of stroke in patients with AF,3 it is only suitable for certain patient groups and care is required when considering whether patients should be prescribed warfarin or dabigatran.
In conclusion, as dabigatran does not require monitoring, significant numbers of patient are likely to be managed with this type of anti-coagulant. This will impact upon dental practitioners who are likely to be faced with the prospect of treating these patients, both in the primary and secondary care setting. Understanding the drug will aid the whole dental care team and ensure that patients are safely managed.
References
NHS Choices. Atrial fibrillation. 2013. Online information available at http://www.nhs.uk/conditions/atrial-fibrillation/Pages/Introduction.aspx (accessed November 2014).
Lilly L S . Pathophysiology of heart disease: a collaborative project of medical students and faculty. 4th ed. New York: Wolters Kluwer/Lippincott Williams and Wilkins, 2007.
Ezekowitz M D . Rationale and design of RE-LY: randomised evaluation of long-term anticoagulant therapy, warfarin, compared with dabigitran. Am Heart J 2009; 157: 805–810.
Boehringer Ingelheim. Pradaxa 150mg hard capsules: section 4.1. 2011, updated 2014. Online information available at http://www.medicines.org.uk/emcmobile/medicine/24839/spc (accessed November 2014).
The Criteria Committee of the New York Heart Association. Diseases of the heart and blood vessels - nomenclature and criteria for diagnosis. 6th ed. Boston: Little Brown and Company, 1964.
Boehringer Ingelheim. Pradaxa 150mg hard capsules: section 5.2. 2011, updated 2014. Online information available at http://www.medicines.org.uk/emcmobile/medicine/24839/spc (accessed November 2014).
Boehringer Ingelheim. Pradaxa prescribing information (SPAF - UK). 2011. Online information available at http://www.boehringer-ingelheim.co.uk/content/dam/internet/opu/uk_EN/documents/prescribing%20information%20SPAF%20and%20pVTEp.pdf (accessed November 2014).
Boehringer Ingelheim. Highlights of prescribing information, section 5. 2013, revised 2014. Online information available at http://bidocs.boehringer-ingelheim.com/BIWebAccess/ViewServlet.ser?docBase=renetnt&folderPath=/Prescribing+Information/PIs/Pradaxa/Pradaxa.pdf (accessed November 2014).
Boehringer Ingelheim. Highlights of prescribing information, section 12.3. 2011. Online information available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022512s007lbl.pdf (accessed November 2014).
Boehringer Ingelheim. Pradaxa 150mg hard capsules: section 4.2. 2011, updated 2014. Online information available at http://www.medicines.org.uk/emcmobile/medicine/24839/spc (accessed November 2014).
Boehringer Ingelheim. Pradaxa 150mg hard capsules: section 4.4. 2011, updated 2014. Online information available at http://www.medicines.org.uk/emcmobile/medicine/24839/spc (accessed November 2014).
British Committee for Standards in Haematology. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. 2007. Online information available at http://www.bcshguidelines.com/documents/WarfarinandentalSurgery_bjh_264 _2007.pdf (accessed November 2014).
Heidbüchel H, Thijs V, Verhamme P, Hermans C, Peeters A, Scavée C . Practical guide dabigatran: guidance for use in particular situations. 2013. Online information available at http://www.thrombosisguidelinesgroup.be/sites/default/files/Dabigatran%20practical%20guide_Version%202%200_January%202013.pdf (accessed November 2014).
Keeling D, Baglin T, Tait C et al. Guidelines on oral anticoagulation with warfarin – fourth edition. Br J Haematol 2011; 154: 311–324.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Syyed, N., Ansell, M. & Sood, V. Dabigatran (Pradaxa®): surgeon's friend or foe?. Br Dent J 217, 623–626 (2014). https://doi.org/10.1038/sj.bdj.2014.1051
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.1051
This article is cited by
-
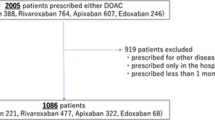
Managing direct oral anticoagulants in patients undergoing dentoalveolar surgery
British Dental Journal (2017)
-
Pharmaceuticals: Private prescription
British Dental Journal (2015)
-
Newer oral anticoagulants
British Dental Journal (2015)