Key Points
-
Tooth wear may be under-diagnosed and not care-planned for in general dental practice.
-
More recently qualified dentists were more likely to chart, risk assess and treatment plan erosive tooth wear.
-
Familiarisation with screening tools such as the Basic Erosive Wear Examination (BEWE) and up-to-date preventive advice may help dental healthcare providers risk assess and treatment plan their patients.
Abstract
Objective To assess charting, risk assessment and treatment-planning of tooth wear between recently qualified and experienced dentists in general dental practice.
Design Service evaluation.
Setting Multi-setting evaluation of three mixed NHS/Private general dental practices in North-East London.
Methods The clinical notes of new patient examinations on dentate adults presenting from the 1 October 2016 to 31 December 2016 were audited collecting data on tooth wear charting, risk assessment and treatment planning. Data were analysed using descriptives, chi square and logistic regressions in SPSS. Significance was inferred at p <0.05.
Results Foundation dentists and experienced dentists performed 85 and 200 new patient examinations, respectively, during the evaluation period. Tooth wear was charted for 48% of those attending foundation dentists and 5% of those attending experienced dentists. Diet was assessed in 50.6% of patients examined by foundation dentists and 1.0% of patients examined by experienced dentists. Foundation dentists were more likely to chart tooth wear, risk assess and preventively manage tooth wear compared to experienced dentists (p <0.001).
Conclusion This service evaluation highlights that improvements are required in recording, risk assessing and preventive treatment planning of erosive tooth wear. Experienced dentists were less likely to risk assess tooth wear and less likely to provide preventive treatment. Experienced GDPs may benefit from re-training in this area.
Similar content being viewed by others
Introduction
Tooth wear is the progressive loss of dental hard tissues through erosion, attrition and abrasion. Erosive tooth wear is defined as a chemical-mechanical process resulting in a cumulative loss of dental hard tissues.1 The aim of the term 'erosive tooth wear' is to draw attention to the fact that severe tooth wear rarely occurs without an underlying erosive element. When severe, erosive tooth wear has been associated with dentine hypersensitivity,2 pain,3 poor aesthetics3 and decreased quality of life.4 Furthermore, a pan-European study on 3,117 adults observed the UK to have the highest prevalence of erosive tooth wear across the nine European countries investigated.5 Early diagnosis, risk assessment and appropriate preventive measures may limit progression. We are aware that there is an increased risk of erosive tooth wear with increasing frequency of dietary acid intake between meals, with drinking habits such as swishing, rinsing or holding drinks in the mouth or habits by which fruit is consumed over longer time periods.6 Furthermore, a recent randomised controlled trial demonstrated that diet behaviour change was able to limit tooth wear progression over a 6-month period. [Furthermore, a recent randomised controlled trial (RCT) we carried out demonstrated that diet behaviour change was able to limit tooth wear progression over a 6-month period. (Note: the results of this RCT have been submitted for publication.)]
In addition, the relationship between palatal erosive tooth wear and gastro-oesophageal reflux involving the upper oesophageal tract is well established.7,8 The UK has a high prevalence of both gastro-oesophageal reflux disease9 and adenocarcinoma of the oesophagus10 which can correspond with reflux symptoms.11 The incidence of eating disorders is increasing in the UK12 and has also been associated with erosive tooth wear.13 Those with eating disorders tend to present with other risk factors, such as high consumption of sugar-free carbonated drinks, and dry mouth caused from xerostomic antidepressant and anxiolytic medication.13,14 Tooth wear may act as a signal diagnostic for these diseases facilitating earlier treatment and is an area where the general dental practitioner can be part of the wider health care team.
The Basic Erosive Wear Examination (BEWE) was introduced through expert consensus in 2008 as a tool to be used by GDPs to record and monitor erosive tooth wear.15 The index records the severity of tooth wear irrespective of the cause but is named BEWE to facilitate its adoption by our European colleagues. It was designed to be used in a similar manner to the Basic Periodontal Examination (BPE). The BEWE has been validated16,17 and the use of the BEWE is increasing in research and epidemiological studies. However, we have yet to collect data on whether or not general dental practitioners are using tooth wear screening tools in practice in the UK. We are also unaware how they are risk assessing patients and what preventive treatments they are providing.
The aim of this service evaluation was to assess tooth wear charting, risk assessment and preventive treatment planning in general practice on dental practitioners with different experience levels.
Methods
This was a multi-practice service evaluation, assessing erosive tooth wear risk assessment in three separate mixed NHS/private clinics in North East London. Ethical approval was obtained from the London Deanery. NHS ethical approval was confirmed as not necessary by the NHS Health Research Authority.
The clinical notes from new patient examinations on dentate adult patients with a minimum of ten teeth in each jaw, during the period 1 October 2016 to 31 December 2016 were audited by four separate dentists using an evaluation proforma. The age, gender and NHS exemption status of the patient were recorded. The total number of dentists whose notes were audited was 11 and included foundation trainees, experienced associate dentists and foundation trainers/practice owners. The year post-qualification of the examining dentist, erosive tooth wear charting, patient risk assessment and recommended treatment/monitoring period were recorded. Examining dentists were categorised as foundation dentists and those with 10+ years post qualification. Tooth wear risk assessment was categorised as recording of diet, intrinsic acid sources or parafunctional habits. Data were analysed using descriptives and chi squared tests in SPSS vers. 23 (IBM Corporation, Armonk, New York). To investigate the relationship between dentist experience and tooth wear charting and risk assessment, binary logistic regressions were performed using tooth wear charting and risk assessment as the outcome variables controlling for age, gender and exemption status of the patient. Significance was inferred at p <0.05.
Results
During the service evaluation period, 285 new patients meeting the inclusion criteria were examined. Of these, 154 were female (54%) and 131 were male (46%). The mean age of the patients was 42.7 years (SD = 17.2). There were 80 patients exempt from NHS fees and 205 NHS fee-paying patients.
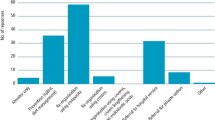
Four foundation dentists performed 85 new patient examinations and charted tooth wear on 41 of these patients (48.2%). During the same period, seven dentists with 10+ years of experience performed 200 new patient examinations and charted tooth wear on ten patients (5%). The BEWE tool was the most common screening tool and was performed on 27 patients (31.1%) by three out of the four of the foundation dentists, but by only one experienced dentist. Tooth wear risk assessment was performed on 55 patients by foundation dentists (64.7%) and 19 patients by experienced dentists (9.5%). Foundation dentists were 19 times more likely to chart tooth wear (OR 19.0, 95% CI 8.5–42.4, p <0.001) and 16 times more likely to perform a risk assessment (OR 16.0, 95% CI 8.2–30.9, p <0.001) (Fig. 1).
Intrinsic sources of acid (reflux symptoms, history of repeated vomiting or eating disorders) were rarely documented for either group. Foundation dentists assessed intrinsic sources in nine patients (10.6%) whereas only one experienced dentist had assessed intrinsic acid sources on one patient. Parafunctional habit assessment was the most common risk factor to be assessed by both foundation dentists (44 patients, 51.8%) and experienced dentists (18 patients, 9%). Diet was assessed in 43 patients (50.6%) by foundation dentists compared to two patients (1%) by experienced dentists. Foundation dentists were statistically more likely to risk assess all aspects of erosive tooth wear compared to experienced dentists (p <0.001) (Fig. 2).
Foundation dentists offered care plans targeting erosive tooth wear for 31 patients. The majority (19 patients) were care-planned for preventive treatment such as monitoring, diet advice, fluoride treatment and occlusal splints. Only two patients were treatment planned for interventive treatment such as direct or indirect restorations. In contrast, experienced dentists care planned prevention for two patients and interventive treatment for five patients. Foundation dentists were statistically significantly more likely to care plan preventive treatments than experienced dentists (p <0.001) (Fig. 3).
Discussion
A first dental examination should risk assess for all forms of oral diseases including oral cancer, caries, periodontal disease and tooth wear. Results from this service evaluation suggest that the overall level of tooth wear charting, risk assessment and preventive treatment was low for both cohorts of dentists. Diet advice and preventive advice was provided by half of the recently qualified dentists and by 1% of the experienced dentists. Although, there is a possibility that dentists were giving but not recording dietary advice, a separate medico-legal issue, it is clear that improvement is required in our service provision. Targeting common risk factors and reinforcing a healthy diet is an area where dentists have potential to impact a patient's overall health and well-being. Recommending the reduction of sugar-sweetened beverage intake, for example, juices and soft drinks, can impact tooth wear and caries in addition to systemic diseases such as diabetes and obesity.18 Similarly, certain types of gastro-oesophageal reflux and eating disorders are medical conditions associated with erosive tooth wear19 which a general dental practitioner may be able to assist with the care pathway.
These practices were chosen as they were part of the foundation training scheme within London and the service evaluation performed by four foundation trainees. This facilitated comparison of senior dentists and recently qualified dentists under the same conditions in the same practice. However, it is a relatively small group of dentists and is not representative of the dentist population. Despite this, it provides some useful comparisons between the two dentist groups. Just under half of new patients assessed by recently qualified dentists and 5% of patients assessed by experienced dentists had their tooth wear recorded during the audit period. Although it is promising to note that recently qualified dentists were more likely to perform tooth wear charting, regular screenings for patients with erosive tooth wear may assist to detect rapid progression of disease. The BEWE was the most common screening tool used in this study and has been found to be efficient and effective in a practice-based setting.17 There are free online tools and smartphone applications available to GDPs to improve erosive tooth wear charting.20 General dental practitioners are strongly encouraged to access these resources.
In a cohort of 200 patients, experienced dentists provided preventive treatments (diet advice, fluoride treatments, occlusal splints) to two patients but five patients were treatment planned for restorative treatments (direct or indirect restorations). Neglecting to provide basic preventive advice and treatment before restorative management is not consistent with modern health management principles. Other countries have identified this problem in service provision. A practice-based survey performed in Norway observed that although dentists were good at diagnosing tooth wear, their provision of preventive advice required improvement.21 Although foundation dentists were more likely to perform preventive interventions rather than restorative intervention, the overall level of preventive treatment and treatment planning for erosive tooth wear in both groups of dentists was low. There is ambiguity regarding the treatment of erosive tooth wear in practice with no universal consensus at what stage a dentist should intervene with restorative treatment.22 This is difficult to gauge and often driven by the patients concerns regarding aesthetics.23 Ideally we need evidence-based guidelines establishing optimal recall periods to monitor erosive tooth wear and when to intervene restoratively in erosive tooth wear progression. Until these guidelines are established, recording tooth wear and monitoring wear while providing preventive advice are the best tools available to the general dental practitioner to inform treatment decisions.
This study is limited in that only three practices were assessed in a single borough in London and is not representative. Similar service evaluations across the UK in rural and urban populations are needed to generalise these findings to all general dental practitioners. It does give an indication that the level of erosive tooth wear monitoring and treatment planning is low. It is promising to note that tooth wear monitoring is being incorporated into routine examinations by a greater number of younger dentists.
Conclusion
This service evaluation demonstrates improvement is required in recording, risk assessing and treatment planning erosive tooth wear. Experienced dentists were less likely to risk assess tooth wear and more likely to provide restorative treatment rather than preventive treatment. Experienced general dental practitioners may benefit from re-training in this area.
References
Carvalho T S, Colon P, Ganss C et al. Consensus report of the European Federation of Conservative Dentistry: erosive tooth wear—diagnosis and management. Clin Oral Investig 2015; 19: 1557–1561. 10.1007/s007840151511–17.
West N X, Sanz M, Lussi A, Bartlett D W, Bouchard P, Bourgeois D . Prevalence of dentine hypersensitivity and study of associated factors: A European population-based cross-sectional study. J Dent 2013; 41: 841–851. 10.1016/j.jdent.2013.07.017.
Al-Omiri M K, Lamey P J, Clifford T . Impact of tooth wear on daily living. Int J Prosthodont 2006; 19: 601–605.
Li M H M, Bernabé E . Tooth wear and quality of life among adults in the United Kingdom. J Dent 2016; 55: 48–53. 10.1016/j.jdent.2016.09.013.
Bartlett D W, Lussi A, West N X, Bouchard P, Sanz M, Bourgeois D . Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013; 41: 1007–1013. 10.1016/j.jdent.2013.08.018.
O'Toole S, Bernabé E, Moazzez R, Bartlett D . Timing of dietary acid intake and erosive tooth wear: A case-control study. J Dent 2017; 56: 96–104. 10.1016/j.jdent.2016.11.005.
Moazzez R, Anggiansah A, Bartlett D W . The association of acidic reflux above the upper oesophageal sphincter with palatal tooth wear. Caries Res 2005; 39: 475–478. 10.1159/000: 088, 182.
Bartlett D W, Evans D, Anggiansah A, Smith B G . A study of the association between gastro-oesophageal reflux and palatal dental erosion. Br Dent J 1996; 181: 125–131.
El-Serag H B, Sweet S, Winchester C C, Dent J . Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014; 63: 871–880. 10.1136/gutjnl-2012-304269.
Edgren G, Adami H O, Weiderpass E, Nyrén O . A global assessment of the oesophageal adenocarcinoma epidemic. Gut 2013; 62: 1406–1414. 10.1136/gutjnl-2012-302412.
Lagergren J, Bergstromeinhold R, Lingren A, Nyren O . Symptomatic gastoroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med 1999; 340: 825–831. 10.1056/NEJM199903183401101.
Micali N, Hagberg K W, Petersen I, Treasure J L . The incidence of eating disorders in the UK in 2000-2009: findings from the General Practice Research Database. BMJ Open 2013; 3: 1–8. 10.1136/bmjopen-2013-002646.
Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson N W . A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med 2015; 77: 83–92. 10.1097/PSY.0000000:000000135.
Kisely S, Sawyer E, Siskind D, Lalloo R . The oral health of people with anxiety and depressive disorders – a systematic review and meta-analysis. J Affect Disord 2016; 200: 119–132. 10.1016/j.jad.2016.04.040.
Bartlett D W, Ganss C, Lussi A . Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig 2008; 12: S65–68. 10.1007/s007840070181–5.
Olley R C, Wilson R, Bartlett D W, Moazzez R . Validation of the basic erosive wear examination. Caries Res 2014; 48: 51–56. 10.1159/000351872.
Dixon B, Sharif M O, Ahmed F, Smith A B, Seymour D, Brunton P A . Evaluation of the basic erosive wear examination (BEWE) for use in general dental practice. Br Dent J 2012; 213: E4. 10.1038/sj.bdj.2012.670.
Basu S, McKee M, Galea G, Stuckler D . Relationship of soft drink consumption to global overweight, obesity, and diabetes: A cross-national analysis of 75 countries. Am J Public Health 2013; 103: 2071–2077. 10.2105/AJPH.2012.300974.
Moazzez R, Bartlett D . Intrinsic causes of dental erosion. In Lussi A, Ganss C (eds). Erosive tooth wear – From diagnosis to therapy. 2nd ed. Basel: Karger; 2014: 180–196.
GSK. BEWE Examination Tool. Available online at https://www.gsk-dentalprofessionals.co.uk/resources/pronamel-bewe-examination-tool/ (accessed February 2018).
Mulic A, Vidnes-Kopperud S, Skaare A B, Tveit A B, Young A . Opinions on dental erosive lesions, knowledge of diagnosis, and treatment strategies among Norwegian dentists: a questionnaire survey. Int J Dent 2012; 716396. 10.1155/2012/716396.
Bartlett D . A personal perspective and update on erosive tooth wear – 10 years on: Part 2 – Restorative management. Br Dent J 2016; 221: 167–171. 10.1038/sj.bdj.2016.555.
Ahmed K E, Murray C A, Whitters C J . A prospective survey of secondary care tooth wear referrals: demographics, reasons for concern and referral outcomes. Br Dent J 2014; 216: E9. 10.1038/sj.bdj.2014.179.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O'Toole, S., Khan, M., Patel, A. et al. Tooth wear risk assessment and care-planning in general dental practice. Br Dent J 224, 358–362 (2018). https://doi.org/10.1038/sj.bdj.2018.171
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.171
This article is cited by
-
The opinions of GDPs on the challenges of managing tooth wear in primary dental care
British Dental Journal (2023)
-
Clinical factors to consider in definitive treatment planning for patients with tooth wear
British Dental Journal (2023)
-
Validation of an erosive tooth wear risk factors questionnaire for adolescents
Clinical Oral Investigations (2022)
-
A study to investigate habits with tooth wear assessments among UK and non-UK dental practitioners
British Dental Journal (2020)
-
Campaign launched to drive routine screening for erosive tooth wear
BDJ Team (2019)