Key Points
-
Summarises the Royal College of Surgeons' (England) guidelines on the management of TMD in primary care.
-
Provides a brief overview of presentation of TMD, history and diagnosis of TMD and principles of management.
-
Guides the reader towards resources contained in the full guideline that will be of help to healthcare practitioners and patients.
Abstract
This paper briefly summarises the key points from the Royal College of Surgeons' (England) Faculty of Dental Surgery Clinical Standards Committee's guidance on the management of temporomandibular disorders in primary care. The full guidelines developed by the faculty in conjunction with the UK Specialist Interest Group in Orofacial Pain and Temporomandibular Disorders (USOT) are available at: http://www.rcseng.ac.uk/fds/publications-clinical-guidelines/clinical_guidelines.
Similar content being viewed by others
Background
The Royal College of Surgeons of England, Faculty of Dental Surgery (FDSRCS (Eng)) develops and maintains a wide range of clinical guidelines to support the highest standards of clinical practice and patient care. This is achieved by working in conjunction with other stakeholders, such as the Department of Health, NICE and other professional bodies.
The guidelines are the responsibility of the clinical standards committee of the FDSRCS (Eng) and are either the work of the committee itself or the endorsement of work by other bodies such as specialist societies.
Temporomandibular disorders (TMD) can present understandable difficulties to the primary care practitioner and some specialist practitioners.1,2,3 It was against this background that the UK specialist interest group in orofacial pain and temporomandibular disorders (USOT) was established with the aim of 'establishing and promoting good practice in diagnosis and management of chronic orofacial pain and TMD' and encouraging cross-specialty management of TMD and chronic orofacial pain.
In conjunction with the FDCRCS (Eng) Clinical Standards Committee, USOT has produced guidance on the management of TMD in primary care in order to give helpful and evidence-based guidance to primary care practitioners.4
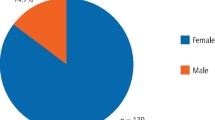
TMD are musculoskeletal disorders and represent the most common cause of chronic pain in the orofacial region. TMD have been known by a plethora of other terms including: myofascial pain dysfunction syndrome, TMJ and TMJD. TMD is now more commonly understood as a collective term, which describes a group of disorders comprising of myogenous and or arthrogenous conditions. TMD reaches a peak incidence in the second and third decades of life, predominantly affecting females.5
History, examination and diagnosis
As with any presenting condition, a full history and examination should be undertaken to enable the formulation of a provisional diagnosis.
The history should examine the symptoms, their character and natural history, and any co-morbidities, predisposing, precipitating, and perpetuating factors.4 Due to the multifactorial biopsychosocial (biological, psychological and sociological) nature of TMD, some form of psychosocial assessment is necessary.
Careful extra- and intra-oral examination of the head and neck structures will help exclude dental pathology as a source of symptoms, while also identifying any other abnormalities or worrisome and red flag findings.4
The signs and symptoms of TMD commonly include:
-
Pain in and around the TMJs and muscles of mastication
-
Muscle and joint tenderness on palpation
-
Joint sounds (clicking and crepitus)
-
Limitation and incoordination of mandibular movement
-
Headaches
-
Otalgia.
One of the more common physical diagnoses of TMD affecting the muscles of mastication is myogenous pain, with or without limitation of opening. The TMJs are also affected by clicking (disc displacement with reduction) and less so by (closed) locking (disc displacement without reduction with limited opening) and dislocation. In addition, the TMJs can be affected by pain and because it is difficult to distinguish the cause of the pain (for example, synovitis, capsulitis, retro-discitis) it is labelled 'arthralgia'. However, if there is pain and crepitus from the joint, indicating articular degeneration, it is diagnosed osteoarthritis.
Dentists should also remember that for some TMD patients their symptoms are part of a systemic condition, for example rheumatoid arthritis, and management of any TMD-like symptoms should be conducted in partnership with the physicians managing their overall condition.
There are a number of recognised diagnostic systems for TMD, but those that operationalise the history and examination provide the most help, for example the clinical examination protocol (CEP-TMD).6 There are also a number of useful sources of information freely available on the web4 containing diagnostic proformas and video demonstrations that practitioners may find useful.
Management for TMD
Reversible and non-invasive therapy should always be the initial management for TMD7 and it's goals should be to:
-
Encourage self-management of the condition through education
-
Reduce the (impact of) pain associated with the condition
-
Decrease functional limitation caused by the condition
-
Reduce exacerbations and educate individuals in how to manage any exacerbation of the condition.
Most of this type of therapy is achievable within primary care either by the dentist alone, or in conjunction with the general medical practitioner or a specialist team. It is important that a management plan is constructed for each case, and this may involve a range of approaches determined by both the symptoms, and the patient's response to the reversible interventions applied, which include:
-
Self-management with an explanation of the diagnosis and its benign, largely non-progressive, nature
-
Physical therapies
-
Pharmacotherapy
-
Occlusal splint therapy
-
Psychological interventions.
It is important to ensure that the patient understands that without full engagement in self-management there will be no foundation for the restoration of control over the signs and symptoms of TMD. Patients need to understand the fluctuating nature of TMD and that with education they can self-manage these exacerbations using very simple techniques.
When introduced early, reversible, non-invasive therapy has been shown to have between a 68–95% success rate across the subtypes of TMD8,9,10,11,12,13,14 and failure of reversible, non-invasive therapy is not an indication to progress to irreversible treatment or more advanced pharmacotherapy.4 A key component of reversible, non-invasive therapy is implementing a review of the patient to identify if management is progressing as would be expected.
Outcome assessment
Given the biopsychosocial nature of TMD, and dependent on the nature and origin (myogenous or arthrogenous), there are a number of areas that can valuably be assessed at repeated follow-ups: objective clinical measurements (for example, jaw opening measurements), simple pain scales and multidimensional patient reported outcome measures (PROMs) are currently under development.
At present, in everyday clinical practice, the best summation of the overall therapeutic goal for TMD is to educate the patient about the condition, and equip them so they feel able to self-manage the condition and its occasionally fluctuant nature. Clinicians should, therefore, carefully discuss with patients their perceived ability in self-managing the condition throughout the time they are undergoing management. This is in itself an important outcome measure.
Conclusion
USOT hope that the guidelines provide support and guidance for primary care practitioners, enabling them to feel comfortable identifying red flags, and diagnosing and performing initial reversible non-invasive therapy for TMD. Provision of a diagnosis for TMD and reassurance over its benign nature and largely self-limiting course is an absolute necessity before starting simple reversible, non-invasive therapies. This first line management is likely to be effective in the vast majority of simple cases.
References
Aggarwal V R, Joughin A, Zakrzewska J, Appelbe P, Tickle M . Dentist's preferences for diagnosis, management and referral of chronic oro-facial pain: results from a national survey. Health Educ J 2012; 71: 662–669.
Aggarwal V R, Joughin A, Zakrzewska J M, Crawford F J, Tickle M . Dentists' and specialists' knowledge of chronic orofacial pain: results from a continuing professional development survey. Prim Dent Care 2011; 18: 41–44.
Durham J, Exley C, Wassell R, Steele J G . 'Management is a black art'professional ideologies with respect to temporomandibular disorders. Br Dent J 2007; 202: E29.
Royal College of Surgeons. Temporomandibular disorders (TMDs): an update and management guide for primary care from the UK Specialist Interest Group in Orofacial Pain and TMDs (USOT). 2013. Online information available at http://www.rcseng.ac.uk/fds/publications-clinical-guidelines/clinical_guidelines (accessed March 2015).
Maixner W, Diatchenko L, Dubner R et al. Orofacial pain prospective evaluation and risk assessment study - the OPPERA study. J Pain 2011; 12 (Suppl 11): T4–11.e2.
Hasanain F, Durham J, Moufti A, Steen I N, Wassell R W . Adapting the diagnostic definitions of the RDC/TMD to routine clinical practice: a feasibility study. J Dent 2009; 37: 955–962.
Greene C S . Managing the care of patients with temporomandibular disorders: a new guideline for care. J Am Dent Assoc 2010; 141: 1086–1088.
Sato S, Kawamura H, Nagasaka H, Motegi K . The natural course of anterior disc displacement without reduction in the temporomandibular joint: follow-up at 6, 12, and 18 months. J Oral Maxillofac Surg 1997; 55: 234–238.
Randolph C S, Greene C S, Moretti R, Forbes D, Perry H T . Conservative management of temporomandibular disorders: a posttreatment comparison between patients from a university clinic and from private practice. Am J Orthod Dentofacial Orthop 1990; 98: 77–82.
Magnusson T, Carlsson G E . A two and a half year follow-up of changes in headache and mandibular dysfunction after stomatognathic treatment. J Prosthet Dent 1983; 49: 398–402.
Greene C S, Laskin D M . Long-term evaluation of treatment for myofascial pain-dysfunction syndrome: a comparative analysis. J Am Dent Assoc 1983; 107: 235–238.
Nel H . Myofascial pain-dysfunction syndrome. J Prosthet Dent 1978; 40: 438–441.
Carraro J J, Caffesse R G . Effect of occlusal splints on TMJ symptomatology. J Prosthet Dent 1978; 40: 563–566.
Greene C S, Laskin D M . Long-term evaluation of conservative treatment for myofascial pain-dysfunction syndrome. J Am Dent Assoc 1974; 89: 1365–1368.
Acknowledgements
USOT who authored the full guidelines consists of: J.Durham, VR Aggarwal, SJ Davies, SD Harrison, RG Jagger, R Leeson, R Lloyd, T Thayer, H Underhill, RW Wassell, J M Zakrzewska, A Begley, AR Loescher, E Murphy, R McMillan, T Renton
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Durham, J. Summary of Royal College of Surgeons' (England) clinical guidelines on management of temporomandibular disorders in primary care. Br Dent J 218, 355–356 (2015). https://doi.org/10.1038/sj.bdj.2015.194
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.194
This article is cited by
-
Patients’ experiences of temporomandibular disorders and related treatment
BMC Oral Health (2023)