Key Points
-
Suggests that simple, low cost studies, whilst not perhaps providing definitive answers, can provide useful information for commissioners.
-
Reports that public health dental preventive interventions are associated with improved population oral health.
Abstract
Introduction An evaluation was undertaken to measure the dental health of five cohorts of 5-year-old children living in Halton and St Helens, each cohort having had a different length of time they were exposed to a population dental prevention programme before their fifth birthday.
Method The dental health of each of five consecutive cohorts of 5-year-old children was measured epidemiologically using standardised methods.
Results The mean level of active decay (dt) in the cohort that had the greatest exposure to the preventive intervention (cohort 5, 2011/12) was 0.83, whereas the mean level of active decay in the cohort with no exposure to the preventive programme (cohort 1, 2007/8) was 1.07. This represents a reduction of 22% in the mean level of active decay in 5-year-olds. There was also a 5.9% absolute increase in the number of 5-year-old children free from decay experience between cohorts 5 and 1. Children living in Halton and St Helens with postcodes in the more socially deprived index of multiple deprivation (IMD) tertiles gained the most from the programme. Comparing cohort 5 and cohort 1, the increase in the proportion of children free from decay was greatest in IMD tertiles 1 and 2 and least in IMD tertile 3 (least socially disadvantaged).
Conclusion Following a four-year population dental preventive programme the dental health of 5-year-old children living in Halton and St Helens has improved and dental health inequalities have reduced. As there was no control group, the effects seen are associative and cannot be assumed to be causative.
Similar content being viewed by others
Introduction
Historically, child dental health in Halton and St Helens has been poor. In 2007, the average Halton and St Helens 5-year-old had in excess of 1.43 decayed, missing or filled teeth (dmft).1 By contrast, nationally, the average 5-year-old had 29% less decay experience with a dmft of 1.1.
Large numbers of children in Halton and St Helens go to an NHS dentist. Indeed, over 70% of local under-18-year-olds attend their dentist on a regular basis.2 Additionally, Halton and St Helens PCT has supported a primary school based milk fluoridation programme for 19 years. Despite this, childhood decay rates in Halton and St Helens have over time remained stubbornly resistant to change. In an attempt to address this problem, the PCT, in spring 2008, embarked on a four-year, two pronged population-based dental prevention programme. It was agreed that:
-
All children attending their dentist would be offered fluoride varnish three times per year
-
All 34,000 children aged 3-11 years living within the boundary of the PCT would be sent through the post, twice yearly, a toothbrush and a tube of fluoride toothpaste (1,450 ppm).
The basis of the former intervention was the BASCD/DH document Delivering better oral health: an evidence based toolkit for prevention.3 The PCT's view was that because of the generally poor levels of child dental health locally, three fluoride varnish applications per year was an appropriate regime for all children to be offered. This programme was rolled out in July 2008. Two applications of fluoride varnish were included as part of the regular six-monthly dental assessments for children. Dentists were given one additional UDA for the third annual fluoride varnish application. Data from the Dental Services Division of the Business Services Authority in July 2012 indicated that the number of claims including fluoride varnish was four times higher among dentists in Halton and St Helens than in the country as a whole.4
The basis of the toothpaste distribution programme is an acceptance that fluoride toothpaste is an evidence-based preventive vehicle.5 Data from the toothpaste manufacturers suggest that toothpaste volume sales in the northwest of England are less than the national average and by regularly delivering a toothpaste/toothbrush package to all 34,000 children aged 3-11 years living within the boundary of the PCT, it was hoped that the toothpaste would be used and that receipt of this preventive package would prompt continued fluoride toothpaste usage within the family. The first toothpaste distribution date was January 2009, with subsequent distributions taking place every six months from that date. The most recent distribution took place in September 2012.
Method
The impact of this population approach to dental prevention was measured epidemiologically. Starting in 2007/8, the dental health of 5-year-olds in Halton and St Helens was measured using standard BASCD6 protocols with trained and calibrated dental epidemiologists. Subsequently, a further four annual local epidemiological surveys of the dental health of 5-year-olds living in Halton and St Helens were undertaken using the same BASCD survey criteria. For each sample survey, all 5-year-old children were invited to participate. Positive consent was used for all of the surveys.
The first cohort of 5-year-olds (2007/8), had never been exposed to the PCT's preventive programme when its dental health was measured. The second cohort (2008/9) had received limited exposure to the programme by the time the baseline data were collected (approximately 0-12 months). The third cohort (2009/10) had been exposed to the preventive programme for between 12-24 months. The fourth cohort (2010/11) had been exposed to the preventive programme for 24-36 months. For cohort 5 (2011/12), the children had been exposed to the preventive programme for 36-48 months before they participated in the evaluation.
Post code data were collected for the place of residence of each child that was eligible to participate in the evaluation in order to identify the social profile of each cohort using the index of multiple deprivation (IMD).7
This paper reports the dental health of five successive 5-year-old population cohorts in Halton and St Helens, each cohort having had a greater exposure time to the preventive programme than the previous one. The paper also reports the impact of the programme on the dental health of children from different social backgrounds.
Results
Table 1 sets out the percentage of the eligible 5-year-old population that participated in each epidemiological survey and the mean IMD score of each participating cohort. The data show that for each annual survey, a similar proportion of the 5-year-old child population participated and the mean IMD scores of the five cohorts were similar. This latter observation is important as it suggests that all the 5-year-old cohorts in the study were socially similar. Table 2 sets out the dental health of the five 5-year-old cohorts.
The data show that the cohort with the greatest life exposure to the dental preventive programme (cohort 5) has better dental health than the cohorts with less life exposure to prevention. The mean number of teeth with active decay in cohort 5 (0.83) is 22% lower than that found in cohort 1 (1.07). The proportion of 5-year-old children free from decay experience in cohort 5 (67.5%) is 5.9% higher than in cohort 1 (61.6%).
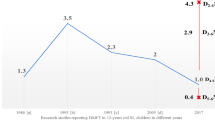
Table 3 sets out the percentage of children free from active decay in each cohort by tertile of IMD. The data show that a social gradient effect is present in each cohort, with, as would be expected, a greater proportion of children whose postcodes are classified in IMD tertile 1 (most socially disadvantaged) being the least likely to be free from active decay. However, the data also show that the greatest improvements in dental health, in absolute terms between cohorts 1 and 5 are to be found in those children whose postcodes are categorised as falling within IMD tertiles 1 and 2. Within these tertiles, the difference in the proportion of children free from decay between cohorts one and five was 4.3% (tertile 1) and 7.4% (tertile 2). For those children in IMD tertile 3 (the most affluent), the difference was 3.6%.
Discussion
This evaluation examines the dental health of five 5-year-old cohorts in Halton and St Helens, the children in each cohort having been exposed to a community dental preventive programme for a different length of time before their fifth birthday. After four years the programme was associated with a 22% reduction in the mean level of active decay in the primary dentition of 5-year-olds. Further, over the period of the evaluation, the percentage of 5-year-olds free from decay experience has increased by almost 6%.
In each year cohort approximately half of the eligible 5-year-population positively consented to participate in the evaluation (Table 1) and year on year, the social profile of children that participated in the dental epidemiological surveys remained relatively stable. Given that population child oral health is closely related to levels of social deprivation,8 the observed changes in dental health between cohorts 1 and 5 cannot be explained by variation in levels of social deprivation within the cohorts.
The data show that there is a trend of improving oral health associated with the length of time the children had been exposed to the preventive programme before their fifth birthday (Table 2). Cohort 5, having had the greatest exposure to the programme (36-48 months) had the best dental health, while cohort 1, with no exposure had the worst. The evaluation also identifies that the programme had a greater impact on children from the more deprived sections of the community (Table 3). In IMD tertiles 1 and 2, the most socially deprived tertiles, there was an increase of 4.3% and 7.4% in the percentage of children free from active decay between cohorts 1 and 5. The equivalent change among children from IMD tertile 3 was 3.6%.
It is important that preventive programmes not only reduce population levels of disease, but also reduce dental health inequalities. The dental profession has struggled to provide the most vulnerable children in society with effective prevention9 and programmes that effectively address this problem need to be developed.
This evaluation only included dental data on children consenting to the study, yet the toothpaste distribution programme was directed at all 3-11 year-olds living in the community and all children attending their dentist were expected to be offered fluoride varnish. In each year of recruitment to the evaluation study there were considerable numbers of children whose parents failed to respond to a request to participate in the study. For each of the five cohorts the mean IMD score of those children whose parents failed to respond was found to be greater than the IMD scores for those that agreed or refused to take part (unpublished data). It is possible, therefore, that this paper under reports the true population benefit of this preventive programme because significant numbers of relatively disadvantaged children, likely to have had high levels of dental decay, were not included in the evaluation, yet may well have benefited from the programme.
This study has significant limitations. No controlled population was observed and the possibility therefore exists that the improvements noted in Halton and St Helens may well have occurred independently of the preventive programme, although it should also be noted that in the last 40 years, since data on the dental health of children has been systematically collected, no similar dental health improvement has been recorded locally.
In 2012, the nationally delivered NHS child dental epidemiological survey, conducted to BASCD standards,1 confirmed statistically significant reductions in mean active decay levels among 5-year-olds in both Halton and St Helens local authority areas, when compared with 2007. In neighbouring Knowsley, a socially similar local authority area, while a reduction in mean active decay level was noted among 5-year-olds between 2007 and 2012, the difference did not reach statistical significance (Table 4).
The costs of the programme were modest. Material costs (toothpaste, toothbrushes and postage) were £259,760 in 2012 or £7.64 per child per year. The cost of this programme represents 1.6% of the annual NHS primary dental care spend in Halton and St Helens PCT. While dentists were given an additional UDA for applying fluoride varnish for a third time in each year, the overall PCT UDA account was not increased.
What this evaluation cannot tell us is the relative impact that the two elements of the preventive programme have on population child dental health. Should the preventive focus be mainly based on the use of fluoride varnish in dental practice or does greater benefit come from delivering prevention across the whole population via the distribution of fluoride toothpaste? Are the two interventions complementary?
Only the 'gold standard' approach of subjecting Halton and St Helens' preventive programme to a well-designed randomised controlled trial will provide the definitive scientific answers to the questions above, but randomised controlled trials are time consuming and expensive to deliver. In this case, such an approach may be an unnecessary research 'luxury' because small scale, pragmatic, low cost local public health evaluation studies, of the type reported here, can provide sufficient information for commissioners to make important practical decisions about the best way to deliver effective dental prevention in specific settings. The lack of scientific rigour associated with this evaluation may limit the usefulness of the findings outside Halton and St Helens, but this particular evaluation study was simple and inexpensive to undertake and readily replicated in other communities. If other localities are able to demonstrate improvements in child dental health following the introduction of programmes similar to that delivered in Halton and St Helens, how much does it matter to NHS dental commissioners if theoretical scientific questions remain? The key points are that child dental health improvement has been achieved and the dental inequalities agenda has been addressed – both important political imperatives.10
In the absence of high quality research data, dental commissioners in areas of the country with stubbornly high levels of childhood decay have to make value judgements about how best to use limited resources dedicated to dental prevention. For some communities wishing to improve levels of oral health, water fluoridation may be the long term goal, but until such schemes are able to proceed a credible dental prevention 'plan B' is required. Identifying the optimal 'plan B' presents difficulties. Should we move away from the population approach and instead target those children who are perceived to be at 'increased risk' of decay, offering this selected group additional support.11 Unfortunately, current dental practice-based risk assessment models have their shortcomings and when implemented in practice can lead to substantial numbers of children deemed to be at low risk of decay actually going on to develop the disease.12 Perhaps the optimal approach to dental prevention is to be found in the Department of Health's guidance document Delivering better oral health: an evidence based toolkit for prevention3 which advocates the adoption of both the population and risk assessment models when planning the clinical dental care of children. This guidance recommends that the parents of all children attending the dentist should be advised to use fluoride toothpaste when cleaning their children's teeth. Clearly there has to be merit in offering all children, including those who do not attend a dentist, a similar degree of cost effective, evidence-based prevention and if this means distributing fluoride toothpaste to families in areas of the country where toothpaste purchasing levels can be shown to be suboptimal, then this should be considered by dental commissioners. Once this 'safety net' level of prevention is in place for all, it is then wholly appropriate to explore targeted techniques in primary care which focus on those children who are felt to be at greater risk of developing decay.
Dentists in Halton and St Helens have for years been doing their best to prevent dental decay in the local child population and their efforts have been underpinned by the implementation of risk assessment models, supported by a school-based milk fluoridation programme. Despite their best efforts, levels of childhood decay have remained largely unaltered for over 30 years. Within four years of the introduction of an evidence-based population prevention programme, levels of decay in the local child population have fallen substantially and child dental health inequalities are reducing. This improved level of child dental health has been achieved at limited cost and the programme is sustainable. By offering communities an effective population-based dental prevention programme, child oral health can be expected to improve and the stage is then set for primary care to address the needs of that diminishing number of children who remain at substantial risk of decay, and who are likely to benefit from further, individually tailored clinical dental preventive support.
References
British Association for the Study of Community Dentistry. Oral Health Surveys. Online information available at: http://www.bascd.org/oral-health-surveys (accessed February 2014).
NHS Information Centre for Health and Social Care. NHS Dental Statistics for England, Quarter 3, 31 December 2009. Online information available at: www.ic.nhs.uk/pubs/dentalstats0910q3 (accessed February 2014).
Department of Health/ British Association for the Study of Community Dentistry. Delivering better oral health: an evidence based toolkit for prevention. 2nd ed. London: Department of Health, 2009.
NHS Business Services Authority – NHS Dental Service. Halton and St Helens PCT, General Clinical Data Set for Quarter end March 2010. http://www.nhsbsa.nhs.uk
Marinho V C, Higgins J P, Sheiham A, Logan S . Fluoride toothpastes for preventing dental caries in children and adolescents 2003. Cochrane Database Syst Rev 2003; CD002278.
Mitropoulos C M, Pitts N B, Deery C . British Association for the Study of Community Dentistry criteria for the standardised clinical assessment of dental health (1992/3). In BASCD Trainer's Pack for caries Prevalence Studies 1992/3. Dundee: University of Dundee, 1992.
Office of the Deputy Prime Minister. The English indices of deprivation 2004: summary (revised). 2004. Online report available at http://webarchive.nationalarchives.gov.uk/20120919132719/http://www. communities.gov.uk/documents/communities/pdf/131206 (accessed February 2014).
Riley J C, Lennon M A, Ellwood R P . The effect of water fluoridation and social inequalities on dental caries in 5-year-old children. Int J Epidemiol 1999; 28: 300–305.
Davies G M, Worthington H V, Ellwood R P et al. An assessment of the cost effectiveness of a postal toothpaste programme to prevent caries amongst 5-year-olds in the North West of England. Community Dent Health 2003; 20: 207–210.
Department of Health. The Operating Framework for the NHS in England 2011/12. Online information available at: www.dh.gov.uk (accessed February 2014).
Page J, Weld J A, Kidd E A M . Caries control in health service practice. Br Dent J 2010; 208: 449–450.
Milsom K M, Blinkhorn A S, Tickle M . The incidence of dental caries in the primary molar teeth of young children receiving National Health Service funded dental care in practices in the North West of England. Br Dent J 2008; 205: E14; discussion 384–385.
Acknowledgements
Janet Neville, Dental Project Manager, The Dental Observatory, Jubilee House, Lancashire Business Park, Centurion Way, Leyland, PR26 6TR
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milsom, K., Rice, A., Kearney-Mitchell, P. et al. A review of a child population dental preventive programme in Halton and St Helens. Br Dent J 216, E18 (2014). https://doi.org/10.1038/sj.bdj.2014.334
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.334
This article is cited by
-
Summary of: A review of a child population dental preventive programme in Halton and St Helens
British Dental Journal (2014)