Key Points
-
In a digital, paperless era, clinicians need to decide whether and how to store old radiographs.
-
Film radiographs can be digitised simply by using a digital camera.
-
Storing existing radiographs in a digital medium does not cause loss of critical information or alter treatment decisions.
Abstract
Aim To investigate whether digital images obtained by a digital camera are deficient compared to the original radiographs.
Materials and methods Twenty pairs of bitewing radiographs of children and 40 anterior periapical radiographs were photographed using a digital camera. Images were saved as JPEG files and loaded onto a laptop. Film radiographs and digital images as scanned and after adjustments were evaluated for proximal caries and for periapical pathologies.
Results A not statistically significant higher number of proximal lesions were observed on plain-film and enhanced digital images than on unenhanced images. Enhanced digital images resulted in significantly more diagnoses of external root resorption compared with conventional radiographs. Pulp canals appeared significantly more abnormal (obliterated or enlarged) in digital images compared with film radiographs.
Conclusions Storing existing radiographs in a digital medium for space saving purposes using a digital camera does not loose critical information.
Clinical implication Clinicians can use digital cameras to digitise and store radiographic images without losing important diagnostic information.
Similar content being viewed by others
Introduction
Since its introduction in the early 1980s, digital radiography has drawn considerable interest in the clinical and the research fields. Its main advantages over conventional film radiographs are speed, convenience, no darkroom procedures, image improvement tools, and in some cases reduced radiation exposure. Although the implementation of digital radiography in a dental practice provides a solution for future imaging requirements, the transfer of existing records (conventional radiographs) to a digital form needs to be addressed for reasons of uniformity and space saving. There is a need to store radiographs in patient charts and archives in a space saving manner.
Several researchers have claimed that density and contrast values of digitised radiographs would not be the same as those of conventional film,1,2 although they can be modified with image processing tools.3,4,5 In one study that compared four different film scanners and addressed the possible loss of information during scanning, the authors concluded that the scanners could not produce a reliable digital conversion of plain film because of their density range limitation.6 These findings agree with another study that indicated a significant loss of information in scanned radiographs, particularly in the dark zones.7
However, others have found no differences in resolution between digitised images and the film-based radiographs,8 although the digitised radiographs demonstrated higher density. While scanned digitisation of conventional radiographs and their comparison with conventional images has been reported, studies using digital cameras as the means of digitisation are very rare.9,10
There are several advantages of digital camera technology producing images of diagnostic quality. Digital cameras are increasingly in use around the world; the photographs are suited for immediate data transmission, eg via email to a specialist, colleague, or dental laboratory, and instant integration into dental practice software for storage; images can be diagnostically enhanced in a similar fashion to digital radiographs, using existing camera software; in a dental practice, it is a means of transferring patient records (conventional radiographs) onto the practice database; and digital photographs facilitate patient education and acceptance of treatment.
A study to determine the proper scanning resolution when using a flatbed scanner for bitewing radiographs in the diagnosis of the presence and depth of approximal caries found that 300 dpi provided the best results for caries detection at almost all lesion depths.11
It has been claimed that the reason digitising conventional radiographs using current high-grade digital cameras or scanners does not produce images of diagnostic quality is the need for improved resolution of viewing monitors.12 Another study found that pulp areas within the crown molar were larger than indicated by radiographs, and there may be a greater risk of mechanical pulp exposure than revealed by the radiographs.13 Therefore the need for accuracy in diagnosis is emphasised.
The purpose of the present study was to compare the diagnostic performance of plain-film intraoral radiographs with digital images of these radiographs obtained with a high-end digital camera for caries and periapical pathologies.
Materials and methods
The study examined retrospectively 20 pairs of bitewing radiographs (total of 272 surfaces), and 40 anterior periapical radiographs of children (mean age of 6.7 years, SD 1.8 years) taken from a collection of a private practice, used in student teaching exercises in paediatric dentistry. There were 101 mesial surfaces and 101 distal surfaces of first and second primary molars and first permanent molars (total of 202 surfaces), and 34 mesial and 36 distal surfaces of primary canines (total of 70 surfaces). The identity of the patients was blinded to the investigators. The study was approved by the Helsinki committee of Tel Aviv University.
Radiographs were taken using a Gendex Medical System X-ray machine (Oralix 65S, Italy) operating at 10 mA and 65 kVp. These showed carious lesions and were standardised by using a Kwik-Bite film holder (Hawe Neos Dental, Bioggio, Switzerland). Radiographs were developed using a manual developing box containing conventional developer and fixer.
All radiographs were placed in slide holders on a light viewing box (Magni Viewer III, Proyrex, Tokyo, Japan) and photographed using a Nikon D70S digital camera (Nikon Corporation, Tokyo, Japan) with an AF Micro-Nikkor 60 mm f/2.8D lens (ISO 200, F = 8, shutter speed = 1/125). The Nikon camera features a charge coupled device (CCD) of 5.47 million pixels with a recording image of 3,008 × 2,000 pixels.
The Nikon camera images were taken at the same camera-radiograph distance with a camera-holder jig. Identical illumination was used throughout with the radiographs placed at the same location on the light box. Digital camera images were saved as Joint Photographic Experts Group (JPEG) files.
Digital images were loaded directly onto an IBM T43 ThinkPad laptop with a 14 inch screen. Images were opened using ACDSee software (Version 8, ACD Systems, Victoria, BC, Canada). The full screen was used with a black background for each image. The following parameters were evaluated for bitewing radiographs: presence of proximal caries (yes/no); depth of lesion (≤half of the enamel width / >half of the enamel width); and treatment decision (restoration/follow-up). The latter was included because it was agreed that a lesion of less than one-half the enamel width would generally not be restored but treated with fluoride and followed-up, where the lesion was adjacent to a sound proximal tooth structure. When lesions less than one-half the enamel width were adjacent to a lesion of more than one-half the enamel width, the smaller lesion was also restored.
For the periapical radiographs, the following parameters were evaluated: periapical pathology (yes/no); periodontal ligament (PDL) enlargement (yes/no); external and internal root resorptions (yes/no); and pulp canal width: abnormal (enlarged/obliterated) or normal.
Conventional radiographs were examined on the light viewing box and digital images directly on the laptop monitor, with each digital image approximately eight (for the #2 size film) and 9.7 (for the #0 size film) times larger than the original radiograph (in diagonal distance). After examining the digital images as they were taken by the camera, they were enhanced by manoeuvering the contrast and brightness for further comparison with the unenhanced images and the original radiographs, and re-evaluated for the same parameters.
Two experienced paediatric dentists evaluated the plain-film radiographs and the digital images, after calibration. Calibration was carried out before the study, with the examiners evaluating five pairs of bitewings not included in this study.
Image sequencing was the same for both evaluators. Films and digital images were examined on different days. Evaluators used a magnifying glass or magnifying loupes, ranging from ×2:5 to ×3:5, freely. Scores were recorded once consensus was reached.
Statistical analysis for comparison between scores for each image mode (conventional, digital and enhanced digital) was carried out using JMP software (Version 3.2.6., JMP Application Co., SAS Institute, Cary, NC, USA). The level of significance for chi-square analysis was set at p <0.05.
Results
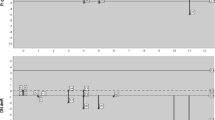
Distribution scores for presence of proximal caries, lesion depth and treatment decision in the bitewings, digital images and enhanced digital images are shown in Table 1. More proximal lesions were observed on the plain-film radiographs and on the enhanced digital images than on the unenhanced digital images. However, these differences were not statistically significant.
The percentage of carious lesions extending to one-half of the enamel width was similar in the three image modes, while the percentage of decisions to restore the cavities was close. No difference was found in the number of proximal carious lesions or periapical lesions in the anterior periapical radiographs and their digital and enhanced digital images.
Table 2 demonstrates the distribution scores for PDL enlargement, external root resorption and pulp canal width in the anterior periapical radiographs, on digital images, and on enhanced digital images. PDL enlargement was more prevalent in the digital and enhanced images than in the conventional radiographs, although the scores did not reach statistical significance. No significant difference was found between the conventional and digital images regarding external root resorption. However, enhanced digital images resulted in significantly more diagnoses compared with conventional radiographs. Pulp canals were significantly more abnormal (enlarged or obliterated) in the digital and enhanced digital images compared with conventional radiographs. No significant differences appeared in the distribution of abnormal/normal canals between both digital imaging groups.
Discussion
The present study did not show differences among plain-film bitewing radiographs and digital images for the diagnosis of caries, lesion depth and treatment decision. However, diagnoses of PDL enlargement, external root resorption and pulp canal width were more prevalent with digital images, which may suggest more accuracy in the digitised images and computer-enhancement procedures regarding root parameters. This shows a major advantage of digitising radiographs over conventional radiographs as previously reported.1,2,3,4,5,6 However, the reason for the difference may originate from another source. The outcome of the digitisation of film-based radiographs may be subject to a number of variables, including the type of camera and exposure resolution selected.14 A Nikon D70S camera was used in the present study, and digitised pictures stored in a JPEG mode.
Since images in JPEG form are compressed by the camera, it is quicker to save to memory and enables the operator to store more pictures. However, in the process of image compression some of the colour information may be lost. For example, when the processor recognises large areas of similar colour, it may choose an average of the pixels that make up the colour to represent the entire area, discarding some of the subtle hues originally captured. Therefore, it is possible that the JPEG files may be responsible for the difference in the diagnosis of root parameters. A reduced dynamic range (grey shades) could occur, which could result in increased contrast of the digitised images compared with the plain radiographs.7,15
The appearance of dental caries on a radiograph is grey. Therefore, it contains very limited dynamic range of colours. Images enhanced by adjusting brightness and contrast could overlook some subtle hues of grey, placing the image into a more dichotomised appearance of black and white. This may explain why there were nine more carious lesions diagnosed with enhanced digital images.
It is expected that higher scanning resolution might result in a higher quality of digital images. However, in subjective image evaluation this may not be the case. In one study15 where digitised images of various scanning resolutions were compared for subjective quality, most of the observers rejected the higher resolution (600 dpi) image. In the present study, the camera-obtained images were also enhanced regarding contrast and brightness.
The decision to keep the images in a JPEG mode was based on the facts that JPEG is a 'universal' file format, can be viewed on almost any computer, and can be written to memory more quickly than other modes such as Tagged Image File Format (TIFF) or RAW. Additionally, in a RAW mode, although the full range of data from the sensor can be achieved, data must still be processed on the computer before they can be used.
The appearance of enlarged PDL or pulp canal abnormalities that were more prevalent in the camera-obtained images compared to conventional radiographs can be understood considering the nature of the JPEG storing mode. In these structures, some of the data in these files may have been lost. The dynamic range of black, grey and white is prominent. Here, images enhanced by adjusting brightness and contrast could definitely overlook subtle hues of grey, placing the image into a more dichotomised appearance of black and white. Images of the proximal caries suffered less from this fault, presenting more resemblance to the conventional radiographs.
The present study has some limitations. All images were subjectively evaluated by two dentists and used the JPEG mode of image storage. Further studies are necessary using more advanced modes of image storing. TIFF, unlike JPEG, can be edited and resaved without compression loss, and RAW enables the optimal mode of image storage.
Another issue was that although the purpose of the present study was to compare the information stored in two modes of image storage, that is conventional plain-film radiographs and their digital images, there was no gold standard of diagnosis in this study. Therefore, a comparative evaluation study for images of normal anatomical structures is required.
This study showed that clinicians can use digital cameras to digitise and store radiographic images without losing important diagnostic information when there is a need to store radiographs in patient's charts and archives in a space saving manner. Professionals who move to digital imaging can digitise their existing conventional radiographs using an single lens reflex (SLR) digital camera. Further studies are recommended to clinically confirm the pathologies visually diagnosed in both the film and two sets of digital images (raw and enhanced), and to more accurately determine the camera parameters needed to preserve or improve the diagnostic quality of the film images.
Conclusion
Based on visual diagnosis of a set of plain-film radiographs and their digitised counterparts using the Nikon D70S camera, no critical diagnostic information was lost by digitising the images and using brightness and contrast enhancement. Treatment decisions did not differ after interpreting film radiographs or digital images. However, a more complete study where the pathologies are verified clinically is required.
References
Shrout M K, Potter B J, Yurgalavage M H, Hildebolt C F, Vannier M W . 35-mm film scanner as an intraoral dental radiography digitizer. I. A quantitative evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1993; 76: 502–509.
Shrout M K, Potter B J, Yurgalavage M H, Hildebolt C F, Vannier M W . 35-mm film scanner as an intraoral dental radiography digitizer. II. Effects of brightness and contrast adjustments. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1993; 76: 510–518.
Kaplan I, Dickens R L . Lightening of dark radiographs with a super proportional reducing agent. Quintessence Int 1990; 21: 737–740.
Wenzel A, Fejerskov O, Kidd E, Joyston-Bechal S, Groeneveld A . Depth of occlusal caries assessed clinically by conventional film radiographs and by digitized processed radiographs. Caries Res 1990; 24: 327–333.
Wenzel A, Larsen M J, Fejerskov O . Detection of occlusal caries without cavitations by visual inspection, film radiographs, xeroradiographs, and digitized radiographs. Caries Res 1991; 25: 365–375.
Hangiandreou N J, O'Connor T J, Felmlee T P . An evaluation of the signal and noise characteristics of four CCD-based film digitizers. Med Phys 1998; 25: 2020–2026.
Schulze R K, Rosing S T, D'Hoedt B . Contrast perception in digitized panoramic radiographs compared with their film-based origin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94: 388–394.
Parissis N, Kondylidou-Sidira A, Tsirlis A, Patias P . Conventional radiographs vs digitized radiographs: image quality assessment. Dentomaxillofac Radiol 2005; 34: 353–356.
Fuge K N, Stuck A M, Love R M . A comparison of digitally scanned radiographs with conventional film for the detection of small endodontic instruments. Int Endod J 1998; 31: 123–126.
Larson A, Lynch D A, Zeligman B et al. Accuracy of diagnosis of subtle chest disease and subtle fractures with a teleradiology system. Am J Roentgenol 1998; 170: 19–22.
Janhom A, van Ginkel F C, van Amerongen J P, van der Stelt P F. Scanning resolution and the detection of approximal caries. Dentomaxillofac Radiol 2001; 30: 166–171.
Goga R, Chandler N P, Love R M . Clarity and diagnostic quality of digitized conventional intraoral radiographs. Dentomaxillofac Radiol 2004; 33: 103–107.
Chandler N P, Pitt Ford T R, Monteith B D . Pulp size in molars: underestimation on radiographs. J Oral Rehabil 2004; 31: 764–769.
Ludlow J B, Abreu M Jr. Performance of film, desktop monitor and laptop displays in caries detection. Dentomaxillofac Radiol 1999; 28: 26–30.
Attaelmanan A, Borg E, Gröndahl H G . Digitization and display of intra-oral films. Dentomaxillofac Radiol 2000; 29: 97–102.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Peretz, B., Kaffe, I. & Amir, E. Digital images obtained with a digital camera are not associated with a loss of critical information – a preliminary study. Br Dent J 206, E9 (2009). https://doi.org/10.1038/sj.bdj.2009.182
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.182
This article is cited by
-
Digitizing an Analog Radiography Teaching File Under Time Constraint: Trade-Offs in Efficiency and Image Quality
Journal of Digital Imaging (2017)
-
Two- and tridimensional analysis of periapical repair after endodontic surgery
Clinical Oral Investigations (2015)
-
Summary of: Digital images obtained with a digital camera are not associated with a loss of critical information – a preliminary study
British Dental Journal (2009)