Key Points
-
There have been many complex and disparate international guidelines on the dental management of patients at risk of developing infective endocarditis.
-
A degree of confusion existed as a consequence among a small number of English hospital orthodontists.
-
This study supports the call for international guidelines to follow the example of the straightforward NICE guidelines published in March 2008.
Abstract
Objective To test the effect complex, multiple dental guidelines have on establishing compliance with ideal clinical practice.
Design A questionnaire was used to determine the level of knowledge of the British Cardiac Society and Royal College of Physicians 2004 infective endocarditis prophylaxis guidelines which were contemporary at the time the study was initiated, as well as to identify the existence of any written departmental policies on the safe management of patients at risk of developing this disease.
Setting Hospital Orthodontic Departments in the East of England.
Subjects and methods Fourteen consultant and nine training grade group hospital orthodontists in the East of England initially answered the questionnaire in November 2005. The results of the survey were then discussed at a subsequent regional audit meeting after which standards were agreed. The original questionnaire was then reissued in June 2006 to 13 and eight of the original consultants and training grade group orthodontists respectively. This was coincidently three months after the publication of further new infective endocarditis prophylaxis guidance from the working party of the British Society for Antimicrobial Chemotherapy.
Results The initial results indicated a number of significant deficiencies in the knowledge of which dental procedures either did or did not need antibiotic prophylaxis that the subsequent audit then improved to a variable extent. Nevertheless, the general finding was one of persistent confusion regarding the multiple conflicting contemporaneous guidelines. This lends further support to the concept of converging guidelines which remain disunified, complex and non-evidence based.
Conclusions The results of this audit confirm that compliance with preferred clinical practice is noticeably compromised when complex conflicting guidelines from either different national or international authoritative bodies exist for the same condition. With particular regard to the dental guidance for infective endocarditis prophylaxis, this has now been largely circumvented in the United Kingdom by the publication of a single, unambiguous guideline from the National Institute of Health and Clinical Excellence (NICE) in March 2008.
Similar content being viewed by others
Introduction
Infective endocarditis (IE) is an uncommon but potentially fatal disease, and while antibiotic prophylaxis prior to some dental procedures was conventional in the United Kingdom (UK) until recently, the tenuous, if not over-emphasised link with dental treatment was beginning to be both scientifically challenged,1,2,3 and acknowledged in civil law.4
Nevertheless, throughout the history of IE prophylaxis, professional organisations have sought to identify and stratify the groups of patients considered to be at risk, as well as list those procedures for which antibiotic cover should be supplied,5,6,7,8,9,10 although none of them have ever reached complete consensus with each other.11
For a long time the UK dental guidelines for IE had been based on the 1993 guidance issued by the British Society of Antimicrobial Chemotherapy (BSAC),5 which was published in the British National Formulary (BNF). Nevertheless, by May 2004 extensive new IE guidelines issued jointly by the British Cardiac Society and the Royal College of Physicians (BCS RCP) had emerged.6
One of the main changes they introduced was the abandonment of the presumption that all dental procedures that cause significant bleeding would need antibiotic cover in patients susceptible of developing IE. This was because research had shown that bleeding following dental treatment was a poor predictor of odontogenic bacteraemia.2
Instead the guidance introduced the concept that any dento-gingival manipulation which resulted in a statistically significant different bacteraemia from a pre-procedure baseline reading would require antibiotic cover, whether it was bloodless or not.10
The aim of this study was therefore to survey the level of knowledge and understanding of these extensive guidelines amongst hospital orthodontists and to audit whether the amount of detail they contained might otherwise have detracted clinicians from achieving full compliance with the recommended IE protocols at the time, and so act as a general indicator of the potential effectiveness for these and any other complex dental guidelines that exist.
Subjects and methods
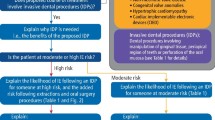
In November 2005, 14 consultant and nine training grade group (TGG) East of England hospital orthodontists completed a questionnaire on IE. They were asked whether specific written protocols on the orthodontic management of patients at risk of developing IE were available in their departments, and they were also asked to identify from a list of dental and orthodontic procedures those which according to the BCS RCP IE 2004 recommendations either would or would not require antibiotic cover.
After discussing the findings of the initial survey at a subsequent regional meeting, together with receiving education on the content of these recommendations, it was agreed that an audit would be undertaken. Because it had been previously stated that these guidelines would 'provide dental practitioners with an easily accessible and easy to use method of identifying patients who require antibiotic prophylaxis, confirmation of the dental procedures requiring antibiotic prophylaxis, and the drug regimens required'10 it was decided to test this supposition by auditing how well the clinicians performed using their new knowledge of which dental procedures of relevance to the practice of orthodontics either would or would not require antibiotic cover for patients at risk of developing IE.
As a consequence, in June 2006 the same questionnaire was re-issued to the consultants and TGGs to complete. However, in the interim one consultant and one TGG had resigned which left 13 and eight of the original clinicians respectively to audit.
In addition, different new IE guidelines had once again appeared three months earlier in the preceding April, following a publication by the BSAC Working Party. In essence, these de-emphasised the risk of a bacteraemia arising from a single procedure in the causation of IE, placing more emphasis instead on the risk of cumulative exposure to bacteraemias from poor oral health, toothbrushing and chewing,7 all of which are shared sentiments that are contained within the current American Heart Association (AHA) guidelines.8
Results
Management protocols for patients at risk of developing IE
Tables 1 and 2 illustrate the clinical protocols that were used for managing patients at risk of developing IE both at the time of the initial survey and during the audit for the consultants and the TGGs. In the first instance, about a fifth of the consultants had specific IE departmental policies, of which a similar fraction of the TGGs were cognisant of. Then during the audit, just over three quarters of the consultants had developed such policies, yet at that stage only about a third of the TGGs were aware of them.
With regard to the contemporaneous need to supervise patients taking their pre-treatment antibiotic prophylaxis as well as the use of a pre-procedure mouth rinse of 0.2% chlorhexidine, both predominated amongst the two groups of clinicians on both occasions.
Knowledge of which dental and orthodontic procedures required antibiotic prophylaxis in patients at risk of developing IE
Tables 3 and 4 show that the consultant and TGG understanding of the general concept that not all dental procedures which result in gingival bleeding would require antibiotic cover and vice versa both improved during the audit. In addition, these tables demonstrate the number and percentage of consultants and TGGs who correctly identified those procedures which the BCS RCP IE 2004 guidelines recommended would require antibiotic prophylaxis for any resultant bacteraemias that would otherwise be significantly above the pre-procedure baseline levels, as well as those that would not.
In the initial survey, the consultants and TGGs respectively answered an average of 67% and 68% of all of these questions correctly. The performance of these two groups during the audit then improved by just over 10%, as the consultants and TGGs respectively answered a mean of 78% and 80% correctly.
Discussion
While the number of participants in this audit was quite small, some interesting observations can still be made. It was rewarding to see that 56% more consultants had developed IE departmental policies on how to manage patients at risk as a consequence of knowing they would be audited (Table 1). However, the subsequent communication of this with their postgraduate trainees was somewhat remiss, as only 15% more of the TGGs subsequently became aware of their existence (Table 2).
As recommended by the BNF which was current at the time of the study,12 the protocol that patients should be witnessed taking their pre-procedure antibiotic cover by either the dentist or the dental nurse predominated at the initial survey and during the audit, although on the second occasion while this appreciation fell slightly amongst the consultants, it rose in contrast to include all of the TGGs (Tables 1 and 2).
Up until then, even though a number of studies had shown no significant reduction in bacteraemias as a result of using a pre-treatment chlorhexidine mouth rinse,13,14 it nevertheless remained a contemporaneous BNF recommendation,12 as was the case in other publications specifically relating to the orthodontic management of patients at risk of developing IE.15,16
That the practices of witnessing pre-procedure antibiotic administrations together with the use of antiseptic mouth rinses were widespread amongst both the consultants and the TGGs at the initial survey and during the subsequent audit was therefore good evidence of protocol compliance with simple, clear guidelines (Tables 1 and 2).
In relation to the extensive list of dental procedures which required antibiotic prophylaxis as per the BCS RCP IE 2004 recommendations, two thirds of the consultants and the TGGs overall correctly identified those which would need to be covered in the initial survey, which then rose to over three quarters of them during the audit.
In comparison, this performance was better than that found in a recent study which evaluated the knowledge of 528 Welsh dental practitioners with respect to a different set of IE guidelines, as contained within the BNF that was current at the time. Of the 33 Hospital Dental Service practitioners within that study's main group, they answered on average 53% of the questions correctly as to which dental procedures would require antibiotic cover.17
Nevertheless, despite this study's participants having been given specific education on which dental and orthodontic procedures produce profound bacteraemias, such as polishing teeth with a rubber cup, scaling, and placing an orthodontic separator,16,18 that the subsequent audit only produced a modest improvement in both groups overall, if not with some isolated examples of actual deterioration, clearly demonstrates the effect complex guidelines have on not being able to reliably achieve complete compliance with preferred clinical practice, especially if different guidelines exist for the same condition contemporaneously.
As a consequence, this audit and the findings of the other IE study17 both support the overall observation that when different guidelines are available, confusion amongst clinicians prevails on how best to proceed.19
However, even though this has now been largely circumvented in the UK by the publication of un-ambiguous IE guidance from the National Institute of Health and Clinical Excellence in March 2008, which recommends nil antibiotic prophylaxis for any dental procedure,20 documented episodes where clinicians are encountering compliance resistance from patients and other colleagues are now beginning to emerge.21 Indeed, under English law, any dentist who decides not to follow up-to-date guidance may be required to justify their decision either to the General Dental Council or a legal court in the event of a complaint or a claim for damages being made.21 This is because the test of liability in relation to the outcome of any treatment is set out in the House of Lords decision of Sidaway.22 In this regard clinicians have to act in accordance not only with a practice accepted at the time as proper by a responsible body of medical opinion (the Bolam test),23 but also with the Bolitho modification,24 that the body of opinion should be reasonable and responsible and the opinion should be logical.25
For those UK clinicians who may choose to adhere to the AHA IE guidelines and still prescribe prophylactic antibiotic cover in limited circumstances, namely for all dental procedures that involve manipulation of the gingival tissue, the periapical region of teeth or the perforation of the oral mucosa, for a number of high risk category patients which are defined,8 it could be argued that their practice would still qualify as being in accordance with a responsible body of opinion, even though it would be contrary to the latest NICE guidance. However, if a claim were ever to arise as a consequence of such practice, it would be down to the judiciary to determine if that body of opinion remained reasonable, responsible and logical.
Unfortunately this will provide little solace for dentists who practice outside of the UK's judicial system, as their level of uncertainty as to which IE guideline to follow will most likely have increased, given the polarisation that now exists between the 2007 AHA and the new 2008 NICE guidance.
Conclusions
The results of this audit confirm that compliance with preferred clinical practice is noticeably compromised when complex, conflicting guidelines from either different national or international authoritative bodies exist for the same condition.
With particular regard to the dental guidance for IE, these results and those from an earlier study17 have shown that lack of guideline standardisation results in sub-optimal clinical practice as a result of generalised confusion. Both of these studies therefore support the sense of guideline convergence, and to this end, hopefully other countries will soon adopt a similar IE prophylaxis policy to the one which now prevails in the UK.
References
Strom B L, Abrutyn E, Berlin J A et al. Dental and cardiac risk factors for infective endocarditis. A population-based, case-control study. Ann Intern Med 1998; 129: 761–769.
Roberts G J . Dentists are innocent! 'Everyday' bacteremia is the real culprit: A review and assessment of the evidence that dental surgical procedures are a principal cause of bacterial endocarditis in children. Pediatr Cardiol 1999; 20: 317–325.
Martin M V . A victory for science and common sense. The new guidelines on antimicrobial prophylaxis for infective endocarditis. Br Dent J 2006; 200: 471.
Martin M V, Longman L P, Forde M P, Butterworth M L . Infective endocarditis and dentistry: the legal basis for an association. Br Dent J 2007; 203: E1.
Simmons N . Recommendations for endocarditis prophylaxis. The Endocarditis Working Party for Antimicrobial Chemotherapy. J Antimicrob Chemother 1993; 31: 437–438.
Ramsdale D R, Turner-Stokes L. Prophylaxis and treatment of infective endocarditis in adults: a concise guide. Clin Med 2004; 4: 545–550.
Gould F K, Elliott T S J, Foweraker J et al. Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2006; 57: 1035–1042.
Wilson W, Taubert K A, Gewitz M et al. Prevention of infective endocarditis. Guidelines from the American Heart Association. Circulation 2007; 116: 1736–1754.
Dajani A S, Taubert K A, Wilson W et al. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. JAMA 1997; 277: 1794–1801.
Roberts G J . New recommendations on antibiotic prophylaxis of infective endocarditis. Ann R Coll Surg Engl 2004; 86 suppl: 163.
Martin M V . Dear confused dentist. Dent Pract 2006; 44: 1, 4.
British National Formulary, September ed. London: BMJ Publishing Group Ltd and RPS Publishing, 2005.
Lockhart P B . An analysis of bacteremias during dental extractions. A double-blind, placebo-controlled study of chlorhexidine. Arch Intern Med 1996; 156: 513–520.
Erverdi N, Acar A, Isguden B, Kadir T . Investigation of bacteremia after orthodontic banding and debanding following chlorhexidine mouth wash application. Angle Orthod 2001; 71: 190–194.
Khurana M, Martin M V . Orthodontics and infective endocarditis. Br J Orthod 1999; 26: 295–298.
Roberts G J, Lucas V S, Omar J . Bacterial endocarditis and orthodontics. J R Coll Surg Edinb 2000; 45: 141–145.
Thompson S A, Davies J, Allen M et al. Cardiac risk factors for dental procedures: knowledge among dental practitioners in Wales. Br Dent J 2007; 203: E21.
Lucas V S, Omar J, Vieira A, Roberts G J . The relationship between odontogenic bacteraemia and orthodontic treatment procedures. Eur J Orthod 2002; 24: 293–301.
Martin M V . Confusing guidelines. Br Dent J 2006; 201: 615.
Prophylaxis against infective endocarditis. NICE Report No: CG064. London: National Institute of Health and Clinical Excellence, 17 March 2008.
Harvey B . NICE guidance on antibiotic prophylaxis. Dentistry 2008; 9: 45.
Sidaway v Board of Governors of the Bethlem Royal Hospital 1985. 1 AC 871.
Bolam v Friern Hospital Management Committee. 1957 1 WLR 582 2 All ER 118.
Bolitho v City and Hackney Health Authority. 1998 AC 232.
Boynton S . Don't just sign here. Dent Protect Service Matters 2006; 4: 1–3.
Acknowledgements
My thanks to Graham Roberts as one of the members of the British Cardiac Society Guidelines Advisory Group, for his helpful clarification of certain aspects and some definitions contained within the BCS RCP IE 2004 recommendations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Chate, R. An infective endocarditis audit illustrates why dental guidelines in general need to be kept clear, simple and unambiguous. Br Dent J 205, 331–335 (2008). https://doi.org/10.1038/sj.bdj.2008.805
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.805
This article is cited by
-
Endocarditis prophylaxis in daily practice of pediatricians and dentists in Flanders
European Journal of Pediatrics (2021)