Abstract
Study design:
This study was a cross-sectional, follow-up survey.
Objectives:
To examine the role of importance of religion and spiritual coping on life satisfaction in adults with pediatric-onset spinal cord injury (SCI).
Setting:
This study was carried out in a specialty hospital system.
Methods:
Individuals who sustained an SCI before age 18 completed a structured telephone interview at ages 24–45. Demographic/medical questionnaires along with standardized measures were administered: Brief COPE, FIM, Craig Handicap Assessment and Reporting Technique (CHART), 12-item Short-Form Health Survey (SF-12) and Satisfaction with Life (SWL) scales. Spirituality was measured with a question assessing importance of religion and using the spiritual coping domain of the Brief COPE.
Results:
A total of 298 individuals (62% men; 56% with tetraplegia) participated in this study. Approximately half (141) of the participants reported that religion is ‘important to very important’ to them and 55% (163) used spiritual coping. Importance of religion and spiritual coping was significantly associated with older age (P<0.01), longer duration of injury (P<0.01) and higher SWL (P<0.05). Importance of religion was also related to higher SF-12 mental component (P<0.05). Spiritual coping was negatively associated with motor independence (P<0.05) and CHART occupation (P<0.05). Moreover, spiritual coping emerged as a predictor of SWL, whereas importance of religion did not.
Conclusion:
Over half of the participants endorsed importance of religion and the use of spiritual coping. Spiritual coping, in particular, may serve a unique role in promoting SWL. Consequently, assessment of spirituality needs to become a standard part of care in the treatment of individuals with SCI and the use of spirituality-focused interventions to promote SWL should be explored.
Similar content being viewed by others
Introduction
Although there is considerable debate regarding the definitions of ‘religion’ and ‘spirituality’,1 there is growing evidence that religion and spirituality serve as possible protective factors against various negative health outcomes.2, 3 Most commonly, ‘religiosity’ is considered the formal, institutional and outward expression of faith and measured by variables such as importance of religion and frequency of religious service attendance.3 ‘Spirituality’, however, is a subjective experience that exists both within and outside the traditional religion. Spirituality can be defined as the internal, personal and emotional expression of the sacred and measured by spiritual or religious coping and peace and comfort derived from faith.1, 3
Much of the existent literature examines the link between religiosity/spirituality and physical health in adults with life-threatening and terminal conditions;4 however, there are limited data on the importance of religiosity and spirituality in rehabilitation.4, 5 Of the few studies that have examined religious and spiritual factors in rehabilitation populations, significant relationships have emerged. For example, adults who were admitted to hospital for stroke rehabilitation and who scored high in religious and spiritual beliefs endorsed lower levels of anxiety and depressive symptoms than less religious/spiritual individuals.6 Increased spirituality in adults with non-acute traumatic brain injury was associated with positive psychological coping strategies.7 In studies with a sample of heterogeneous adult rehabilitation patients, including individuals with spinal cord injury (SCI), increased spirituality was associated with higher levels of quality of life and increased life satisfaction.8, 9 Studies focusing exclusively on individuals with SCI are even more limited. Brillhart10 found a significant correlation between a psychological/spiritual domain of a quality of life measure and life satisfaction. Another SCI study noted that existential spirituality (that is, individuals' search for purpose and meaning in their lives) was related to life satisfaction, general health-related quality of life and social integration; however, religious spirituality (that is, relationship with a higher power) was not related to these outcomes.5
Although much of the literature describes a positive impact of religiosity and spirituality on health, a limited number of studies suggest that some rehabilitation patients may turn away from religion/spirituality. In a heterogeneous sample of adult rehabilitation patients, religion did not promote better recovery or adjustment, and negative religious coping and anger with God were risk factors for a poor recovery.11 Moreover, approximately one-third of a heterogeneous rehabilitation group reported a significant decline in spiritual well-being over time.12
To the best of our knowledge, data on the role of religion and spirituality on emotional health in individuals with pediatric-onset SCI are nonexistent. This group of individuals is unique in that they have grown up with an SCI. Moreover, a primary goal of pediatric SCI rehabilitation programs is to facilitate positive psychological adjustment and promote adaptive coping strategies so that youth can lead satisfying and productive adult lives.13 Understanding factors associated with physical and emotional well-being, such as religion and spirituality, can help identify individuals at risk for poor outcomes. Therefore, the purpose of our study was to assess the impact of religion and spiritual coping on life satisfaction in individuals with pediatric-onset SCI. We hypothesized that individuals who describe religion as meaningful to them and who use spiritual coping will experience greater life satisfaction. This work aims to expand on current knowledge on religion/spirituality in the field of rehabilitation and provide new data to the pediatric literature so as to guide the development of pediatric interventions designed to facilitate positive adjustment and long-term outcomes.
Materials and methods
Participants were individuals who sustained an SCI at 18 years of age or younger, were 24 years of age or older at time of interview and were former patients at one of the three pediatric SCI programs (Shriners Hospitals for Children (SHC) Chicago, Philadelphia and Northern California), which treat children throughout the United States, Canada and Mexico. Participants were part of a larger longitudinal investigation of outcomes of pediatric-onset SCI and were identified through the hospital system's SCI database. Exclusionary criteria included non-English-speaking patients and individuals with a significant traumatic brain injury or severe cognitive limitations. Informed consent was obtained before conducting telephone interviews. This study was approved by the institutional review board at all three hospitals and is registered in a public access database at www.clinicaltrialsgov.
Measures
Demographic and medical characteristics
A structured questionnaire designed for this study was used to collect demographic and pain information. Injury-related information and medical history were obtained from medical chart reviews and the hospital system's SCI database.
FIM
FIM (The service marks and trademarks associated with the FIM instrument are all owned by Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities Inc. (‘UDSMR’). The use of the FIM instrument to collect data for this research study was authorized and conducted in accordance with the terms of a special purpose license granted to Licensee by Uniform Data System for Medical Rehabilitation a division not been processed by of UDSMR. The patient data collected during the course of this research study have UDSMR. No implication is intended that such data have been or will be subjected to UDSMR's standard data processing procedures or that it is otherwise comparable to data processed by UDSMR) The telephone version of the FIM was used to assess independent performance in self-care, sphincter control, transfers, locomotion, communication and social cognition.14 The Motor domain, consisting of self-care, transfers, locomotion and sphincter control, was used for these analyses. Items are scored on a Likert scale ranging from 1 (total assistance) to 7 (complete independence).
Craig Handicap Assessment and Reporting Technique
This measure of social and community participation for individuals with physical disabilities comprises six areas: physical independence, cognitive independence, mobility, occupation, social integration and economic self-sufficiency.15 The maximum score for each domain is 100 and indicates less handicap or higher social and community participation.
SF-12 Health Survey
Self-perception of general health status was assessed with the 12-item Short-Form Health Survey (SF-12), which generates physical and mental component summary scores.16 Only the mental component summary score was used for these analyses. Scores range from 0 to 100, with higher scores indicating greater perceived health.
Importance of religion
Importance of religion was assessed using a Likert scale ranging from 1 (not important) to 5 (very important). For data analysis, we collapsed the responses into two groups: 1–3 versus 4–5.
Brief COPE
This self-report measure of adaptive and maladaptive coping skills was modified to measure coping to an SCI.17 Each item is scored on a Likert scale ranging from 1 (not at all) to 4 (do this a lot). Only the spiritual coping domain was used for these analyses, which is defined by two statements: ‘I’ve been trying to find comfort in my religion or spiritual beliefs' and ‘I've been praying or meditating.’ Domain scores range from 2 to 8, with higher scores indicating greater use of the coping skill.
Satisfaction with Life scale
Subjective global life satisfaction was assessed with the Satisfaction with Life scale, which consists of five statements each rated on a Likert scale from 1 (strongly disagree) to 7 (strongly agree).18 Scores range from 5 to 35, with higher scores indicating greater life satisfaction.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Data analytic plan
Summary statistics were used to describe the sociodemographic, medical and psychological characteristics of the participants. Correlational analyses were computed with Pearson's product (r) and Spearman's rank correlation (rs). Step-wise regression analyses were used to identify predictors of life satisfaction. Confounding variables were entered in the first step. Importance of religion and spiritual coping was entered in the second step. Analyses were conducted using SPSS statistical package version 17.0 (Chicago, IL, USA).
Results
Response rates
Of the 668 patients in the hospital system's SCI database, 404 (60.5%) patients were part of the larger longitudinal study. Compared with nonparticipants, participants were more likely to be women (P=0.001), Caucasian (P<0.001) and had tetraplegia (P=0.015). Reasons for nonparticipation included death (n=54), lack of interest (n=97) or inability to be located (n=113). As the Brief COPE was added later in the study, 298 (74%) participants completed this measure and therefore were included in data analyses. There were no significant differences in gender, race, age at injury, level or impairment of SCI between those who completed and those who did not complete the Brief COPE.
Demographic and medical characteristics
Table 1 reports the main characteristics of the 298 participants.
Religion and spiritual coping
Approximately half (141) of the participants reported that religion is ‘important to very important’ to them. Mean spirituality coping score was 5.14 (s.d.=2.32, range 2–8), with 55% (163) of respondents using spiritual coping ‘a medium amount to a lot’. Several statistically significant relationships were noted for importance of religion and spiritual coping but these correlations were not robust (Table 2). Importance of religion was positively correlated with age, duration of injury, mental component summary (SF-12) and life satisfaction. Positive correlations were also found between spiritual coping and age, duration of injury and life satisfaction. Spiritual coping was negatively correlated with FIM motor and Craig Handicap Assessment and Reporting Technique (CHART) occupation.
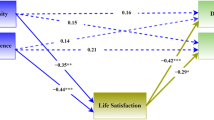
Predictors of life satisfaction
A stepwise regression analysis was performed using life satisfaction as the outcome variable. Confounding variables were entered at step one: age, marital status, duration of injury, FIM motor, CHART occupation, pain and SF-12 mental component summary score. Importance of religion and spiritual coping was entered at step two. Results of the regression analysis are shown in Table 3. The model explained 40% of the variance in life satisfaction, F(9, 288)=21.05, P<0.001. Significant individual contributions were found for greater perceived mental health, being married/having domestic partner, greater occupational participation, lower incidence of pain and greater motor functioning. As hypothesized, greater use of spiritual coping predicted life satisfaction after controlling for confounding variables. Importance of religion did not emerge as a predictor of life satisfaction.
Discussion
This study of adults with pediatric-onset SCI suggests the importance of religion and spirituality on life satisfaction. To the best of our knowledge, this is the first study that focused specifically on individuals with pediatric-onset SCI. These findings are consistent with current adult rehabilitation literature, in that religion and spirituality have a positive impact on emotional functioning,6, 7, 8, 9, 10, 19 and suggest that religion and spirituality can have an integral role in the SCI rehabilitation process. Spiritual coping, in particular, may help facilitate adaptive coping to an SCI and consequently, improve life satisfaction. Therefore, the rehabilitation environment should aim to promote religious/spiritual practices in accordance to patients' beliefs.
Consistent with our hypothesis, spiritual coping emerged as a predictor of life satisfaction after controlling for confounding variables in adults with pediatric-onset SCI. In contrast, importance of religion did not make a unique contribution. Previous research has suggested a relationship between religion and emotional well-being; however, the findings of our study suggest that spiritual coping may have a more substantial relationship than religion with life satisfaction. It is possible that the use of spiritual coping strategies may enhance self-empowerment and reshape a sense of meaning in life thereby helping an individual to experience greater life satisfaction. Moreover, it is not just maintaining religious beliefs but using spiritual resources, which facilitates adjustment to the SCI and provides new life meaning.
Although spirituality was a significant predictor of life satisfaction in this population of adults with pediatric-onset SCI, it contributed to only 3% of the variance in life satisfaction. In contrast, perceived mental health, marriage, participation in occupational activities, pain and functional impairment (FIM motor) accounted for 37% of the variance in life satisfaction. Therefore, to improve life satisfaction, these factors also need to be addressed during rehabilitation. For example, interventions aimed at decreasing pain/improving pain management coping strategies or improving overall emotional health would be expected to improve life satisfaction. Similarly, life satisfaction could be improved through interventions designed to increase participation in activities such as work or school as well as social engagements. Finally, life satisfaction could be enhanced by interventions that improve function in those with greater impairment, such as upper extremity surgeries to improve hand function.
Findings and limitations from this study serve as stepping-stones for future research in the area of religion/spirituality and pediatric rehabilitation. Our measures of religion and spirituality provide insight on only some elements of these complex constructs. Future studies would benefit from a more in-depth investigation of religion and spirituality in pediatric patients with SCI, including the use of more comprehensive spirituality-specific measures, such as the Spiritual Well-Being Scale. Although this study was part of a longitudinal study, findings described were using cross-sectional data. As change is a constant in childhood and adolescent development, longitudinal studies are warranted to examine the roles of religion and spirituality as mediators of emotional functioning over time. Moreover, as our data indicated that spiritual coping affects life satisfaction, future studies are needed to assess the efficacy of spiritual coping interventions as components of comprehensive rehabilitation programs. Developing developmentally appropriate interventions for children with SCI is particularly important and challenging as they navigate the demands of adolescence and transition to adulthood. Finally, the inclusion of former patients from a single hospital system that could be located and were willing to participate is a study limitation. Although the three hospitals are at various locations in the United States, have a large catchment area and treat patients with diverse socio- and economic backgrounds, generalizations about spirituality and life satisfaction of other populations are not possible. Inclusion of a more diverse sample in future studies is indicated.
In summary, data from this study suggest that the life satisfaction of youth and adults with SCI may be improved by assessing and fostering spirituality as part of the standard care of these individuals.
References
Hill PC, Pargament KI . Advances in the conceptualization and measurement of religion and spirituality: implications for physical and mental health research. Am Psychol 2003; 58: 64–74.
Cotton S, Zebracki K, Rosenthal S, Tsevat J, Drotar D . Religion/spirituality and adolescent health outcomes: a review. J Adolesc Health 2006; 38: 472–480.
Koenig H, McCullough M, Larson D (eds). Handbook of Religion and Health. Oxford University Press: New York, NY, 2001.
Johnson B, Yoon D . Relationship between the Brief Multidimensional Measure of Religiousness/Spirituality and health outcomes for a heterogenous rehabilitation population. Rehabil Psychol 2009; 54: 422–431.
Matheis E, Tulsky D, Matheis R . The relation between spirituality and quality of life among individuals with spinal cord injury. Rehabil Psychol 2006; 51: 265–271.
Giaquinto S, Spiridigliozzi C, Caracciolo B . Can faith protect from emotional distress after stroke? Stroke 2007; 38: 993–997.
Mahalik JL, Johnstone B, Glass BA, Yoon DP . Spirituality, psychological coping, and community integration for persons with traumatic brain injury. J Religion Disabil Health 2007; 11: 65–77.
Riley BB, Perna R, Tate DG, Forchheimer M, Anderson C, Leura G . Types of spiritual well-being among person with chronic illness: their relations to various forms of quality of life. Arch Phys Med Rehabil 1998; 79: 258–264.
Tate DG, Forchheimer M . Quality of life, life satisfaction, and spirituality. Am J Phys Med Rehabil 2002; 81: 400–410.
Brillhart B . A study of spirituality and life satisfaction among persons with spinal cord injury. Rehabil Nurs 2005; 30: 31–34.
Fitchett G, Rybarczyk BD, DeMarco GA, Nicholas JJ . The role of religion in medical rehabilitation outcomes: a longitudinal study. Rehabil Psychol 1999; 44: 333–353.
Kim J, Heinemann AW, Bode RK, Sliwa J, King RB . Spirituality, quality of life, and functional recovery after medical rehabilitation. Rehabil Psychol 2000; 45: 365–385.
Vogel LC, Anderson CJ . Spinal cord injuries in children and adolescents: a review. J Spinal Cord Med 2003; 26: 193–203.
Uniform Data System for Medical Rehabilitation. The Guide for Uniform Data Set for Medical Rehabilitation (including the FIM™ Instrument). UDSMR: Buffalo, 1997.
Whiteneck GG, Charlifue SW, Gerhart KA, Overhosler JD, Richardson GN . Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil 1992; 73: 519–526.
Ware JE, Kosinski M, Keller SD . A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233.
Carver CS . You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med 1997; 4: 92–100.
Diener E, Emmons R, Larsen J, Griffin S . The satisfaction with life scale. J Pers Assess 1985; 49: 71–75.
McColl MA, Bickenbach J, Johnston J, Nishihama S, Schumaker M, Smith K et al. Changes in spiritual beliefs after traumatic disability. Arch Phys Med Rehabil 2000; 81: 817–823.
Acknowledgements
We thank the Dr Randal Betz and Dr Craig McDonald for their collaboration with this study, as well as the anonymous reviewers for their valuable comments on an earlier draft. We are grateful to Shriners Hospitals for Children, Chicago, which funded this study. Most importantly, we acknowledge the contributions of our former patients who graciously participated in our research over many years.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chlan, K., Zebracki, K. & Vogel, L. Spirituality and life satisfaction in adults with pediatric-onset spinal cord injury. Spinal Cord 49, 371–375 (2011). https://doi.org/10.1038/sc.2010.80
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.80
Keywords
This article is cited by
-
Between Presence and Commitment: A Qualitative Exploratory Study of People with Visual Impairment in Polish Religious Communities
Journal of Religion and Health (2023)
-
Relationship Between Spirituality, Religiosity, and General Life Satisfaction Among Canadians Living with Neurological Conditions in New Brunswick and Manitoba
Journal of Religion and Health (2022)
-
The Effect of Spiritual Well-being on Hope in Immobile Patients Suffering From Paralysis Due to Spinal Cord Injuries
Journal of Religion and Health (2022)
-
The role of spirituality in spinal cord injury (SCI) rehabilitation: exploring health professional perspectives
Spinal Cord Series and Cases (2018)
-
Coping strategies recalled by young adults who sustained a spinal cord injury during adolescence
Spinal Cord (2012)