Abstract
Objective:
To develop an interactive computer program that facilitates uniformity and accuracy in the collection and assessment of spinal cord-impairment data.
Design:
A computer program that captures and processes clinical examination information in graphical form using the 2002 American Spinal Injury Association (ASIA) guidelines. This program calculates motor and sensory level, neurological level, the ASIA impairment scale (AIS) grade and zone of partial preservation.
Participants/Methods:
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) were encoded and a graphic representation of the standard ASIA data-capturing form (with permission) was produced using Adobe Flash programming technology by the Division of Multimedia at the University of Saskatchewan.
Results:
Testing by the development team has been successful in producing accurate ASIA-impairment data.
Conclusion:
Adapting the ISNCSCI system to a computer-generated format is possible and will promote uniformity in the collection and interpretation of impairment data. This program can also be used to educate health-care personnel, including residents and medical students, on classifying the impairment in traumatic spinal cord injury.
Similar content being viewed by others
Introduction
With the development of an instrument that standardizes the neurological classification of spinal cord injury, the American Spinal Injury Association (ASIA) established a model for the uniform assessment and description of impairment in this patient group. The importance of adopting a standard approach was identified by Guttman and Michaelis1 in 1969. This led to further development of a data set that was both quantified and qualified with respect to measuring impairment. An added benefit of establishing a standard approach was to aid many allied clinical specialists, such as physiatrists, neurologists, orthopedic surgeons, neurosurgeons, other health-care professionals and researchers, in examining a spinal cord-injured patient and communicating their findings consistently.
The ASIA impairment classification system was adopted in 1982 under the leadership of Samuel Stover and the National Database for the Model SCI Centers. Since then, it has undergone a number of revisions designed to more accurately describe the severity of a spinal cord injury, including key muscle and sensory points to be examined. These changes were initiated because of continued discrepancies among clinicians and investigators.2 Its utility as a resource tool was shown by Walker3 in 1991. He showed that clinical outcomes became more predictable and had been used in justifying efficient use of hospital care and in multi-centered trials. The classification system was adopted by the International Spinal Cord Society in 1992, when it was renamed the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI). The last update of the ISNCSCI was carried out in 2002.4, 5
In order to use the classification system in its present form, it is important that the clinician accurately completes the physical examination, records the findings and interprets the results using the most up-to-date guidelines. Although widely in use, and objective in scope, it is recognized that the interpretation and implementation of the rules may not be consistent among clinicians, thus affecting its inter-rater reliability.6 In addition, we were concerned that some health-care providers may not be aware of updates that have been implemented over the years.
To address these issues, this project focused on developing a computerized algorithm capable of capturing information on clinical spinal cord injury examination, processing it with the current ASIA guidelines and calculating an injury level and impairment rating. The ultimate objective was to promote the use of the ISNCSCI among all health-care providers of spinal cord injury, ensure uniformity in its use on a national and international level, and develop an interactive tool useful for teaching the impairment rating system.
Description of program—overview
The ISNCSCI program was designed in its entirety in Adobe Flash7 (formerly Macromedia Flash). The logic and the algorithm is coded in Actionscript, which is the programming language used by Adobe Flash. It can be run as an executable file for Windows users or as a projector file for Macintosh users. The user will need to have a screen resolution that is ⩾800 × 600 pixels, as well as a keyboard and mouse. To view the program online, this program can be delivered within a web browser, such as Internet Explorer, Firefox or Safari. However, an updated Flash Player plug-in must be installed for the program to be run. The user will need to have the Flash Player 6 plug-in or above to run this program. At the time of writing, the latest version of Flash Player available was 9, and the market penetration rates for Flash Player6 are over 96%.8 If the user require an updated Flash Player plug-in, it can be downloaded free of charge.9
In keeping with the ISNCSCI protocol there are a number of prerequisites for the examination data to be entered into the program. First, the individual being tested must have a traumatic spinal cord injury affecting a single portion of the spinal cord. Second, all abnormal scores must be due to the spinal cord injury and not due to another cause, such as peripheral nerve injury or stroke. Third, according to instructions for muscle strength grading in the ISNCSCI, strength should not be downgraded if it is due to deconditioning effort or inhibiting factors.
To use the program, the user must first agree with the disclaimer. Agreeing to do so will open a pathway to the data-capturing module. From there, an introduction screen guides the user on the procedure to follow in order to enter data. Separate modules allow the user to enter motor scores (Figure 1) and sensory scores (Figure 2). Another module can record patients' information and, if required, assistance is provided through a help module.
Motor scores can be entered directly into a chart, which is a graphical reproduction of the familiar ASIA scheme. As with the ASIA system, the Medical Research Council muscle-grading system scores are entered into text boxes that correspond to the key ASIA muscle functions. The program automatically assumes normal grades (5/5) for all text boxes. These values can be changed by using a +/− icon to reflect the actual clinical data. The program asks for the presence of voluntary anal contraction for later consideration of completeness of injury and calculates the total motor score.
Sensory score entry is facilitated by easy screen transition to the following screen. Scores representing light touch and pin-prick testing can be entered into separate screens for either the cervical, thoracic or lumbar regions. As with the ASIA scheme, sensory testing is graded from 0/2 (absent) to 2/2 (normal). A graphical representation of the patient is provided with color-coded dermatomes that correspond to the sensory scores. In this scheme, gray represents non-testable dermatomes, red corresponds to a score of 0 (unable to distinguish between sharp and dull sensation or completely absent sensation), yellow is equivalent to a score of 1 (impaired) and green translates to 2 or normal sensation. Color coding provides an immediate graphical representation of the sensory level for the spinal cord injury. Total numerical values are also calculated for pin prick and light touch.
The last module provides a summary and analysis of relevant clinical information that has been previously entered on the data-capture screens both in color-coded graphical form and also in numerical format (Figure 3). Right and left sensory and motor levels are displayed, and a calculation of the level in which sensation and motor scores are normal for pin prick, fine touch and strength testing, respectively, is carried out. The neurological level (that is, the level in which sensory and motor scores are normal) is also provided. The zone of partial preservation is indicated for patients with complete injuries (that is, absence of sensory or motor function in the lowest sacral segment). The print module provides instructions on how to print summary data. An interactive version of this program can be found at http://www.medicine.usask.ca/pmr/asia.exe/view.
Algorithm logic sequence
The classification of spinal cord injury was determined in roughly the same manner as that suggested in the reference manual for the Standards. The program is capable of calculating the following elements:
-
Sensory levels (left, right and overall),
-
Motor levels (left, right and overall),
-
Neurological levels (left, right and overall),
-
ASIA impairment scale (from A to E),
-
Complete vs incomplete injury,
-
Zone of partial preservation,
-
Sensory and motor total scores
-
Brown-Sequard syndrome.
Initially, the sensory levels for the right and left sides are determined. This is followed by the motor level for the right and left sides. The program then compares the motor level versus the sensory level in which a myotome level is not present.
After this, the single neurological level is identified. Before determining the ASIA impairment rating, the motor level is modified temporarily to reflect some of the exceptions when grading the ASIA impairment scale (AIS). This is particularly important when the possibility of an AIS C or D grade exists. In these situations, the computer must use the ‘neurological’ level as opposed to the ‘motor’ level for a portion of the calculation.
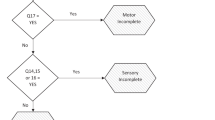
Finally, the AIS grade is determined. The program does this by identifying whether the patient had an AIS A or E grade; if neither of these is present, it determines whether an AIS grade D or C is present. If none of these four conditions exist, by a process of elimination, the program assumes that AIS grade B is present. Lastly, with a complete injury, a zone of partial preservation is identified. The complete ASIA algorithm contains roughly 3800 lines of code.
Limitations of the program
All scenarios presenting for assessment using the AIS cannot be realistically tested under ‘experimental laboratory conditions’. As a result, situations may arise in which the algorithm either cannot handle a data set or arrives at an incorrect conclusion. We invite all users to submit discrepant results for our own analysis with the aim of modifying the program if necessary. Currently, the program is configured using the 2002 standards. Our aim is to regularly revise the program to reflect changes brought about by the ASIA updates.
Conclusion
The neurological classification of spinal cord injury can be challenging. The ISNCSCI provide a scheme that determines the severity and level of normal sensory and motor functioning. The rules that guide the determination of these values are somewhat complex and may be subject to interpretation errors resulting in inconsistencies in patient evaluation. Fewer errors are anticipated with the development of a computer program capable of interpreting the ISNCSCI. The potential to provide the program through the Internet would facilitate uniformity in the neurological classification of spinal cord injury. It will also be useful in providing residents, medical students and other health-care professionals with the ability to learn how to classify a person with spinal cord injury and check their answers while in training.
An additional benefit of this program is that if future revisions to the ISNCSCI occur, the algorithm can also be modified. Currently the program can only classify one person at a time and does not store results. Future considerations would see the algorithm input data from a database and export output to a database for incorporation in research studies.
The value of good clinical examination technique cannot be understated as this program is not a substitute for human interface at the bedside.
References
Guttmann L, Michaelis LS . Proceedings of the annual scientific meeting of the International Medical Society of Paraplegia, 28–30 July 1969, held at Stoke Mandeville Hospital, Aylesbury. Paraplegia 1970; 8: 67–69.
American Spinal Injury Association. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, IL, 1994.
Walker MD . Acute spinal cord injury. N Engl J Med 1991; 324: 1885–1888.
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury, revised 2002. American Spinal Injury Association: Chicago, IL, 2002.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. ASIA Neurological Standards Committee 2002. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Burns SP . Reliability and validity of the international standards of classification of spinal cord injury. In: Marino RJ (ed). Reference Manual for the International Standards for Neurological Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, IL, 2003.
A 30-day trial version of Adobe Flash can be downloaded from Adobe's website: http://www.adobe.com/products/flash/flashpro/.
Adobe Flash Player Version Penetration http://www.adobe.com/products/player_census/flashplayer/version_penetration.html.
Adobe Flash Player can be downloaded free of charge from Adobe's website: http://www.adobe.com/products/flashplayer/.
Acknowledgements
The authors thank Frank Bulk and Gabriel Ng, Division of Media and Technology, University of Saskatchewan, for facilitating the development of this program. Special thanks to Dr Brad Selk for his assistance with placing the program on the Internet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linassi, G., Li Pi Shan, R. & Marino, R. A web-based computer program to determine the ASIA impairment classification. Spinal Cord 48, 100–104 (2010). https://doi.org/10.1038/sc.2009.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.98
Keywords
This article is cited by
-
Computer International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) algorithms: a review
Spinal Cord (2023)
-
Achieving assessor accuracy on the International Standards for Neurological Classification of Spinal Cord Injury
Spinal Cord (2017)
-
Development and validation of a computerized algorithm for International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)
Spinal Cord (2016)
-
Feasibility of using training cases from International Spinal Cord Injury Core Data Set for testing of International Standards for Neurological Classification of Spinal Cord Injury items
Spinal Cord (2014)
-
Accuracy of physical examination for chronic lumbar radiculopathy
BMC Musculoskeletal Disorders (2013)