Abstract
Study design:
Case report.
Objectives:
To report an unusual case of neuro-Behcet's disease (NBD) presenting with isolated myelitis that affected the lumbar cord.
Setting:
Department of Neurology, West China Hospital, Chengdu, Sichuan, China.
Methods:
A 19-year-old man presented with a 3-day history of paresthesia and weakness in both the legs. He had a 6-year history of recurrent oral and genital ulcers with erythema nodosum on his legs. Magnetic resonance imaging (MRI) revealed a T1-hypointense and T2-hyperintense lesion at the L1 level. Nodular enhancement of the lesion was achieved with gadolinium administration. Biopsy specimens from cutaneous lesions were consistent with an active perivasculitic process.
Results:
Corticosteroid (pulsed methylprednisolone followed by oral prednisolone) therapy was administered immediately. Subsequently, the patient's clinical condition improved dramatically. The spinal cord lesion disappeared on the MRI performed 1 year later. Thus far, there has been no recurrence.
Conclusion:
NBD may involve the lumbar spinal cord. Prompt recognition of this disease and early vigorous steroid therapy are important to prevent further disability and recurrence.
Similar content being viewed by others
Introduction
Behcet's disease (BD) is a multisystem recurrent inflammatory disorder. Neurological involvement is a relatively rare manifestation of BD. Isolated myelitis has been reported in only a few cases of BD, and lesions were almost located in the cervical or thoracic cord.1, 2 We report a patient with myelitis presented with lumbar spinal cord involvement in the setting of BD.
Case report
A 19-year-old man was admitted because of a 3-day history of paresthesia and disabling weakness in both the legs. Since the age of 13 years he had recurrent oral and genital ulcers with the development of erythema nodosum on his legs. He had suffered from dysuresia and dyschesia for 10 days. He had experienced an acute numbness and absence of temperature sensation in the right lower extremity 3 days ago. Two days before admission, an unsteady gait and weakness in both his legs were noticed.
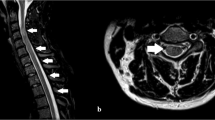
On physical examination, we noticed multiple red tubercles on his lingual root. Erythema nodosum like dark red, painful lesions were noticed on his legs. His scrotum showed ulceration. Ophthalmological examination revealed no sign of uveitis. He was alert, his cranial nerves and cerebellar functions were normal. According to the Medical Research Council grade, his muscle strength was 0/5 at both proximal lower extremities, 1/5 at the distal left lower limb, and 2/5 at the distal right lower limb. Cremasteric reflex and right knee jerk reflex were absent. Pain and temperature sensation reduced below the level of L4. Position sense was absent in the right distal leg. On admission, blood tests were normal except for increased erythrocyte-sedimentation rate (59 mm h−1) and C-reactive protein level (125 mg l−1). Cerebrospinal fluid analysis revealed pleocytosis (contained 50 × 106 l−1 white cells), with normal protein and glucose levels. The IgG index was normal and oligoclonal bands were absent. Visual evoked potentials and electromyogram were normal. Biopsy specimens of the erythema nodosum showed inflammatory cell infiltration in the perivascular areas (Figure 1). This histopathological result is consistent with the manifestation of perivasculitis. A diagnosis of neuro-Behcet's disease was suspected.
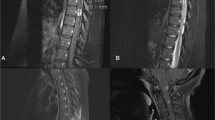
Results on cranial magnetic resonance imaging (MRI) were normal. Spinal MRI revealed abnormal signal at the L1 level. The lesion was hypointense on T1-weighted images but hyperintense on T2-weighted images, with nodular enhancement after gadolinium injection (Figures 2a and b). These signal abnormalities were indicative of an inflammatory change.
A 5-day pulse methylprednisolone therapy of 1 g d−1 was initiated. After high-dose methylprednisolone therapy, we administered oral prednisolone (60 mg d−1) to the patient and the dosage was decreased gradually. Thalidomide (200 mg d−1) was also administered to improve the mucocutaneous symptoms. After 18 days, the patient regained normal motor power with mild sensory deficits. Sphincter dysfunction and mucocutaneous lesions improved evidently. Spinal MRI performed 1 year later revealed that the lumbar cord lesion had completely resolved. Thus far, there has been no relapse.
Discussion
Neurological involvement in BD was first reported in 1941 by Knapp, and the term neuro-Behcet's disease (NBD) was introduced by Cavara and D'Ermo in 1954.3 The prevalence of spinal cord involvement in NBD patients ranges from 2.5 to 30%, and a predilection for cervical and thoracic involvements has been widely noted.1, 2 A case of NBD presenting as transverse myelitis from T9 to the conus after local spinal needle puncture was reported by Deshpande et al.,4 but the puncture procedure may have been the reason for the induced pathergy of spinal cord and might have caused the neurological involvement.
Our patient had no predisposing factor and fulfilled the clinical criteria for BD.5 Spinal cord MRI revealed a lesion in the lumbar cord, whereas cerebral MRI showed no abnormality. To our knowledge, this is the first report of an NBD case presenting with lumbar spinal cord involvement without other predisposing factors.
In our case, perivascular infiltration was confirmed via a cutaneous biopsy. However, pathological mechanism underlying spinal cord involvement in NBD cases has not been confirmed thus far.2 We administered corticosteroids to our patient to reduce inflammation and prevent relapse, and the outcome was fairly good. We think that edema and reversible inflammatory damage are the most likely abnormalities that caused the lumbar cord lesion.
Conclusion
This study indicates that NBD may involve the lumbar spinal cord. NBD should be considered as an etiological factor for myelitis, especially when the patient has a classical triad of oral and genital ulcerations with uveitis. In addition, in the light of the evidence of poor prognosis in patients with BD and spinal cord involvement, we suggest an early vigorous steroid therapy upon recognition of such patients.
References
Moskau S, Urbach H, Hartmann A, Schmidt S . Multifocal myelitis in Behcet's disease. Neurology 2003; 60: 517.
Yesilot N, Mutlu M, Gungor O, Baykal B, Serdaroglu P, Akman-Demir G . Clinical characteristics and course of spinal cord involvement in Behcet's disease. Eur J Neurol 2007; 14: 729–737.
Cavara V, D'Ermo F . A case of neuro-Behcet's syndrome. Acta XVIII Concillum Ophthal 1954; 3: 1489–1505.
Deshpande DM, Krishnan C, Kerr DA . Transverse myelitis after lumbar steroid injection in a patient with Behcet's disease. Spinal Cord 2005; 43: 735–737.
The International Study Group for Behcet's Disease. Evaluation of diagnostic (‘classification’) criteria in Behcet's disease—towards internationally agreed criteria. Br J Rheumatol 1992; 31: 299–308.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhao, B., He, L. & Lai, XH. A case of neuro-Behcet's disease presenting with lumbar spinal cord involvement. Spinal Cord 48, 172–173 (2010). https://doi.org/10.1038/sc.2009.124
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.124