Abstract
Study design:
Retrospective chart review.
Objective
To report six patients with isolated longitudinal myelitis (LM).
Setting:
Outpatients at Multiple Sclerosis Center/Clinic Vanderbilt University Medical Center.
Methods:1. Patients:
Patients treated for LM in whom evidence for multiple sclerosis (MS), neuromyelitis optica (NMO) and systemic inflammatory disorders such as systemic lupus erythematosus (SLE) was lacking. 2. Interventions: Clinical, laboratory and imaging data, treatment and outcomes were reviewed. 3. Main Outcome Measures: LM in the absence of optic neuritis, normal or nonspecific brain magnetic resonance imaging (MRI) findings, the absence of NMO antibody.
Results:
All presented with monophasic myelitis with variable loss of motor, sensory and bowel/bladder functions. MRIs of the brain were normal (five cases), and in the sixth showed a single T2 hyperintense lesion, which was interpreted as an ischemic lesion due to small-vessel disease. MRIs of the spinal cord of all patients showed swelling and T2 hyperintense lesions with patchy contrast enhancement that extended from the cervicomedullary junction to the conus medullaris. Two of these patients received rituximab with clinical benefit. Another patient received one dose of rituximab, developed an allergic reaction, received further treatments with azathioprine and also made a good recovery. In one patient, approval for rituximab was obtained several months after the inflammation had subsided, and she has shown only a minimal improvement. The two patients who did not receive rituximab made no significant recovery from their maximal neurological deficits.
Conclusions:
Isolated LM may be a new clinical syndrome, or a variant of NMO.
Similar content being viewed by others
Introduction
Transverse myelitis is an acute or subacute inflammatory disorder of the spinal cord, from diverse causes, resulting in loss or impairment of motor, sensory and autonomic disturbances below the level of the lesion.1 Recently, the term ‘longitudinally extensive transverse myelitis’ has been proposed to refer to myelitis with the involvement of more than three vertebral levels in the spinal cord, as is commonly seen with NMO.2 LM, with extensive contiguous involvement of the spinal cord, is rare and is described in the literature almost exclusively in the context of SLE.3, 4, 5, 6, 7 We describe six cases of isolated monophasic (follow-up 9 months to 4 years) LM, involving the entire length of the spinal cord.
Methods
Case records of patients treated for myelitis at the Vanderbilt Multiple Sclerosis Center were reviewed. Of the 339 patients who had been treated for myelitis since 2005, the vast majority had transverse myelitis secondary to either MS or NMO. These, and patients with another diagnosis, such as systemic inflammatory disorder or neurosarcoidosis, were excluded from review. Six patients who had LM not attributable to other diagnoses were reviewed in detail.
Results
Clinical presentation
All six patients presented with acute or subacute progressive loss of motor, sensory and bladder and bowel functions (Table 1). None of the patients had cognitive or visual problems, or symptoms referable to brainstem dysfunction. None had a history of antecedent infections. None of the patients had features of systemic inflammatory autoimmune diseases. Neurological examinations at the time of maximum deficits are shown in Table 1. Mental function, vision, cranial nerve examinations and ocular funduscopy were normal in all patients.
Imaging and evoked potentials
Magnetic resonance imaging (MRI) of the brain and spinal cord was performed on presentation in all patients and consisted of T1, T2, T2-FLAIR and T1 post-contrast sequences. Brain MRIs were normal in five patients and showed a solitary white matter lesion, possibly ischemic in one (patient 4). Spinal cord MRIs in all patients showed swelling and patchy T2 hyperintense lesions, extending from the cervicomedullary junction to the conus medullaris, with foci of T1 contrast enhancement (Figure 1). In patient 1, there was diffuse thickening of the spinal cord, raising concerns for an infiltrative tumor (Figure 2), but biopsy showed only inflammation. Visual evoked potential studies were available in four patients (1,2,4,6), and in patients 2 and 4, showed unilateral prolongation of P100.
Spinal cord magnetic resonance imaging (MRI) in longitudinal myelitis (patient 2). Sagittal T2-weighted images of cervical and upper thoracic (a), thoracic (d) and lumbar (g) demonstrate a contiguous T2 hyperintense lesion extending from C1 to the conus medullaris. Sagittal T1 pre-contrast (b, e and h) and T1 post-contrast (c, f and i ) images of these regions of spinal cord show swelling and foci of contrast enhancement (arrows).
Spinal cord magnetic resonance imaging (MRI) in longitudinal myelitis (patient 1). (a) Sagittal T2-weighted image of thoracic spinal cord demonstrates a contiguous T2 hyperintense lesion extending down to the conus medullaris. (b) Pre-contrast and (c) post-contrast sagittal T1-weighted images of thoracic spinal cord demonstrate diffuse thickening and contrast enhancement of the thoracic spine down to the conus medullaris.
Laboratory studies
Cerebrospinal fluid studies (Table 2) in all patients reflected a sterile inflammatory response within the central nervous system. Routine bacterial and viral cultures and PCRs (herpes simplex virus types 1 and 2, cytomegalovirus, varicella-zoster virus) were negative. Oligoclonal bands were absent in all patients except patient 5, who also had an elevated IgG index of 2.13. Other laboratory studies are shown in Table 2.
Treatment and outcomes
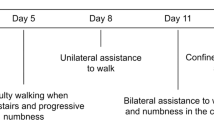
All patients received high-dose intravenous methylprednisolone, 1 g daily for 5–7 days, followed in patients 2, 3, 4 and 6 by plasma exchange (Table 1). Patients 4, 5 and 6 received rituximab at a dose of 375 mg m−2. Patient 4 developed an allergic reaction (skin rash) and received no further doses. Her lower extremity strength improved from BMRC scale 0/5–4/5, and after 5 months, she is ambulatory with the help of a cane. The others received additional doses at 3-month intervals (Table 1). Patient 6 received six doses of rituximab over 18 months, along with mycophenolate mofetil at a dose of 2000 mg daily, followed by mycophenolate mofetil alone. After a further 12 months, he has normal strength in all extremities, but uses a cane for walking because of persistent proprioceptive loss in the lower extremities. Patient 5, who was started on rituximab several months after the onset of her symptoms but whose symptoms were still evolving, has received three doses of rituximab so far. She recovered from being wheelchair-confined to being ambulatory with the help of a cane. In patient 3, rituximab was started after several months during which she received rehabilitation and mycophenolate mofetil 2000 mg daily, when there were no signs of further evolution of symptoms. She made only a minimal motor recovery. She has had a return of sensation in the lower extremities. Patients 1 and 2, who did not receive rituximab, made no appreciable recovery from their maximum disability (Table 1).
MRI of the spinal cord after treatment was available in all patients except patient 4, who was the most recently diagnosed and has not yet had a follow-up scan. There was resolution of swelling and contrast enhancement, with residual areas of T2 hyperintensities, and variable atrophy in all patients. Figure 3 shows serial MRIs of patient 6, at presentation, 8 and 20 months later.
Spinal cord MRIs before and after treatment (patient 6). (a–d) The cervical and thoracolumbar spinal cord at presentation; (e–h) 8 months later and (i–l) 20 months later. Initial MRIs show extensive T2 hyperintense signal and swelling of the entire spinal cord (a and c) with extensive contrast enhancement (b and d). In the second set of MRIs, the corresponding sequences show lower T2 abnormality and contrast enhancement, and resolution of the swelling. The third set of MRIs show the absence of contrast enhancement (j and l) and atrophy of spinal cord with patchy T2 hyperintense abnormality (i and k).
Discussion
The six cases of LM had a varied presentation (Table 1). The features common to all cases included a monophasic course, lack of visual symptoms suggestive of NMO, lack of inflammatory brain lesions and absent laboratory or clinical evidence of systemic inflammatory autoimmune diseases.
Several cases of longitudinal myelitis have been described in the literature, all in the context of SLE except for one case with Sjogren's syndrome.8 Extensive workup in our series could not point to a specific cause for the myelitis. Isolated longitudinal myelitis may therefore represent a new clinical syndrome. NMO, however, cannot be fully excluded, although longitudinally extensive transverse myelitis seen in NMO usually involves three to four segments of the spinal cord, rather than the entire cord.2 Because of the reported efficacy of B-cell depletion therapy in NMO, we decided to treat our patients using rituximab.9, 10, 11 Rituximab use appeared to facilitate recovery. Insurance authorization could not be obtained in patients 1 and 2, and they appeared to have made no appreciable recovery. There was a delay of several months in patient 3, and she too made a minimal recovery. The remaining patients received rituximab when their symptoms were still evolving, and they showed recovery. The response to rituximab may indicate that the inflammation in LM is mediated by a B-lymphocyte-mediated process, similar to that seen in NMO,12 but may also reflect SLE or another process mediated by B cells. NMO also cannot be fully excluded, as the positivity of the NMO antibody is only present in 12.5% of patients with the monophasic variant of NMO.13 Finally, given the short follow-up period in these patients (9 months to 4 years), it is possible that they may experience recurrent episodes of myelitis, or optic neuritis, in the future.
References
Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology 2002; 59: 499–505.
Weinshenker BG, Wingerchuk DM, Vukusic S, Linbo L, Pittock SJ, Lucchinetti CF et al. Neuromyelitis optica IgG predicts relapse after longitudinally extensive transverse myelitis. Ann Neurol 2006; 59: 566–569.
Deodhar AA, Hochenedel T, Bennett RM . Longitudinal involvement of the spinal cord in a patient with lupus related transverse myelitis. J Rheumatol 1999; 26: 446–449.
Tellez-Zenteno JF, Remes-Troche JM, Negrete-Pulido RO, Davila-Maldonado L . Longitudinal myelitis associated with systemic lupus erythematosus: clinical features and magnetic resonance imaging of six cases. Lupus 2001; 10: 851–856.
Lehnhardt FG, Impekoven P, Rubbert A, Burghaus L, Neveling M, Heiss WD et al. Recurrent longitudinal myelitis as primary manifestation of SLE. Neurology 2004; 63: 1976.
Chen HC, Lai JH, Juan CJ, Kuo SY, Chen CH, Chang DM . Longitudinal myelitis as an initial manifestation of systemic lupus erythematosus. Am J Med Sci 2004; 327: 105–108.
Orzechowski NM, Michet Jr CJ . Longitudinal myelitis. Mayo Clin Proc 2008; 83: 350.
Heinlein AC, Gertner E . Marked inflammation in catastrophic longitudinal myelitis associated with systemic lupus erythematosus. Lupus 2007; 16: 823–826.
Doan T, Massarotti E . Rituximab. Drugs Today (Barc) 2005; 41: 785–797.
Matiello M, Jacob A, Wingerchuk DM, Weinshenker BG . Neuromyelitis optica. Curr Opin Neurol 2007; 20: 255–260.
Wingerchuk DM, Weinshenker BG . Neuromyelitis Optica. Curr Treat Options Neurol 2005; 7: 173–182.
Lucchinetti CF, Mandler RN, McGavern D, Bruck W, Gleich G, Ransohoff RM et al. A role for humoral mechanisms in the pathogenesis of Devic's neuromyelitis optica. Brain 2002; 125 (Part 7): 1450–1461.
Lennon VA, Wingerchuk DM, Kryzer TJ . A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet 2004; 364: 2106–2112.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pawate, S., Sriram, S. Isolated longitudinal myelitis: a report of six cases. Spinal Cord 47, 257–261 (2009). https://doi.org/10.1038/sc.2008.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.99
Keywords
This article is cited by
-
Idiopathic acute transverse myelitis: outcome and conversion to multiple sclerosis in a large series
BMC Neurology (2013)
-
Entmarkungserkrankungen
Der Nervenarzt (2010)