Abstract
Study design:
Cost-effectiveness analysis following international guidelines and taking the societal viewpoint.
Objectives:
To estimate the cost-effectiveness of transanal irrigation using a self-administered irrigation system when compared with conservative bowel management.
Setting:
A randomized clinical trial was conducted at five spinal centres situated in Denmark, Germany, Italy, United Kingdom and Sweden. Estimates of resources and unit costs were made for the German health care system.
Methods:
Efficacy outcomes were drawn from a randomized controlled trial conducted in 2003–2005. Adult spinal cord-injured patients with neurogenic bowel dysfunction were randomized to 10 weeks with either transanal irrigation using Peristeen Anal Irrigation or to conservative bowel management. Costs were calculated based on results from the clinical trial and on 24 interviews conducted in Germany. Unit costs were obtained from the Federal Statistical Office Germany and product list prices.
Results:
When comparing outcome measures at termination, transanal irrigation significantly reduced symptoms of neurogenic bowel dysfunction. Product-related costs were higher for transanal irrigation using the self-administered system; however, costs for a carer to help with bowel management and changes/washing due to leakage were lower. For transanal irrigation, costs associated with urinary tract infections and patient time spent were reduced. Thus, the total cost to society is lower when patients use transanal irrigation. The results were shown to be robust in the sensitivity analysis.
Conclusion:
Transanal irrigation using a self-administered system reduces symptoms of neurogenic bowel dysfunction and results in a lower total cost to society than conservative bowel management.
Sponsorship:
The study was supported by Coloplast A/S.
Similar content being viewed by others
Introduction
Bowel dysfunction caused by spinal cord injury has a major impact on the patient's quality of life because of constipation, fecal incontinence, the extended time spent on defecation and the social restrictions that bowel dysfunction imposes on the patient.1, 2 Neurogenic bowel dysfunction affects around 80% of all spinal cord injured patients to some degree,3 making it a condition affecting an estimated number of 250 000 in Europe and another 250 000 in the United States of America.4, 5
Current management of neurogenic bowel dysfunction is largely empirical with limited evidence base.6 An acceptable solution has been sought for each patient on an individual basis using combinations of digital stimulation, manual evacuation, laxatives and suppositories as well as adjusting activity level, fluid intake and diet.7, 8 Thus, the current economic burden of bowel management in spinal cord injured patients remains to be established.
Transanal irrigation is a procedure that has been used for thousands of years, and has only of late been introduced for managing neurogenic bowel dysfunction.9 A recent randomized controlled trial of transanal irrigation versus conservative bowel management showed that transanal irrigation was the most efficient health technology for improving constipation, fecal incontinence and symptom-related quality of life in adult spinal cord injury patients.10 The study used a new product that enables independent transanal irrigation for patients with limited dexterity, thus promoting their independence in addition to alleviating symptoms of neurogenic bowel dysfunction.
Assessing the cost-effectiveness of new interventions is of major importance in policy decisions. We estimated the cost-effectiveness of transanal irrigation using data from the clinical trial as well as reliable estimates of the use of relevant resources and of unit costs appropriate to the German health care system.
Materials and methods
Health economic analysis
The present study is a cost-effectiveness analysis of transanal irrigation using a self-administered irrigation system when compared with conservative bowel management. The analysis follows international guidelines for cost-effectiveness analyses and takes the societal viewpoint as recommended by health economists.11
Outcome measurement
The efficacy outcomes were drawn from a randomized controlled trial conducted in five European countries in 2003–2005.10 Adult spinal cord injured patients with neurogenic bowel dysfunction were randomized to 10 weeks with either transanal irrigation using Peristeen Anal Irrigation or 10 weeks with conservative bowel management.8 Inclusion criteria were: Aged 18 or above with a spinal cord injury at any level at least 3 months from injury and one or more of the following symptoms: spending half an hour or more attempting to defecate each or every other day, episodes of fecal incontinence once or more per month, symptoms of autonomic dysreflexia before or during defecation, abdominal discomfort before or during defecation. Patients were excluded if there was evidence of other bowel disease or neurological disease. A power calculation estimated the effect size of the study to be 80 patients.
Peristeen Anal Irrigation (Coloplast A/S, Humlebaek, Denmark) is an integrated irrigation system consisting of a coated rectal balloon catheter, a control unit with a manual pump and a water container. The system is specially designed to enable self-administered transanal irrigation for immobilized patients and patients with poor dexterity. Conservative bowel management was defined as ‘best supportive bowel care without irrigation’ and followed the guidelines published by the Spinal Cord Medicine Consortium.8 A specialist nurse carried out training of patients in transanal irrigation or reeducation in conservative bowel management in hospital or on an outpatient basis. Patients were encouraged to contact the specialist nurse for advice, especially at the initiation of training.
The design and methods used for measuring efficacy outcomes is fully described elsewhere.10 A summary of baseline characteristics is presented in Table 1.
Outcome variables for efficacy were measured at baseline and after 10 weeks of treatment. The primary end points of the study were the St Mark's fecal incontinence score12 and the Cleveland Clinic constipation scoring system.13 The neurogenic bowel dysfunction score, which is a symptom-based score developed specifically for spinal cord-injured patients and takes into account the symptoms’ impact on quality of life14 was added as a secondary end point data was analysed by intention-to-treat using baseline values for missing outcome values at 10 weeks, thus assuming no effect of treatment and giving a conservative estimate of effect.
Cost measurement
Costs were calculated based on data collected in the randomized clinical trial used for outcome measurement,10 and the data was supplemented with information about carer time spent on different procedures. This was obtained in 24 structured interviews with nurses conducted in seven German rehabilitation centres from January to March 2007. Unit costs were obtained from the Federal Statistical Office Germany (2007) and product list prices (2007). The cost of products for transanal irrigation also includes the cost of disposables. The costs have been calculated for a 2-day period, corresponding to the average time between bowel management procedures and the cost variables used are specified in Table 2.
Uncertainty
The robustness of the cost-effectiveness analysis was tested in a one-way analysis.11 We systematically varied key parameters one at a time to investigate the sensitivity of the overall result to changes in these variables. Furthermore, we investigated the sensitivity of the results when assumptions were made regarding adverse events.
Results
Efficacy outcome
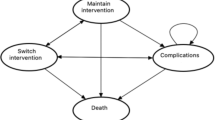
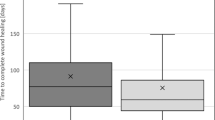
Of the 124 eligible patients, 87 patients were included and randomly assigned to the two treatment groups, 45 patients to conservative bowel management and 42 patients to transanal irrigation (Figure 1). The efficacy outcomes of the two bowel management methods are shown in Figure 2. When comparing outcome measures at termination, statistically significant results in favour of transanal irrigation were found for all three scoring systems. Conservative bowel management resulted in a slight improvement in fecal incontinence symptoms, whereas symptoms of constipation and neurogenic bowel dysfunction were slightly worse after 10 weeks. Transanal irrigation resulted in an improvement of symptoms for all three scoring systems.
Patient flow in clinical study reported by Christensen et al.10
Effect of the two bowel management methods. Mean scores for all patients are reported. For all three scoring systems, a higher score indicates more severe symptoms. Effects with negative values are improvements, that is, reductions in symptom severity. P-values are given for differences between groups at termination (student's t-test). Data from Christensen et al.10
Costs
The calculated costs for the two bowel management methods are presented in Table 3. Although product-related costs are higher for transanal irrigation using the self-administered system, costs for a carer to help with bowel management and changes/washing due to leakage are lower for transanal irrigation. Furthermore, costs associated with urinary tract infections are reduced when bowel management is transanal irrigation. Because patient time spent on bowel management is also reduced, the patient's indirect expenditure is lower for transanal irrigation. Thus, the total cost to society is lower when patients use transanal irrigation instead of conservative bowel management.
Sensitivity analysis
The three most decisive parameters for the overall result were carer time for bowel management, price of the system for transanal irrigation and the patient time spent on bowel management. By varying the average carer time spent on bowel management with transanal irrigation, the effect of this variable on the overall result was analysed. Carer time could be increased up to 26% before influencing the overall result. Furthermore the price of the system for self-administered transanal irrigation could be increased up to 12% without tipping the balance. Similarly, it was possible to increase patient time spent on bowel management with transanal irrigation with up to 10% before altering the result that transanal irrigation is cheaper than conservative bowel management from a societal perspective. In the clinical study,10 two patients managed with transanal irrigation were hospitalized because of severe abdominal pain caused by constipation. The sensitivity analysis showed that 2.5 events should occur before altering the overall result, under the assumption that the treatment consisted of two hospital days for disimpaction of constipated stool at a cost of 452 Euro per hospital day.
Discussion
The selection of an appropriate management method for neurogenic bowel dysfunction has only been based on clinical evidence to a limited extent, because of the lack of high quality studies comparing different management methods. The economic consequences of choosing a specific method have been even less studied.
This study aimed to investigate the cost-effectiveness of transanal irrigation using a self-administered system when compared with conservative bowel management using data from a randomized controlled trial. Transanal irrigation was more effective in reducing symptoms of constipation and fecal incontinence in spinal cord injured individuals. In addition, from a societal perspective transanal irrigation was cheaper than conservative bowel management. In economic terms, this is a dominant situation, where one management method is both cheaper and more effective than the alternative. The results obtained in this study were shown to be robust in the sensitivity analysis, where even relatively large changes to the parameters of time spent on bowel management and price of the irrigation system did not alter the overall conclusions of the cost analysis.
The economic analysis is limited by the fact that outcome measures were obtained from a study not specifically designed for the purpose of an economic analysis. We included both the primary and secondary outcomes from the study in our analysis because the data for all the parameters was collected systematically, and thus the number of observations minimized the risk of introducing large uncertainties to the calculations. By analogy, we chose not to include the observed adverse events because of the very limited number of observations. However, a sensitivity analysis including assumptions about occurrence of the adverse events observed in the clinical study10 showed that a 25% increase when compared with the clinical study was allowed before changing the outcome of the analysis.
Although the cost saving by using the self-administered transanal irrigation system for bowel management appears rather modest, the implications for society as a whole are more far-reaching when one considers a longer time frame and the number of patients who need a method to manage their neurogenic bowel dysfunction. With an assumption that 20% of patients who suffer from neurogenic bowel dysfunction could benefit from using transanal irrigation, the savings for society in Europe would be approximately 7.2 million Euros per year.
If one were to adopt a narrower health care perspective for the analysis, that is, look at cost-effectiveness from the payer's viewpoint, the patient's indirect expenditure would not be included in the sum of costs. Owing to higher costs for products, transanal irrigation would appear to be more expensive, and the relevant question is whether the extra health improvement obtained is worth the extra resources used. To make this ‘extrawelfarist’ assessment of cost-effectiveness correctly, however, the clinical study used for outcome measures has some limitations. Although validated scales have been used for measuring symptoms and quality of life, the scales are ordinal scales and cannot be translated directly into quality-adjusted life years, which are normally used in cost-effectiveness analyses to measure all health-related quality of life gains.
Nevertheless, the study shows a significant reduction in symptoms of constipation and fecal incontinence and it is well-documented that constipation and fecal incontinence are socially debilitating and that any improvement in these symptoms has a great impact on the patient's quality of life.15 Furthermore, the reduction of time spent on bowel management for the patients as well as their increased independence from carers also contribute to a higher quality of life for these patients. We therefore assume that the reported increase in quality of life for patients using transanal irrigation9, 10 would compensate for the increased product costs of the method and thus result in a higher cost-effectiveness for transanal irrigation. However, this would have to be confirmed in future studies.
Another limitation of this study is the short time perspective in terms of the outcome measurements. As a result, the costs have been calculated for a 2-day period, corresponding to the average time between bowel management procedures. If, on the other hand, the costs were calculated for a longer period of time, such as a year or a patient lifetime, the outcome measurements would also have to be done for longer than 10 weeks. This might in turn influence the overall result.
One scenario is that the long-term efficacy of transanal irrigation and the incidence of adverse events may differ from the ones reported here. However, transanal irrigation has been used for long-term management, and the success rate over time appears to stay high.16 Another scenario is that outcomes measured in this study may impact on other outcomes that are seen during the lifetime of a patient. An example could be urinary tract infections. The randomized trial comparing transanal irrigation to conservative bowel management showed a lower incidence of urinary tract infections for patients using transanal irrigation.10 In the long-term this might save patients from the more serious complications of urinary tract infections that occur in the spinal cord injured population,17 and thus result in additional health care cost savings by saving hospital days and treatment expenses.
Other benefits of transanal irrigation are much harder to value. In this study, we have taken into account the gained working days for patients by less time spent on bowel management procedures. However, we have not investigated how the lifted social restrictions and increased self-esteem and independence may actually be the crucial factor that enables a person to hold a job. What this means to the individual is practically impossible to put a price on.
Conclusion
This cost-effectiveness study of transanal irrigation when compared with conservative bowel management showed that transanal irrigation using a self-administered system reduces symptoms of neurogenic bowel dysfunction. Product-related costs were higher for transanal irrigation; however, costs of carer help, cost for treatment of urinary tract infections and loss of patient productivity were lower for transanal irrigation. This results in a lower total cost to society for transanal irrigation using a self-administered system. Thus, transanal irrigation is both cheaper and more effective than conservative bowel management.
References
Glickman S, Kamm MA . Bowel dysfunction in spinal-cord-injury patients. Lancet 1996; 347: 1651–1653.
Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA . Bowel dysfunction following spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord 2000; 38: 717–723.
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Ergas Z . Spinal cord injury in the United States: a statistical update. Cent Nerv Syst Trauma 1985; 2: 19–32.
Coggrave M, Wiesel PH, Norton C . Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev 2006, CD002115.
Haas U, Geng V, Evers GC, Knecht H . Bowel management in patients with spinal cord injury—a multicentre study of the German speaking society of paraplegia (DMGP). Spinal Cord 2005; 43: 724–730.
Clinical practice guidelines: neurogenic bowel management in adults with spinal cord injury. Spinal Cord Medicine Consortium. J Spinal Cord Med 1998; 21: 248–293.
Christensen P, Kvitzau B, Krogh K, Buntzen S, Laurberg S . Neurogenic colorectal dysfunction—use of new antegrade and retrograde colonic wash-out methods. Spinal Cord 2000; 38: 255–261.
Christensen P, Bazzocchi G, Coggrave M, Abel R, Hultling C, Krogh K et al. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology 2006; 131: 738–747.
Drummond MF, Jefferson TO . Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996; 313: 275–283.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA . Prospective comparison of faecal incontinence grading systems. Gut 1999; 44: 77–80.
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD . A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 1996; 39: 681–685.
Krogh K, Christensen P, Sabroe S, Laurberg S . Neurogenic bowel dysfunction score. Spinal Cord 2006; 44: 625–631.
Ng C, Prott G, Rutkowski S, Li Y, Hansen R, Kellow J et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis Colon Rectum 2005; 48: 1562–1568.
Christensen P, Krogh K, Buntzen S, Payandeh F, Laurberg S . Long-term outcome and safety of transanal irrigation for constipation and fecal incontinence. Dis Colon Rectum 2007 (accepted for publication).
Stover SL, Lloyd LK, Waites KB, Jackson AB . Urinary tract infection in spinal cord injury. Arch Phys Med Rehabil 1989; 70: 47–54.
Acknowledgements
We thank Dagnia Looms, PhD, for writing and editorial assistance with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christensen, P., Andreasen, J. & Ehlers, L. Cost-effectiveness of transanal irrigation versus conservative bowel management for spinal cord injury patients. Spinal Cord 47, 138–143 (2009). https://doi.org/10.1038/sc.2008.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.98
Keywords
This article is cited by
-
Contemporary management considerations of urinary tract infections for women with spina bifida
International Urogynecology Journal (2022)
-
Peristeen Transanal Irrigation System to Manage Bowel Dysfunction: A NICE Medical Technology Guidance
Applied Health Economics and Health Policy (2019)
-
Neurogenic Bowel Dysfunction in Patients with Neurogenic Bladder
Current Bladder Dysfunction Reports (2016)
-
Bowel Dysfunction in Spinal Cord Injury: Current Perspectives
Cell Biochemistry and Biophysics (2014)
-
Application of transanal irrigation for patients with spinal cord injury in South Korea: a 6-month follow-up study
Spinal Cord (2013)