Abstract
Study design:
Cross-sectional study.
Objective:
To study the manifestation of spasticity in daily life of the patients with spinal cord injury, their perception of spasticity and spasticity-related discomfort.
Setting:
Rehabilitation center in the Netherlands.
Methods:
Twenty-six patients with motor complete spinal cord injury (SCI) and spasticity in the lower limbs completed a questionnaire. The following outcome measures were used: manifestation of spasticity, activities during which spasticity occurs, perceived degree of spasticity and resulting discomfort, measured with visual analog scale (VAS) and Borg scale, respectively.
Results:
In general, spasticity manifested as extensor spasms (84.6%), flexor spasms and/or clonus (both 69.2%), and less often as continuous tension (57.7%). The registered activities were categorized into five main groups: ‘changing position’ was the largest group (22.0%) with a median VAS of 6.8 (range: 2.5–9.5) and median Borg scale of 3.0 (range: 1.0–7.0). Other groups of activities were ‘making a transfer’ (20.7%), ‘activities of daily living’ (17.1%), ‘being active’ (17.1%) and ‘stable body position’ (12.2%). The overall correlation between VAS and Borg was moderate (Spearman's rho=0.53, P=0.005).
Conclusions:
Patients with complete SCI experienced several manifestations of spasticity, extensor spasms being the most common. Many daily life activities elicited different manifestations of spasticity. The experienced discomfort was only moderately related to the perceived degree of spasticity during an activity. Possibly, the discomfort is influenced by other factors than the perceived spasticity alone.
Similar content being viewed by others
Introduction
Spasticity is commonly described as a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes, resulting from hyperexcitability of the stretch reflex.1 For patients with spinal cord injury (SCI), however, this definition can be considered too narrow, as spasticity and other positive signs of the upper motor neuron syndrome are sometimes hard to differentiate in clinical practice. For that reason, different broader definitions are used increasingly.2, 3, 4 In this study, a definition introduced by the SPASM consortium5 is used. The definition describes spasticity as disordered sensorimotor control, presenting as involuntary muscle activation following an upper motor neuron lesion, thus it includes all positive features of upper motor neuron syndrome.
Patients with SCI have a high probability to develop spasticity.3 Of all SCI patients, 25–43% reported problematic spasticity that hindered their daily activities.3, 4, 6, 7 Although some beneficial effects of spasticity have been reported,3, 4, 8 it is more often associated with secondary negative consequences like pain, fatigue and deformities,3 and its overall impact on daily life seems to be negative.9 A decision to treat spasticity depends largely on whether or not it interferes with patient's daily life. In patients with SCI, it has not been identified when spasticity mostly presents. However, this information is essential to improve our understanding of the impact of spasticity on their daily life.
Treatment of spasticity requires reliable assessment methods, which allow therapy to be individually optimized. To be able to assess whether ‘we are treating what we want to treat’, we need objective measurement methods that could measure spasticity in terms of body functions and structures within the framework of the International Classification of Functioning, Disability and Health (ICF).10 On the other hand, methods are needed that are closer to the patients’ perception, because in decision making for optimal treatment, patients’ perception plays an important role. The patients’ evaluation of spasticity is often an ad hoc report and is rarely documented by using measurement tools like the spasm frequency scale or a visual analog scale (VAS).11, 12, 13 Usually no differentiation is made between the perceived degree of spasticity and the experienced spasticity-related level of discomfort.
Figure 1 shows a proposed basic model, showing the interrelationship between the different components of the ICF framework and the perception of the patient.
Both the perception of spasticity and the experienced discomfort are influenced by personal and environmental factors, maybe in different proportions. It has been suggested that patients might include other physical sensations, such as pain, in their perception of spasticity.3, 8 Psychological factors, such as personal interpretations and coping strategies, will probably play a role as well.8 The experienced spasticity-related discomfort is expected to be influenced considerably by environmental factors, for example, the context in which spasticity occurs. It is recognized that a high degree of perceived spasticity does not necessarily imply high resulting discomfort,8, 9 although the relation between perceived spasticity and spasticity-related discomfort has not yet been explored. This knowledge could, however, provide important information for the interpretation of spasticity assessment and will, therefore, be essential in evaluating the effect of treatment.
In summary, this study aims to answer two questions. First, how and when does spasticity manifest in patients with motor complete SCI? Second, what is the relationship between the perceived degree of spasticity and the level of spasticity-related discomfort?
Materials and methods
This explorative cross-sectional study was performed by using a questionnaire that was developed for this study. Patients with motor complete SCI (American Spinal Injury Association) impairment scale14 grade A or B) were recruited from in- and outpatient departments of a rehabilitation center. The inclusion criteria were SCI at least 6 months old, stable medical condition and self-reported spasticity in the lower limbs. Patients signed informed consent before participation.
Questionnaire
The questionnaire consisted of three parts. The first part was a general section concerning sociodemographics and information on the date and level of injury and use of medication.
The second part focused on the individual perception and description of spasticity in the lower limbs. Four manifestations of spasticity were predefined in the questionnaire, of which patients could choose one or more when applicable: (a) a sensation of continuous tension or stiffness in one or both legs, (b) sudden bending of one or both legs (flexor spasms), (c) sudden straightening of one or both legs (extensor spasms) and/or (d) ‘shaking’ of the leg or the ankle (clonus). If necessary, patients could provide a description in their own words as well. Subsequently, questions were posed about whether spasticity was experienced as problematic, and if yes, how, and questions concerning the identification of factors influencing spasticity. These factors were prelisted, including the possibility to add others: (a) infection or inflammation, (b) (change of) posture, (c) full bladder or bowel, (d) skin problems, (e) time of the day, (f) emotions or mental stress, (g) tight clothing and (h) other.
In the final section, patients were asked to list a maximum of five activities during which they experience high degree of spasticity in the lower limbs. For each activity, patients were asked to rate the degree of spasticity as well as the level of spasticity-related discomfort they experienced. The perceived degree of spasticity was assessed using the VAS, a 10-cm line with ‘no spasticity’ and ‘most imaginable spasticity’ at the extremes. The VAS is a valid and reliable measure in rating pain intensity and is presently being used more often for the assessment of spasticity.11, 13 The level of spasticity-related discomfort was scored using the Borg scale. The Borg scale is a widely used scale for perceived exertion in exercise,15, 16 but is new in this field. In this study, a 12-point ratio scale was used with both numbers and verbal anchors,16 varying from ‘no discomfort at all’ (0) to ‘extremely much discomfort’ (10).
The questionnaires were completed in the presence of the investigator (JF or GV), so that instructions on how to fill out the questionnaire could easily be provided. Subjects without sufficient hand function were assisted in writing down their verbally given responses. For completing the VAS score, the investigator slowly moved a pencil from the left to the right extremity of the line. The mark was placed at the position indicated by the patient.
The questionnaire, in Dutch language, can be provided separately on request.
Analysis
Descriptive statistics were used to analyze the general characteristics of perceived spasticity. The activities with the highest VAS score per patient were grouped for an overall estimation of the relationship between perceived spasticity and spasticity-related discomfort. Subsequently, to facilitate interpretation each of the listed activities was allocated to one of six main groups. For each group, the reported characteristics of spasticity, as well as the medians and ranges of both VAS and Borg scores were mapped.
To assess the strength of association between the self-rated scores of VAS and Borg the non-parametric Spearman's rank correlation coefficient, with a significance level of 0.05, was used. To avoid bias due to paired observations, in case patients had written down more than one activity assigned to the same group, only the activity with the highest VAS score per patient was used for all calculations.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Sociodemographics
Twenty-six patients participated in the study. Each questionnaire took approximately 30–45 min to be completed.
Table 1 summarizes the baseline characteristics of the study population.
General characteristics of perceived spasticity
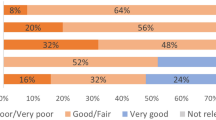
Fifteen patients (57.7%) described the spasticity in the legs as continuous tension. Flexor and extensor spasms were perceived by 69.2 and 84.6% of the patients, respectively. Eighteen subjects (69.2%) had clonus. Additionally, two patients described spasticity in different ways (slow contraction of muscles in toes and burning sensation, and slowly increasing tension).
More than half of the patients (57.7%) found the perceived spasticity problematic, mostly due to decreasing function (73.3%) rather than pain (33.3%). Other problems, such as annoyance, contractures and wounds, as a result of spasticity, were mentioned by six patients (23.1%).
In 20 patients (76.9%) the manifestation of spasticity was affected by infection or inflammation. Change of posture (92.3%), time of the day (53.8%), full bladder or bowel (50%), skin problems (42.3%), tight clothing (26.9%) and emotions or mental stress (23.1%) were also mentioned. Fifteen patients added other factors, of which temperature/climate (both coldness and heat), external stimuli (like riding on rough surface) and fatigue were the most frequently mentioned.
Activities with high degree of perceived spasticity
Altogether 82 activities were included. The registered activities were divided into six main groups (Table 2): ‘changing position’ was the largest group (22.0%). Other groups of activities were ‘making a transfer’ (20.7%), ‘activities of daily living’ (17.1%), ‘being active’ (17.1%) and ‘stable body position’ (12.2%). The ‘stable body position’ group included activities during which the patient remains in the same position for a long time. The remaining group consisted mainly of reactions on stimuli, and thus contained no specific activities (11.0%). This group was, therefore, left out of further analysis.
In Table 3, the types of manifestation per group of activities are presented.
Extensor spasms were the most commonly occurring manifestation in all groups except in the ‘stable body position’ group, where flexor spasms were the most common (87.5%).
Relationship between perceived spasticity and spasticity-related discomfort
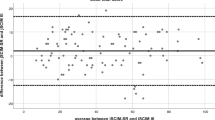
The (mixed) group of activities with the highest VAS score per patient had a median VAS of 7.6 (range: 2.5–9.5) and a median Borg of 6.0 (range: 0.0–10.0). The correlation between VAS and Borg scale was moderate (Spearman's rho=0.53, P<0.01).
The association between VAS and Borg scores was also calculated for all five groups of activities (see Table 4). For the groups 4 (‘being active’) and 5 (‘stable body position’), the correlation between the VAS and Borg score was marked (rho=0.71 and 0.78, respectively) and statistically significant (P=0.01 and 0.02). For group 3 (‘activities of daily living’), the correlation was moderate (rho=0.58) but statistically significant (P=0.046). For the other two groups, correlation was low and not significant.
Five patients mentioned positive effects of spasticity. Some described it as practical, for example, while getting dressed, especially when putting on trousers, or when stretching the trunk. Another subject experienced it as a pleasant feeling because an outburst of spasms relaxes the muscles afterwards. Prevention of muscle atrophy and prevention of skin sores were mentioned as well.
Several patients indicated that they had experienced high discomfort at the onset of the symptoms, but later they had got used to the spasticity and it was no longer regarded as problematic. One patient said that it had taken her time to learn how to interpret the new body signals. Another patient used to be ashamed of the spasticity shortly after his injury, but not anymore. Most patients had found ways to suppress spasms or clonus when they felt it coming up, for example, by pushing with hands or arms on the knees or by changing position.
Presence of high discomfort at the time of participation in this study was usually associated with the fear of falling (for example, out of the wheelchair, in the shower) or otherwise dangerous situations, such as driving.
Discussion
Spasticity is a multidimensional phenomenon, which seems to be looked upon in different ways by patients and clinicians. It is important to have insight in these different perceptions, especially when considering treatment to reduce spasticity, to be able to meet the patients’ needs. The aim of this study was to provide epidemiological data on the manifestation of spasticity in patients with motor complete SCI and to investigate how the perceived degree of spasticity and spasticity-related discomfort are associated.
A high degree of spasticity was most frequently perceived during ‘changing position’ and ‘making a transfer’. These two groups of activities partially overlap, as part of the perceived spasticity during transfers is possibly elicited by changing position. Other explanations for perceived spasticity during transfers are touching the skin, increasing abdominal pressure or great physical exertion. From clinical observations, it is known that extension of the hips can elicit spasms, particularly extensor spasms. Flexor spasms are usually seen after skin stimuli. Experimental observations have confirmed that proprioceptive stimuli from the hip are the most likely triggers for extensor spasms in patients with SCI.17, 18 The influence of knee joint rotation in provoking extensor spasms is also described.18 In addition to skin stimuli, imposed movements of the ankle or knee joint can also elicit flexor reflexes in SCI.19, 20
Perception of spasticity by ASIA-A subjects is hard to explain in neurological context. Spasms and clonus, causing limb movement, can obviously be perceived indirectly, for example, by vision. A possible consequence of continuous tension might be the increased difficulty in performing the activities.
A highly interesting finding in this study is the modest correlation between perceived spasticity and spasticity-related discomfort during activities as measured with the VAS and Borg scale, respectively. Correlation between the VAS and Borg scale is higher during activities involving a ‘stable body position’ and while ‘being active’. This finding confirms the idea that the impact of spasticity on daily life is related to the context in which it occurs. It would appear that in some situations, a high degree of spasticity is disturbing, whereas in other situations, the patient can adapt more easily. The experienced discomfort can be based on practical reasons, such as disturbance of sleep, compromised safety, and so on, or on psychological factors, such as coping strategies or negative self-image. The latter is supported by the indication that overall negative impact of spasticity seemed to decrease with time since injury, as was brought up by a number of patients in this study. This finding agrees with other observations.3, 7, 8 Perhaps the growing acceptance of their situation, better understanding of the altered body functions and/or finding ways how to deal with it, can explain the diminishing impact of spasticity on daily life of patients with SCI through the years. These observations imply that treatment of spasticity might serve different purposes for patients in different phases after injury, as ‘confounding’ of the patients’ perception seems to change throughout time. This information is of high clinical interest as it might improve communication between patients and clinicians. However, further research is needed to clarify the complexity of this process.
Conclusions
Patients with motor complete SCI experienced several manifestations of spasticity. Extensor spasms, mainly elicited by activities incorporating change of position, were most common.
Self-ratings on the perceived degree of spasticity by the patients should be added to the set of assessment methods for the evaluation of spasticity. It is useful to distinguish between the perceived degree of spasticity and experienced spasticity-related discomfort, because they were only moderately associated. How these self-rating scores relate to spasticity in terms of involuntary muscle activity, assessed with more objective tools, will be an interesting area for further research.
References
Lance JW . Symposium synopsis. In: Feldman RG, Young RR, Koella WP (eds). Spasticity: Disordered Motor Control. Chicago: Year Book 1980, pp 485–494.
Priebe MM, Sherwood AM, Thornby JI, Kharas NF, Markowski J . Clinical assessment of spasticity in spinal cord injury: a multidimensional problem. Arch Phys Med Rehabil 1996; 77: 713–716.
Sköld C, Levi R, Seiger A . Spasticity after traumatic spinal cord injury: nature, severity, and location. Arch Phys Med Rehabil 1999; 80: 1548–1557.
Adams MM, Hicks AL . Spasticity after spinal cord injury. Spinal Cord 2005; 43: 577–586.
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil 2005; 27: 2–6.
Levi R, Hultling C, Nash MS, Seiger A . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
Mahoney JS, Engebretson JC, Cook KF, Hart KA, Robinson-Whelen S, Sherwood AM . Spasticity experience domains in persons with spinal cord injury. Arch Phys Med Rehabil 2007; 88: 287–294.
Adams MM, Ginis KA, Hicks AL . The spinal cord injury spasticity evaluation tool: development and evaluation. Arch Phys Med Rehabil 2007; 88: 1185–1192.
Geneva World Health Organization. WHO: International Classification of Functioning, Disability and Health (ICF). World Health Organization: Geneva, 2001, Chapter 5.1, pp 18-19.
Sköld C . Spasticity in spinal cord injury: self- and clinically rated intrinsic fluctuations and intervention-induced changes. Arch Phys Med Rehabil 2000; 81: 144–149.
Platz T, Eickhof C, Nuyens G, Vuadens P . Clinical scales for the assessment of spasticity, associated phenomena, and function: a systematic review of the literature. Disabil Rehabil 2005; 27: 7–18.
Lechner HE, Frotzler A, Eser P . Relationship between self- and clinically rated spasticity in spinal cord injury. Arch Phys Med Rehabil 2006; 87: 15–19.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Borg G . Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health 1990; 16 (Suppl 1): 55–58.
Dawes HN, Barker KL, Cockburn J, Roach N, Scott O, Wade D . Borg's rating of perceived exertion scales: do the verbal anchors mean the same for different clinical groups? Arch Phys Med Rehabil 2005; 86: 912–916.
Little JW, Micklesen P, Umlauf R, Britell C . Lower extremity manifestations of spasticity in chronic spinal cord injury. Am J Phys Med Rehabil 1989; 68: 32–36.
Wu M, Hornby TG, Hilb J, Schmit BD . Extensor spasms triggered by imposed knee extension in chronic human spinal cord injury. Exp Brain Res 2005; 162: 239–249.
Schmit BD, McKenna-Cole A, Rymer WZ . Flexor reflexes in chronic spinal cord injury triggered by imposed ankle rotation. Muscle Nerve 2000; 23: 793–803.
Wu M, Hornby TG, Kahn JH, Schmit BD . Flexor reflex responses triggered by imposed knee extension in chronic human spinal cord injury. Exp Brain Res 2006; 168: 566–576.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fleuren, J., Voerman, G., Snoek, G. et al. Perception of lower limb spasticity in patients with spinal cord injury. Spinal Cord 47, 396–400 (2009). https://doi.org/10.1038/sc.2008.153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.153
Keywords
This article is cited by
-
Limb accelerations during sleep are related to measures of strength, sensation, and spasticity among individuals with spinal cord injury
Journal of NeuroEngineering and Rehabilitation (2022)
-
The experience of spasticity after spinal cord injury: perceived characteristics and impact on daily life
Spinal Cord (2018)
-
Treatment patterns of in-patient spasticity medication use after traumatic spinal cord injury: a prospective cohort study
Spinal Cord (2018)
-
Neuropathic Pain After Spinal Cord Injury: Challenges and Research Perspectives
Neurotherapeutics (2018)
-
Reliability of the Modified Ashworth Scale and Modified Tardieu Scale in patients with spinal cord injuries
Spinal Cord (2017)