Abstract
Study design:
International expert working group.
Objective:
To develop an International Bowel Function Extended Spinal Cord Injury (SCI) Data Set presenting a standardized format for the collection and reporting of an extended amount of information on bowel function.
Setting:
Working group consisting of members appointed by the American Spinal Injury Association (ASIA) and the International Spinal Cord Society (ISCoS).
Methods:
A draft prepared by the working group was reviewed by Executive Committee of the International SCI Standards and Data Sets and later by the ISCoS Scientific Committee and the ASIA Board. Relevant and interested scientific and professional organizations and societies (around 40) were also invited to review the data set and it was posted on the ISCoS and ASIA websites for 3 months to allow comments and suggestions. The ISCoS Scientific Committee, ISCoS Council and ASIA Board received the data set for final review and approval.
Results:
The International Bowel Function Basic SCI Data Set includes 26 items providing a thorough description of bowel-related symptoms as well as clinical assessment of anal sphincter function and description of total gastrointestinal or segmental colorectal transit times.
Conclusion:
An International Bowel Function Extended SCI Data Set has been developed. This Data Set is mainly for research purposes and it should be used in combination with the information obtained from the International SCI Core Data Set and the International Bowel Function Basic SCI Data Set.
Similar content being viewed by others
Introduction
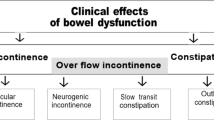
Neurogenic bowel dysfunction including constipation, fecal incontinence and abdominal pain or discomfort affects the majority of individuals with spinal cord injury (SCI).1, 2, 3, 4 Symptoms often restrict social activities and impair quality of life.2, 3 Colonic transit times are usually prolonged5, 6, 7, 8 and anorectal sensibility and voluntary control of the external anal sphincter is reduced or lost.5, 9, 10 The severity of colorectal and anal sphincter dysfunction depends on the completeness of SCI3 and constipation-related symptoms become significantly more severe with time since injury.1, 11
A Bowel Function Basic SCI Data Set (Krogh K et al., submitted) has been developed to facilitate comparison of symptoms and outcomes between patients, various centers and countries through the collection of data in a standardized manner. Furthermore, background information about age, gender, level of lesion and so on is collected within the International SCI Core Data Set.12
A Cochrane review concluded that the treatment of bowel dysfunction in patients with central neurological diseases must remain empirical until well-designed clinical trials have been performed.13 Such trials, as well as other studies on bowel function after SCI, may benefit from detailed collection of data in a standardized manner. In accordance with the aim and vision of the International Spinal Cord Injury Data Sets,14 the following International Bowel Function Extended SCI Data Set has been developed mainly for this purpose. Accordingly, information within the Bowel Function Extended SCI Data Set is mainly for research purposes and should be used in connection with information from the International SCI Core Data Set12 and the Bowel Function Basic SCI Data Set.
Methods
The development of the International Bowel Function Extended SCI Data Set by the working group appointed by the American Spinal Injury Association (ASIA) and the International Spinal Cord Society (ISCoS), together with a representative of the Executive Committee of the International Spinal Cord Injury Standards and Data Sets, followed the lines described for the International Bowel Function Basic SCI Data Set (Krogh K et al., submitted).
Results
The complete International Bowel Function Extended SCI Data form is included in the Appendix. The complete data syllabus, data sheet and training cases will be available at the respective websites of ISCoS (www.iscos.org.uk) and ASIA (www.asia-spinalinjury.org). The following items are included in the Data Set:
Date of data collection
As the collection of data on bowel function may be carried out at any time since SCI, the date of data collection is imperative to compute time since injury and to identify the data collected in relation to other data collected on the same individual at various time points (that is, in the International SCI Core Data Set).12
Duration of constipation
Functional constipation is usually defined according to the Rome II15 or Rome III16 criteria. Accordingly, within a specified period of time, individuals should report at least one of the following: straining >¼ of defecations, lumpy or hard stools >¼ of defecations, sensation of incomplete evacuation >¼ of defecations, sensation of anorectal obstruction/blockade >¼ of defecations, manual maneuvers to facilitate defecation >¼ defecations, or <3 defecations per week. The Rome criteria have not been specifically developed for individuals with SCI. However, in this data set, they are used to define the term constipation. In most individuals with SCI, the duration of constipation is equal to the time since SCI. However, constipation-related symptoms may become more severe with time after SCI and some individuals may develop constipation years later.11
Unsuccessful attempts at defecation
This variable documents the average number of daily unsuccessful attempts at defection within the last 3 months. Unsuccessful attempt at defecation is a common sign of obstructed defecation. To be considered as one attempt, the bowel emptying procedure should be separated from the previous bowel emptying procedure by some other activity.
Incomplete rectal emptying after defecation
This variable documents the presence of any sense of incomplete rectal emptying after defecation within the last 3 months. A sense of incomplete rectal emptying after defecation is a common sign of obstructed defecation.
Abdominal bloating
This variable documents the presence of abdominal bloating within the last 3 months. Abdominal bloating is a common symptom in chronic constipation and other motility disorders. In this data set, bloating is either a subjective feeling of excessive intra-abdominal gas or visible/palpable abdominal distension due to gas.
Abdominal pain/discomfort
This variable documents the presence of abdominal pain or discomfort within the last 3 months. Abdominal pain or discomfort is a common symptom not only in individuals with SCI4 but also in chronic constipation or irritable bowel syndrome and in the general population.17, 18 It should be documented separately from abdominal bloating and perianal symptoms covered by those specific variables. In some individuals, abdominal pain is an indirect signal of the need to defecate. In such cases, it is covered both by that specific variable in the Bowel Function Basic SCI Data Set and here. In subjects unable to feel abdominal pain, the term ‘Never’ should be used.
Respiratory discomfort due to a distended abdomen
This variable documents any respiratory discomfort (shortness of breath/difficulty in taking a deep breath) considered to be entirely or partly due to a distended abdomen. Constipation and bloating may cause or contribute to respiratory discomfort. This is defined as a feeling of shortness of breath or difficulty in taking a deep breath entirely or partly due to a distended abdomen. Accordingly, patients do not have to be able to clearly differentiate between bowel and other causes of respiratory discomfort. However, respiratory symptoms entirely due to higher level SCI are not included in this variable.
Perianal pain during defecation
This variable documents the presence of perianal pain during defecation within the last 3 months. Perianal pain during defecation is a common sign of difficult bowel evacuation. Most individuals with complete SCI are unable to feel perianal pain during defecation. In such cases, the code ‘Never’ and not the code ‘Unknown’ should be used. Indirect indicators of perianal pain during defecation such as perspiration, spasms or headache are not registered here.
Frequency of flatus incontinence
This variable documents the frequency of flatus incontinence within the last 3 months. Flatus incontinence is defined as involuntary passage of flatus.
Frequency of fecal incontinence to liquid stools
This variable documents frequency of fecal incontinence to liquid stools within the last 3 months. Fecal incontinence is defined as involuntary passage of stools. It has profound influence on quality of life and may cause severe restriction on social activities.3, 19
Frequency of fecal incontinence to solid stools
This variable documents frequency of fecal incontinence to solid stools within the last 3 months.
Ability to defer defecation for 15 min or more
This variable documents the ability to defer defecation for 15 min or more within the last 3 months. Inability to defer defecation may cause fecal incontinence and restrict social activities.
Position for bowel care
This variable documents the position for bowel care used within the last 3 months. The position for bowel care is important for bowel management. Whenever appropriate more than one code could be used for the same individual.
Degree of independence during bowel management
The degree of independence during bowel management is important to most individuals with SCI. The codes used are identical to those used in the Spinal Cord Independence Measure III (SCIM III).20
Bowel care facilitators
Individuals with SCI may use a number of maneuvers to facilitate bowel care. Digital anorectal stimulation is digital triggering of rectal contractions and anal relaxation and thus rectal emptying. Digital evacuation is the need to dig out stools with a finger. Although the effect is not much validated, abdominal massage is recommended by some to improve colorectal transit. The gastrocolonic response stimulates colorectal motility after the intake of a meal. It remains after SCI, and many individuals with SCI use this response by performing bowel care shortly after breakfast.
Events and intervals of defecation (1): Average time from the initiation of bowel care to first stool coming out
This variable is an attempt to describe the time spent at bowel care in more detail than just total time spent at defecation.21 The code given in minutes is based on each individual's own assessment of average time consumption.
Events and intervals of defecation (2): Average time during bowel movement when stool comes out
This variable begins when the previous variable stops and documents average time during bowel movement when stool intermittently or continuously (in the case of a single defecation) comes out with or without assistance. It is an attempt to describe the time spent at bowel care in more detail than just total time spent at defecation.21 The code given in minutes is based on each individual's own assessment of time consumption.
Events and intervals of defecation (3): Time spent waiting after last stool passes before ending bowel care
This variable begins when the previous variable ends. In line with the two previous items this variable is also an attempt to describe the time spent at bowel care in more detail. End of bowel care is defined as end of dressing. If this is not applicable, end of bowel care is end of clean up.
Lifestyle alteration due to anal incontinence
Anal incontinence covers fecal incontinence and flatus incontinence. This variable only covers altered lifestyle due to anal incontinence or the risk of anal incontinence. Examples may be avoidance of social activities, traveling, sexual activities and so on.
Lifestyle alteration due to constipation
This variable only covers altered lifestyle due to constipation. Constipation-related symptoms included difficult bowel evacuation. Examples may by avoidance of social activities, traveling and so on.
Self-reported impact on the quality of life caused by neurogenic bowel dysfunction
Self-reported impact on the quality of life caused by neurogenic bowel dysfunction covers the patient's own assessment of the impact of all aspects of neurogenic bowel dysfunction. This parameter is important for any choice of treatment modality.
Anal tone
Digital examination of anal tone mainly provides information about the anal resting pressure. Under normal circumstances, it is estimated that the internal anal sphincter muscle, consisting of smooth muscle cells, contributes to 55–85% of the anal resting pressure. The remaining is from the striated external anal sphincter muscle and the pressure within the hemorrhoidal plexus.22
Sympathetic innervation is believed to increase the tone of the external anal sphincter.23 Accordingly, anal resting pressure is generally lower in individuals with spinal cord lesions at or above the second lumbar vertebrae than in those with lower lesions.10 However, spasms of the striated external anal sphincter muscle may cause an excessively high pressure. The resting anal pressure is highly variable between individuals,24, 25 and the reproducibility and validity of digital anal examination of individuals with SCI remains to be tested. Accordingly, this variable depends on the subjective assessment of the examiner and only three options are given for this.
Evidence suggests that the amplitude of rectoanal inhibitory reflex mediating relaxation of the internal anal sphincter muscle during stretch of the rectal wall is affected by the level of SCI.10 Therefore, it is recommended that the tone of the anal canal is evaluated before and not after digital examination of the rectum is performed.
Voluntary contraction of the anal canal
Digital evaluation of voluntary contraction of the anal canal is an assessment of the voluntary function of the external anal sphincter muscle. The comments about intersubjective variation and validity of the examination given above are also true for this variable. Accordingly, it is only assessed whether there is voluntary contraction of the anal canal or not.
Voluntary anal contraction may be confused with spasms or reflex activity of the external anal sphincter muscle. Accordingly, it is recommended to ask the patient to contract the anal canal two times or more during the examination.
Total gastrointestinal or colonic transit time
This variable documents total gastrointestinal or colonic transit time assessed by means of radio-opaque markers and a plain abdominal X-ray. Total gastrointestinal and colonic transit times are prolonged in many individuals with SCI.5, 6, 7, 8 Transit time through the stomach and the small intestine is usually just a few hours. Colonic transit time is, however, much longer. Some authors present transit times as total gastrointestinal transit time and others prefer colonic transit time. Unless multiple X-rays are taken, the most correct term is total gastrointestinal transit time.
Generally, transit time is prolonged throughout the colon in individuals with supraconal SCI. In contrast, individuals with conal or cauda equina lesions often have severely prolonged rectosigmoid or left colonic transit times.8 The intrasubjective variation remains to be studied and due to poor correlations between total gastrointestinal/colonic transit time and colorectal symptoms after SCI, the clinical relevance of transit time measurement has been questioned.26 Several types of radio-opaque markers and protocols for determining total gastrointestinal and colonic transit times exist. However, no evidence exists to recommend one from the others.
Right colonic transit time
This variable documents transit time of the cecum, ascending and transverse colon assessed by means of radio-opaque markers. The comments given about total gastrointestinal or colonic transit time are applicable to this item too.
Left colonic transit time
This variable documents transit time of the descending colon (including the splenic flexure) and the rectosigmoid assessed by means of radio-opaque markers.
Discussion
The data within this International Bowel Function Extended SCI Data Set shall be seen in conjunction with data in the International SCI Core Data Set12 and the International Bowel Function Basic SCI Data Set. The International SCI Core Data Set includes information on date of birth and injury, gender, the cause of spinal cord lesion, and neurologic status among others. The Bowel Function Basic SCI Data Set was mainly developed for clinical use and the number of items included (n=12) was kept as small as possible. In contrast, the present International Bowel Function Extended SCI Data Set is mainly intended for research and should provide a standardized format for the collection and reporting of extended information on bowel function after SCI.14 However, the working group recognizes that information within the Bowel Data Sets could be extended by other clinically important information whenever appropriate. We are also aware that not all items in the Data Set will be relevant in all studies and researchers may choose to use only those relevant in a given setting.
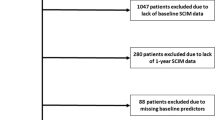
Several scores have been developed for fecal incontinence,27, 28 constipation19 or neurogenic bowel dysfunction29 but none have yet been generally accepted for use in individuals with SCI. The working group found it important to make results from studies using the SCI Bowel Data Sets as comparable as possible to results from other patient groups and we recognize that treatment of bowel dysfunction after SCI should be multidisciplinary. Therefore, the combined Basic and Extended Data Sets cover the most commonly used scores even if this means including a few items that could otherwise have been left out. This also explains why the time period used for some items is four weeks while it is 3 months in others.
The present International Bowel Function Extended SCI Data Set mainly includes colorectal symptoms. This reflects the paucity of validated objective measures for bowel dysfunction after SCI. However, the working group found that objective parameters should be included if valid and if available at most institutions. The most basic objective measure is anal tone and contraction force assessed by digital examination. To keep it as simple as possible, these two parameters are described as normal, reduced or excessive and present or not present. Anorectal sensibility is covered by the International SCI Core Data Set.12 Radiographically determined gastrointestinal or total and segmental colorectal transit times were included as objective parameters for colorectal function as they are easily performed. The correlation between transit times and symptoms is poor,26 and symptoms and objective measures should complement each other. We also considered including anorectal physiology tests but chose not to do so. This was mainly for the following two reasons: equipment for anorectal physiology testing is not available at most centers and variation in the parameters commonly used is extremely large.30
To facilitate the use of the International SCI Data Sets, this Bowel Function Extended Data Set and its data collection form (Appendix) have been developed much along the lines of the International Lower Urinary Tract Function Basic SCI Data Set.31
The International Bowel Function Basic and Extended SCI Data Sets were developed by a working group of experts with clinical and research experience within the field, and a large number of organizations and societies were asked for comments. The general outline of the Bowel Data Sets was accepted by almost all those giving their comments, and nearly all comments received were about specific details and clarification. However, the validity and reproducibility of most items included is unknown and the usefulness of the Bowel Data Sets needs to be shown. Much work is still needed to validate and translate these data sets, and the authors invite all interested to participate in this open and ongoing process.
References
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I . Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol 1990; 84: 1114–1119.
Glickmann S, Kamm MA . Bowel dysfunction in spinal cord injury patients. Lancet 1996; 347: 1651–1653.
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Finnerup NB, Faaborg P, Krogh K, Jensen TS . Abdominal pain in long-term spinal cord injury. Spinal Cord 2008; 46: 198–203.
Beuret-Blanquart F, Weber J, Gouverneur JP, Demangeon S, Denis P . Large bowel transit time and anorectal manometric abnormalities in 19 patients with complete transection of the spinal cord. J Auton Nerv Syst 1990; 25: 109–112.
Menardo G, Bausano G, Corazziari E, Fazio A, Marangi A, Genta V et al. Large bowel transit in paraplegic patients. Dis Colon Rectum 1987; 30: 924–928.
Nino-Murcia M, Stone J, Chang P, Perkash I . Colonic transit in spinal cord injured patients. Invest Radiol 1990; 25: 109–112.
Krogh K, Mosdal C, Laurberg S . Gastrointestinal and segmental colonic transit times in patients with acute and chronic spinal cord lesions. Spinal Cord 2000; 38: 615–621.
MacDonagh R, Sun WM, Thomas DG, Smallwood R, Read NW . Anorectal function in patients with complete supraconal spinal cord lesions. Gut 1992; 33: 1532–1538.
Krogh K, Mosdal C, Gregersen H, Laurberg S . Rectal wall properties in patients with acute and chronic spinal cord lesions. Dis Colon Rectum 2002; 45: 641–649.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K . The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2008; 46: 234–238.
DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stipling T et al. International Spinal Cord Injury Core Data Set. Spinal Cord 2006; 44: 535–540.
Wiesel PH, Norton C, Brazzelli M . Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev 2001; 4: CD002115.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T et al. International Spinal Cord Injury Data Sets. Spinal Cord 2006; 44: 530–534.
Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA . Functional bowel disorders and functional abdominal pain. Gut 1999; 45 (Suppl II): II43–II47.
Drossman DA . The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006; 130: 1377–1390.
Jones R, Lydeard S . Irritable bowel syndrome in the general population. Br Med J 1992; 304: 87–90.
Drossman DA, Sandler RS, McKee DC, Lovitz AJ . Bowel patterns among subjects not seeking health care. Gastroenerology 1982; 83: 529–534.
Agachan F, Chen T, Pfeiffer J, Reisman P, Wexner SD . A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 1996; 39: 681–685.
Catz A, Itzkovich M . Spinal Cord Independence Measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res Dev 2007; 44: 65–68.
House JG, Stiens SA . Pharmacologically initiated defecation for persons with spinal cord injury: effectiveness of three agents. Arch Phys Med Rehabil 1997; 78: 2062–2065.
Lestar B, Pennickx F, Kerremans R . The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis 1989; 4: 118–122.
Uher E-M, Swash M . Sacral reflexes: physiology and clinical application. Dis Colon Rectum 1998; 41: 1165–1177.
Pedersen IK, Christiansen J . A study on the physiological variation in anal manometry. Br J Surg 1989; 76: 69–70.
Rogers J, Laurberg S, Misiewiez JJ . Anorectal physiology validated: a repeatability study of the motor and sensory tests of anorectal function. Br J Surg 1989; 76: 607–609.
Leduc BE, Spacek E, Lepage Y . Colonic transit after spinal cord injury: any clinical significance. J Spinal Cord Med 2002; 25: 161–166.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA . Prospective comparison of faecal incontinence grading systems. Gut 1999; 44: 77–80.
Jorge JMN, Wexner SD . Etiology and management of faecal incontinence. Dis Colon Rectum 1993; 36: 77–97.
Krogh K, Christensen P, Sabroe S, Laurberg S . Neurogenic bowel dysfunction score. Spinal Cord 2006; 44: 625–631.
Madoff RD, Orrom WJ, Rothenberger DA, Goldberg SM . Rectal compliance: a critical reappraisal. Int J Colorectal Dis 1990; 5: 37–40.
Biering-Sørensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ . International lower urinary tract function basic spinal cord injury data set. Spinal Cord 2008; 46: 325–330.
Acknowledgements
Coloplast A/S (Denmark) has supported the work with this Data Set with an unconditional grant. We are thankful for all comments and suggestions received. We thank Susan Charlifue, Lawrence Vogel, Dan Lammertse, William Donovan, Inge Eriks Hoogland, Karen Smith and Peter Christensen.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Krogh, K., Perkash, I., Stiens, S. et al. International bowel function extended spinal cord injury data set. Spinal Cord 47, 235–241 (2009). https://doi.org/10.1038/sc.2008.103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.103
Keywords
This article is cited by
-
Are micro enemas administered with a squeeze tube and a 5 cm-long nozzle as good or better than micro enemas administered with a 10 cm-long catheter attached to a syringe in people with a recent spinal cord injury? A non-inferiority, crossover randomised controlled trial
Spinal Cord (2022)
-
Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease
Spinal Cord (2022)
-
Development of a novel neurogenic bowel patient reported outcome measure: the Spinal Cord Injury Patient Reported Outcome Measure of Bowel Function & Evacuation (SCI-PROBE)
Spinal Cord (2020)
-
Bioelectric neuromodulation for gastrointestinal disorders: effectiveness and mechanisms
Nature Reviews Gastroenterology & Hepatology (2019)
-
Neural pathways for colorectal control, relevance to spinal cord injury and treatment: a narrative review
Spinal Cord (2018)