Abstract
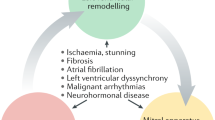
Degenerative mitral regurgitation is a major threat to public health and affects at least 24 million people worldwide, with an estimated 0.88 million disability-adjusted life years and 34,000 deaths in 2019. Improving access to diagnostic testing and to timely curative therapies such as surgical mitral valve repair will improve the outcomes of many individuals. Imaging such as echocardiography and cardiac magnetic resonance allow accurate diagnosis and have provided new insights for a better definition of the most appropriate timing for intervention. Advances in surgical techniques allow minimally invasive treatment with durable results that last for ≥20 years. Transcatheter therapies can provide good results in select patients who are considered high risk for surgery and have a suitable anatomy; the durability of such repairs is up to 5 years. Translational science has provided new knowledge on the pathophysiology of degenerative mitral regurgitation and may pave the road to the development of medical therapies that could be used to halt the progression of the disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Yadgir, S. et al. Global, regional, and national burden of calcific aortic valve and degenerative mitral valve diseases, 1990–2017. Circulation 141, 1670–1680 (2020). Important up-to-date global and national estimates demonstrating that degenerative mitral regurgitation is an important cause of disease burden among older adults.
Otto, C. M. et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143, e72–e227 (2021).
Vahanian, A. et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. J. Cardiothorac. Surg. 60, 727–800 (2021).
Russo, G. et al. Transcatheter mitral valve implantation: current status and future perspectives. Circ. Cardiovasc. Interv. 14, e010628 (2021).
Debonnaire, P., Palmen, M., Marsan, N. A. & Delgado, V. Contemporary imaging of normal mitral valve anatomy and function. Curr. Opin. Cardiol. 27, 455–464 (2012).
Namazi, F., Vo, N. M. & Delgado, V. Imaging of the mitral valve: role of echocardiography, cardiac magnetic resonance, and cardiac computed tomography. Curr. Opin. Cardiol. 35, 435–444 (2020).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Coffey, S. et al. Global epidemiology of valvular heart disease. Nat. Rev. Cardiol. 18, 853–864 (2021).
Delling, F. N. et al. Research opportunities in the treatment of mitral valve prolapse: JACC expert panel. J. Am. Coll. Cardiol. 80, 2331–2347 (2022). Landmark review article discussing the advances and gaps in knowledge of degenerative mitral regurgitation.
Levine, R. A. et al. Mitral valve disease–morphology and mechanisms. Nat. Rev. Cardiol. 12, 689–710 (2015).
Tao, G., Kotick, J. D. & Lincoln, J. Heart valve development, maintenance, and disease: the role of endothelial cells. Curr. Top. Dev. Biol. 100, 203–232 (2012).
Liu, A. C., Joag, V. R. & Gotlieb, A. I. The emerging role of valve interstitial cell phenotypes in regulating heart valve pathobiology. Am. J. Pathol. 171, 1407–1418 (2007).
Judge, D. P., Markwald, R. R., Hagege, A. A. & Levine, R. A. Translational research on the mitral valve: from developmental mechanisms to new therapies. J. Cardiovasc. Transl. Res. 4, 699–701 (2011).
van Wijngaarden, A. L., Kruithof, B. P. T., Vinella, T., Barge-Schaapveld, D. & Ajmone Marsan, N. Characterization of degenerative mitral valve disease: differences between fibroelastic deficiency and Barlow’s disease. J. Cardiovasc. Dev. Dis. 8, 23 (2021).
Fornes, P. et al. Correlation between clinical and histologic patterns of degenerative mitral valve insufficiency: a histomorphometric study of 130 excised segments. Cardiovasc. Pathol. 8, 81–92 (1999).
Rabkin, E. et al. Activated interstitial myofibroblasts express catabolic enzymes and mediate matrix remodeling in myxomatous heart valves. Circulation 104, 2525–2532 (2001).
Roberts, W. C., Vowels, T. J., Ko, J. M. & Hebeler, R. F. Jr. Gross and histological features of excised portions of posterior mitral leaflet in patients having operative repair of mitral valve prolapse and comments on the concept of missing (= ruptured) chordae tendineae. J. Am. Coll. Cardiol. 63, 1667–1674 (2014).
Dietz, H. C. et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352, 337–339 (1991).
Lindsay, M. E. et al. Loss-of-function mutations in TGFB2 cause a syndromic presentation of thoracic aortic aneurysm. Nat. Genet. 44, 922–927 (2012).
Loeys, B. L. et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat. Genet. 37, 275–281 (2005).
Kyndt, F. et al. Mutations in the gene encoding filamin A as a cause for familial cardiac valvular dystrophy. Circulation 115, 40–49 (2007).
Kyndt, F. et al. Mapping of X-linked myxomatous valvular dystrophy to chromosome Xq28. Am. J. Hum. Genet. 62, 627–632 (1998).
Durst, R. et al. Mutations in DCHS1 cause mitral valve prolapse. Nature 525, 109–113 (2015).
Toomer, K. A. et al. Primary cilia defects causing mitral valve prolapse. Sci. Transl. Med. 11, eaax0290 (2019).
Ta-Shma, A. et al. Congenital valvular defects associated with deleterious mutations in the PLD1 gene. J. Med. Genet. 54, 278–286 (2017).
Wunnemann, F. et al. Loss of ADAMTS19 causes progressive non-syndromic heart valve disease. Nat. Genet. 52, 40–47 (2020).
Kyryachenko, S. et al. Chromatin accessibility of human mitral valves and functional assessment of MVP risk loci. Circ. Res. 128, e84–e101 (2021).
Yu, M. et al. Genome-wide association study-driven gene-set analyses, genetic, and functional follow-up suggest GLIS1 as a susceptibility gene for mitral valve prolapse. Circ. Genom. Precis. Med. 12, e002497 (2019).
Armstrong, E. J. & Bischoff, J. Heart valve development: endothelial cell signaling and differentiation. Circ. Res. 95, 459–470 (2004).
Milgrom-Hoffman, M. et al. The heart endocardium is derived from vascular endothelial progenitors. Development 138, 4777–4787 (2011).
Puceat, M. Embryological origin of the endocardium and derived valve progenitor cells: from developmental biology to stem cell-based valve repair. Biochim. Biophys. Acta 1833, 917–922 (2013).
Norris, R. A. et al. Periostin regulates atrioventricular valve maturation. Dev. Biol. 316, 200–213 (2008).
Morse, D. E., Hamlett, W. C. & Noble, C. W. Jr. Morphogenesis of chordae tendineae. I: scanning electron microscopy. Anat. Rec. 210, 629–638 (1984).
Sauls, K. et al. Developmental basis for filamin-A-associated myxomatous mitral valve disease. Cardiovasc. Res. 96, 109–119 (2012).
Kruithof, B. P. T. et al. Stress-induced remodelling of the mitral valve: a model for leaflet thickening and superimposed tissue formation in mitral valve disease. Cardiovasc. Res. 116, 931–943 (2020). Experimental model demonstrating the structural changes to the mitral leaflets in degenerative mitral regurgitation.
Sabbag, A. et al. EHRA expert consensus statement on arrhythmic mitral valve prolapse and mitral annular disjunction complex in collaboration with the ESC Council on valvular heart disease and the European Association of Cardiovascular Imaging endorsed by the Heart Rhythm Society, by the Asia Pacific Heart Rhythm Society, and by the Latin American Heart Rhythm Society. Europace 24, 1981–2003 (2022).
Basso, C. & Perazzolo Marra, M. Mitral annulus disjunction: emerging role of myocardial mechanical stretch in arrhythmogenesis. J. Am. Coll. Cardiol. 72, 1610–1612 (2018).
Basso, C. et al. Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 132, 556–566 (2015).
Perazzolo Marra, M. et al. Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circ. Cardiovasc. Imaging 9, e005030 (2016).
van Wijngaarden, A. L. et al. Identification of known and unknown genes associated with mitral valve prolapse using an exome slice methodology. J. Med. Genet. 57, 843–850 (2020). Important study demonstrating new genes associated with the presence of degenerative mitral regurgitation.
Yang, L. T. et al. Mitral valve prolapse patients with less than moderate mitral regurgitation exhibit early cardiac chamber remodeling. J. Am. Soc. Echocardiogr. 33, 815–825.e2 (2020).
Constant Dit Beaufils, A. L. et al. Replacement myocardial fibrosis in patients with mitral valve prolapse: relation to mitral regurgitation, ventricular remodeling, and arrhythmia. Circulation 143, 1763–1774 (2021).
Kitkungvan, D. et al. Myocardial fibrosis in patients with primary mitral regurgitation with and without prolapse. J. Am. Coll. Cardiol. 72, 823–834 (2018).
Kitkungvan, D. et al. Prognostic implications of diffuse interstitial fibrosis in asymptomatic primary mitral regurgitation. Circulation 140, 2122–2124 (2019). Landmark article demonstrating the relevance of left ventricular myocardial tissue characterization with cardiac magnetic resonance in patients with severe degenerative mitral regurgitation.
Ajmone Marsan, N. et al. Valvular heart disease: shifting the focus to the myocardium. Eur. Heart J. 44, 28–40 (2023).
van Wijngaarden, A. L. et al. Prognostic impact of extra-mitral valve cardiac involvement in patients with primary mitral regurgitation. JACC Cardiovasc. Imaging 15, 961–970 (2022).
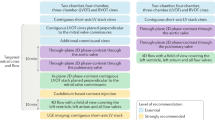
Lancellotti, P. et al. Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper. Eur. Heart J. Cardiovasc. Imaging 23, e171–e232 (2022).
Zoghbi, W. A. et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 30, 303–371 (2017).
Hahn, R. T. et al. Recommended standards for the performance of transesophageal echocardiographic screening for structural heart intervention: from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 35, 1–76 (2022). Important guide on how to perform transoesophageal echocardiography to select patients for interventional treatment of degenerative mitral regurgitation.
Nicoara, A. et al. Guidelines for the use of transesophageal echocardiography to assist with surgical decision-making in the operating room: a surgery-based approach: from the American Society of Echocardiography in collaboration with the Society of Cardiovascular Anesthesiologists and the Society of Thoracic Surgeons. J. Am. Soc. Echocardiogr. 33, 692–734 (2020).
Lancellotti, P. et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Heart J. Cardiovasc. Imaging 17, 1191–1229 (2016).
Liu, B., Edwards, N. C., Pennell, D. & Steeds, R. P. The evolving role of cardiac magnetic resonance in primary mitral regurgitation: ready for prime time. Eur. Heart J. Cardiovasc. Imaging 20, 123–130 (2019).
Penicka, M. et al. Prognostic implications of magnetic resonance-derived quantification in asymptomatic patients with organic mitral regurgitation: comparison with Doppler echocardiography-derived integrative approach. Circulation 137, 1349–1360 (2018). Landmark article demonstrating the incremental prognostic value of cardiac magnetic resonance to quantify degenerative mitral regurgitation in asymptomatic patients.
Freed, L. A. et al. Mitral valve prolapse in the general population: the benign nature of echocardiographic features in the Framingham Heart Study. J. Am. Coll. Cardiol. 40, 1298–1304 (2002).
Avierinos, J. F. et al. Natural history of asymptomatic mitral valve prolapse in the community. Circulation 106, 1355–1361 (2002).
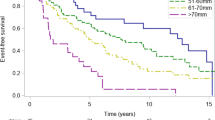
Grigioni, F. et al. Outcomes in mitral regurgitation due to flail leaflets: a multicenter European study. JACC Cardiovasc. Imaging 1, 133–141 (2008).
Antoine, C. et al. Clinical outcome of degenerative mitral regurgitation: critical importance of echocardiographic quantitative assessment in routine practice. Circulation 138, 1317–1326 (2018).
Tribouilloy, C. et al. Long-term mortality associated with left ventricular dysfunction in mitral regurgitation due to flail leaflets: a multicenter analysis. Circ. Cardiovasc. Imaging 7, 363–370 (2014).
Tribouilloy, C. et al. Survival implication of left ventricular end-systolic diameter in mitral regurgitation due to flail leaflets a long-term follow-up multicenter study. J. Am. Coll. Cardiol. 54, 1961–1968 (2009).
Hiemstra, Y. L. et al. Prognostic value of global longitudinal strain and etiology after surgery for primary mitral regurgitation. JACC Cardiovasc. Imaging 13, 577–585 (2020).
Enriquez-Sarano, M. & Sundt, T. M. 3rd Early surgery is recommended for mitral regurgitation. Circulation 121, 804–811 (2010). discussion 812.
Gillinov, A. M. et al. Should patients with severe degenerative mitral regurgitation delay surgery until symptoms develop? Ann. Thorac. Surg. 90, 481–488 (2010).
Suri, R. M. et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA 310, 609–616 (2013).
Lazam, S. et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation: analysis of a large, prospective, multicenter, international registry. Circulation 135, 410–422 (2017). Landmark article in a large population with degenerative mitral regurgitation comparing surgical mitral valve repair and mitral valve replacement.
Barbieri, A. et al. Prognostic and therapeutic implications of pulmonary hypertension complicating degenerative mitral regurgitation due to flail leaflet: a multicenter long-term international study. Eur. Heart J. 32, 751–759 (2011).
Essayagh, B. et al. Prognostic implications of left atrial enlargement in degenerative mitral regurgitation. J. Am. Coll. Cardiol. 74, 858–870 (2019).
Rusinaru, D. et al. Left atrial size is a potent predictor of mortality in mitral regurgitation due to flail leaflets: results from a large international multicenter study. Circ. Cardiovasc. Imaging 4, 473–481 (2011).
Grigioni, F. et al. Long-term implications of atrial fibrillation in patients with degenerative mitral regurgitation. J. Am. Coll. Cardiol. 73, 264–274 (2019).
Hayashi, H. et al. Prognostic significance of moderate primary mitral regurgitation and concomitant paroxysmal atrial fibrillation. J. Cardiol. 75, 309–314 (2020).
Kusunose, K., Popovic, Z. B., Motoki, H. & Marwick, T. H. Prognostic significance of exercise-induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ. Cardiovasc. Imaging 6, 167–176 (2013).
Grigioni, F. et al. The MIDA mortality risk score: development and external validation of a prognostic model for early and late death in degenerative mitral regurgitation. Eur. Heart J. 39, 1281–1291 (2018).
Nagata, Y. et al. Abnormal mechanics relate to myocardial fibrosis and ventricular arrhythmias in patients with mitral valve prolapse. Circ. Cardiovasc. Imaging 16, e014963 (2023).
Miller, M. A. et al. Arrhythmic mitral valve prolapse: JACC review topic of the week. J. Am. Coll. Cardiol. 72, 2904–2914 (2018).
Basso, C., Iliceto, S., Thiene, G. & Perazzolo Marra, M. Mitral valve prolapse, ventricular arrhythmias, and sudden death. Circulation 140, 952–964 (2019).
Morningstar, J. E. et al. Mitral valve prolapse induces regionalized myocardial fibrosis. J. Am. Heart Assoc. 10, e022332 (2021).
Dziadzko, V. et al. Outcome and undertreatment of mitral regurgitation: a community cohort study. Lancet 391, 960–969 (2018).
Shuhaiber, J. H., Ho, S. Y., Rigby, M. & Sethia, B. Current options and outcomes for the management of atrioventricular septal defect. Eur. J. Cardiothorac. Surg. 35, 891–900 (2009).
Badhwar, V. et al. Volume-outcome association of mitral valve surgery in the United States. JAMA Cardiol. 5, 1092–1101 (2020).
Carpentier, A. Cardiac valve surgery – the “French correction”. J. Thorac. Cardiovasc. Surg. 86, 323–337 (1983).
Gammie, J. S. et al. Safety and performance of a novel transventricular beating heart mitral valve repair system: 1-year outcomes. Eur. J. Cardiothorac. Surg. 59, 199–206 (2021).
Marin Cuartas, M. et al. Mitral valve repair: robotic and other minimally invasive approaches. Prog. Cardiovasc. Dis. 60, 394–404 (2017).
Castillo, J. G., Anyanwu, A. C., Fuster, V. & Adams, D. H. A near 100% repair rate for mitral valve prolapse is achievable in a reference center: implications for future guidelines. J. Thorac. Cardiovasc. Surg. 144, 308–312 (2012).
David, T. E., David, C. M., Tsang, W., Lafreniere-Roula, M. & Manlhiot, C. Long-term results of mitral valve repair for regurgitation due to leaflet prolapse. J. Am. Coll. Cardiol. 74, 1044–1053 (2019).
Javadikasgari, H. et al. Simple versus complex degenerative mitral valve disease. J. Thorac. Cardiovasc. Surg. 156, 122–129.e16 (2018).
Kang, D. H. et al. Early surgery versus conventional treatment for asymptomatic severe mitral regurgitation: a propensity analysis. J. Am. Coll. Cardiol. 63, 2398–2407 (2014).
Gammie, J. S. et al. Isolated mitral valve surgery: the Society of Thoracic Surgeons adult cardiac surgery database analysis. Ann. Thorac. Surg. 106, 716–727 (2018).
Lesevic, H. et al. Long-term outcomes after mitraclip implantation according to the presence or absence of EVEREST inclusion criteria. Am. J. Cardiol. 119, 1255–1261 (2017).
Benfari, G. et al. Association of transcatheter edge-to-edge repair with improved survival in older patients with severe, symptomatic degenerative mitral regurgitation. Eur. Heart J. 43, 1626–1635 (2022).
Feldman, T. et al. Percutaneous repair or surgery for mitral regurgitation. N. Engl. J. Med. 364, 1395–1406 (2011). First randomized clinical study comparing the efficacy of transcatheter edge-to-edge mitral valve repair and surgical mitral valve repair or replacement in patients with degenerative mitral regurgitation.
Feldman, T. et al. Randomized comparison of percutaneous repair and surgery for mitral regurgitation: 5-year results of EVEREST II. J. Am. Coll. Cardiol. 66, 2844–2854 (2015).
Mack, M. et al. Transcatheter mitral valve therapy in the United States: a report from the STS-ACC TVT registry. J. Am. Coll. Cardiol. 78, 2326–2353 (2021).
Lim, D. S. et al. Randomized comparison of transcatheter edge-to-edge repair for degenerative mitral regurgitation in prohibitive surgical risk patients. JACC Cardiovasc. Interv. 15, 2523–2536 (2022).
Chikwe, J. et al. Mitral surgery after transcatheter edge-to-edge repair: Society of Thoracic Surgeons database analysis. J. Am. Coll. Cardiol. 78, 1–9 (2021). Large registry demonstrating the rate of mitral valve surgery after transcatheter edge-to-edge mitral valve repair.
D’Onofrio, A. et al. Outcomes of transapical mitral valve repair with neochordae implantation. J. Thorac. Cardiovasc. Surg. 165, 1036–1046.e4 (2022).
Latib, A. et al. First-in-human transseptal transcatheter mitral chordal repair. JACC Cardiovasc. Interv. 15, 1768–1769 (2022).
von Bardeleben, R. S. et al. First in human transcatheter COMBO mitral valve repair with direct ring annuloplasty and neochord leaflet implantation to treat degenerative mitral regurgitation: feasibility of the simultaneous toolbox concept guided by 3D echo and computed tomography fusion imaging. Eur. Heart J. 39, 1314–1315 (2018).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42, 3599–3726 (2021).
Akowuah, E. F. et al. Minithoracotomy vs conventional sternotomy for mitral valve repair: a randomized clinical trial. JAMA 329, 1957–1966 (2023).
Elias, P. et al. Deep learning electrocardiographic analysis for detection of left-sided valvular heart disease. J. Am. Coll. Cardiol. 80, 613–626 (2022).
Tromp, J. et al. Automated interpretation of systolic and diastolic function on the echocardiogram: a multicohort study. Lancet Digit. Health 4, e46–e54 (2022).
Krishna, H. et al. Fully automated artificial intelligence assessment of aortic stenosis by echocardiography. J. Am. Soc. Echocardiogr. 36, 769–777 (2023).
Author information
Authors and Affiliations
Contributions
V.D. and M.A.B. defined the outline of the review and performed the literature search. All the authors contributed to the drafting of the manuscript, reviewed the compiled version, provided constructive feedback and suggestions for improvement and approved the final version for submission. Overview of Primer: V.D.
Corresponding author
Ethics declarations
Competing interests
V.D. received speaker fees from Edwards Lifesciences (aortic valve disease), Medtronic (aortic valve disease), Novartis (heart failure) and Philips (echocardiography), and consulting fees from Edwards Lifesciences (tricuspid valve disease) and Novo Nordisk (heart failure). M.A.B. declares that his hospital receives speakers’ honoraria and/or consulting fees on his behalf from Edwards Lifesciences, Medtronic, Abbott and Artivion. N.A.M. received speaker fees from Abbott Vascular, Philips Ultrasound, GE Healthcare and Ormon, and research grants from Pfizer, Novartis, Alnylam and Pie Medical. R.T.H. reports speaker fees from Abbott Structural, Baylis Medical, Edwards Lifesciences, Medtronic and Philips Healthcare; she has institutional consulting contracts for which she receives no direct compensation with Abbott Structural, Edwards Lifesciences, Medtronic and Novartis; she is Chief Scientific Officer for the Echocardiography Core Laboratory at the Cardiovascular Research Foundation for multiple industry-sponsored tricuspid valve trials, for which she receives no direct industry compensation. R.A.N. reports funding from the National Institutes of Health (grant number C06 RR018823, from the Extramural Research Facilities Program of the National Center for Research Resources). Other funding sources: National Institutes of Health (GM103444, R.A.N.; HL149696, R.A.N.; HL131546, R.A.N.). L.Z. is funded by the South African Medical Research Council (SAMRC) through its Division of Research Capacity Development under the Mid-Career Scientist Programme from funding received from the South African National Treasury. The contents hereof are the sole responsibility of the authors and do not necessarily represent the official views of the SAMRC. L.Z. also receives support from the National Research Foundation of South Africa (NRFSA), as well as the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement, via the African Research Leader Award (MR/S005242/1). R.O.B. declares no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks S. Maréchaux, V. Rudolph and Y. Topilsky for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41572_2023_478_MOESM1_ESM.mp4
Supplementary Video 1 Minimally invasive surgical repair of mitral valve prolapse. The valve exposure and the steps to achieve a successful mitral valve repair with minimally invasive surgery are shown.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Delgado, V., Ajmone Marsan, N., Bonow, R.O. et al. Degenerative mitral regurgitation. Nat Rev Dis Primers 9, 70 (2023). https://doi.org/10.1038/s41572-023-00478-7
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-023-00478-7