Abstract
The efficacy and safety of blood pressure lowering in patients with heart failure with preserved ejection fraction (HFpEF) remain unknown. We systematically searched PubMed/Medline, ICHUSHI, EMBASE, and the Cochrane Central Library database for randomized controlled trials (RCTs) assessing the efficacy and safety of blood pressure lowering in patients with HFpEF that were published from January 1996 to July 2017. Our study included a total of 10 RCTs involving 13,091 patients with HFpEF that compared all-cause mortality, cardiovascular mortality, heart failure hospitalization, renal dysfunction, and/or hypotension between drug intervention and control groups. Then, we analyzed systolic blood pressure (SBP) before and during trials using the SBP from the RCTs data. SBP decreased in the intervention group (134.7–130.2 mmHg) more than that in the control group (134.4–133.3 mmHg), and heart failure hospitalization was reduced in the intervention group compared to that in the control group [RR 0.89 (0.82–0.97), P = 0.006]. There was no effect of treatment on all-cause mortality, cardiovascular mortality, and hypotension. However, in the studies that compared renal function, SBP decreased in the intervention group (134.3–129.6 mmHg) more than that in the control group (134.0–132.8 mmHg), and the occurrence of renal dysfunction increased in the intervention group compared to that in the control group [RR 1.52 (1.31–1.76), P < 0.00001)]. Blood pressure lowering that achieves SBP levels of ~130 mmHg may be related to the reduction in heart failure hospitalization in patients with HFpEF, but it also possibly leads to an increased risk of renal dysfunction.
Similar content being viewed by others
Introduction
Heart failure (HF) is a major cause of morbidity and mortality [1], and it has become a major epidemic throughout the world. Heart failure with preserved ejection fraction (HFpEF) accounts for ~50% of HF cases [2, 3], and its prevalence relative to HF with reduced ejection fraction (HFrEF) continues to rise [4]. Heart failure readmission is common in HFpEF, which is similar to HFrEF [5]. However, there are no established treatments for patients with HFpEF despite the availability of numerous pharmacological and nonpharmacological therapies that have been proven to improve survival and reduce HF hospitalization in patients with HFrEF [6].
Hypertension is a major contributor to the development of HFpEF, whereas, obesity, coronary artery disease, diabetes mellitus, atrial fibrillation, and hyperlipidemia are also highly prevalent in HFpEF according to population-based studies and registries [3, 7, 8]. The current guidelines for managing hypertension recommend strict blood pressure (BP) control in patients with HFpEF [9, 10]. However, in patients with HFpEF, there was no convincing evidence per se for the efficacy and safety of BP lowering.
In this study, we aimed to systematically review clinical trials that evaluated the effects of drug therapy lowering BP among patients with HFpEF.
Methods
Data sources and searches
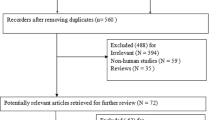
This systematic review and meta-analysis were conducted according to the PRISMA statement [11]. We performed a systematic search of PubMed/Medline, Cochrane Library, EMBASE, and Igaku Chuo Zasshi (ICHUSHI: database of Japanese journals launched by the Japan Medical Abstracts Society) for studies published from January 1996 to 24 July 2017 using medical subject headings and relevant text words for heart failure with preserved ejection fraction (heart failure, diastolic [MESH] and various text words, such as diastolic dysfunction, preserved left ventricular ejection fraction, preserved ejection fraction, and etc.), and BP lowering (antihypertensive agents [MESH] and various text words, such as BP lowering, BP control, and etc.). The study languages were restricted to English and Japanese.
Study selection
The literature search, data extraction, and quality assessment were conducted independently by two authors (HK, AF). The inclusion criteria were as follows: randomized controlled trials (RCTs) that compared the effects of BP lowering (e.g., renin-angiotensin system inhibitors, diuretics, and β-blockers) to a placebo or control treatment among patients with HFpEF, which was defined as HF with LVEF ≥ 40%, on all-cause mortality, cardiovascular mortality, heart failure hospitalization, renal dysfunction, and/or hypotension. The exclusion criteria were RCTs that did not report systolic BP (SBP) measurements before and/or during randomized treatment.
Data extraction and quality assessment
The data collected from each paper included baseline patient characteristics (age, mean systolic and diastolic BP, history of hypertension, mean left ventricular ejection fraction, and definition of heart failure), medication, follow-up duration, mean SBP and DBP during trial, outcome events, and adverse events. We judged study equivalency by evaluating trial procedures for randomization, concealment of treatment allocation, the similarity of treatment groups at baseline, the provision of a description about the eligibility criteria, completeness of follow-up, and the use of intention-to-treat analysis. The Cochrane Collaboration’s tool was used for assessing the risk of bias. Any disagreement concerning the collected data was adjudicated by a third reviewer.
Statistical analysis
The individual study Risk Ratio (RR) and 95% CI were calculated for each outcome before pooling the data. Baseline and achieved BP levels were also calculated. Random-effects models were used to estimate the pooled RR for the binary outcomes, and weighted mean differences were determined for continuous outcomes with 95% CI. Statistical heterogeneity across studies was quantified using the Cochran Chi-squared test and I2 statistics. Publication bias was assessed using funnel plots. The statistical analyses were performed using Review Manager software (version 5.3, Cochrane Collaboration, Oxford, UK).
Results
Ten RCTs (including one with two separate comparisons) that compared all-cause mortality, cardiovascular mortality, heart failure hospitalization, or adverse events between drug intervention and control groups in 13,091 patients with HFpEF were included and analyzed in our study (Table 1 and Fig. 1) [12,13,14,15,16,17,18,19,20,21]. The mean SBP changed from 134.5 to 129.8 mmHg in the drug intervention group and changed from 134.2 to 132.9 mmHg in the control group, which indicated that more SBP lowering occurred in the drug intervention group than that in the control group.
All-cause mortality
There were nine RCTs (including one with two separate comparisons) that reported all-cause mortality events, and the meta-analysis for these nine RCTs showed no significant difference between the intervention and control groups [RR 0.98(0.91–1.06), P = 0.69], although they did demonstrate that SBP decreased more in the intervention group (134.5–129.8 mmHg) than that in the control group (134.2–132.9 mmHg) (Fig. 2).
Forest plot and funnel plot of the outcomes for all-cause mortality in randomized controlled trials between the drug intervention and control groups of patients with HFpEF. SBP decreased more in the intervention group (134.5–129.8 mmHg) than that in the control group (134.2–132.9 mmHg) before and during trials
Cardiovascular mortality
There were six RCTs (including one with two separate comparisons) that reported cardiovascular mortality events, and the meta-analysis of these six RCTs showed no significant difference between the intervention and control groups [RR 0.99 (0.89–1.09), P = 0.80], although they demonstrated that SBP decreased in the intervention group (134.6–130.3 mmHg) more than that in the control group (134.4–133.3 mmHg) (Fig. 3).
Forest plot and funnel plot of the outcomes for cardiovascular mortality in randomized controlled trials between the drug intervention and control groups of patients with HFpEF. SBP decreased more in the intervention group (134.6–130.3 mmHg) than that in the control group (134.4–133.3 mmHg) before and during trials
Heart failure hospitalization
There were eight RCTs (including one with two separate comparisons) that reported heart failure hospitalization events, and the meta-analysis of these eight RCTs showed that heart failure hospitalization was reduced in the intervention group compared to that in the control group [RR 0.89 (0.82–0.97), P = 0.006], and they demonstrated that SBP was decreased in the intervention group (134.7–130.2 mmHg) more than that in the control group (134.4–133.3 mmHg) (Fig. 4).
Forest plot and funnel plot of the outcomes for heart failure hospitalization in randomized controlled trials between the drug intervention and control groups of patients with HFpEF. SBP decreased more in the intervention group (134.7–130.2 mmHg) than that in the control group (134.4–133.3 mmHg) before and during trials
Worsening renal function
We analyzed nine RCTs that included data about the occurrence of worsening renal function, and the meta-analysis of those nine RCTs demonstrated an increased occurrence of worsening renal function in the intervention group compared to that in the control group [RR 1.52 (1.31–1.76), P < 0.00001]. Additionally, SBP decreased more in the intervention group (134.3–129.6 mmHg) than that in the control group (134.0–132.8 mmHg) (Fig. 5).
Forest plot and funnel plot of the outcomes for worsening renal function in randomized controlled trials between the drug intervention and control groups of patients with HFpEF. SBP decreased more in the intervention group (134.3–129.6 mmHg) than that in the control group (134.0–132.8 mmHg) before and during trials
Hypotension
We analyzed five RCTs that included data about the occurrence of hypotension, and the meta-analysis of those five RCTs demonstrated that there was no significant occurrence of hypotension between the intervention and control groups [RR 1.36 (0.75–2.46), P = 0.31], although SBP decreased in the intervention group (136.8–131.8 mmHg) more than that in the control group (136.4–136.0 mmHg) (Fig. 6).
Forest plot and funnel plot of the outcomes for hypotension in randomized controlled trials between the drug intervention and control groups of patients with HFpEF. SBP decreased more in the intervention group (136.8–131.8 mmHg) than that in the control group (136.4–136.0 mmHg) before and during trials
Study quality and publication bias
One or two studies were identified as having a high risk of bias among the included intervention studies for each outcome (Supplementary Table 1-5). The funnel plots for all-cause mortality, cardiovascular mortality, heart failure hospitalization, worsening renal function, and hypotension were symmetrical (Figs. 2–6).
Discussion
This study demonstrated that heart failure hospitalization was reduced after drug intervention that led to more SBP lowering (down to ~130 mmHg) compared to that in the control group, although there were no significant differences in all-cause mortality and cardiovascular mortality between the drug intervention and control groups.
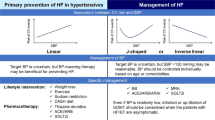
The 2018 ESC/ESH Guidelines for the management of arterial hypertension recommended that SBP lowering to <140/90 mmHg should be considered for HFpEF as well as HFrEF [22]. However, there was no evidence to support a target BP of 140 mmHg in HFpEF. Recently, the SPRINT trial showed that intensive BP control (SBP target of < 120 mmHg for the automated office BP measurement) lowered the rates of fatal and nonfatal major cardiovascular events and death from any cause in individuals without diabetes who had an SBP of 130 mmHg or higher [23]. Thus, the results suggest that intensive BP control could improve outcomes in HFpEF. The most recent American guidelines for the management of hypertension recommended SBP lowering below 130 mmHg after management of volume overload in patients with HFpEF and persistent hypertension, although there was no convincing evidence to support this guidelines [10].
This study is the first meta-analysis about the effects of drug therapy lowering SBP on the outcomes for HFpEF. The results suggest that SBP lowering to 130 mmHg by drug intervention should be considered because of the reduction in heart failure hospitalization. Although the precise mechanism remains unknown, Solomon et al. [24] demonstrated that the degree of improvement in annular relaxation velocity, which is an indicator of LV diastolic dysfunction, was associated with the extent of SBP reduction, and patients with the lowest achieved SBP had the highest final diastolic relaxation velocities. Thus, their results may support our study.
Next, this study demonstrated an increased occurrence of renal dysfunction in the drug intervention group compared to that in the control group, in association with additional SBP lowering (down to ~130 mmHg) compared with the control, although there was no significant difference in hypotension between the drug intervention and control groups. The SPRINT trial also showed an increase in serious adverse events related to low BP, especially hypotension, syncope, and acute kidney injury [23]. A recent network meta-analysis including the SPRINT trial [25] demonstrated that in patients with hypertension, an on-treatment systolic BP target of <130 mmHg achieved the optimal balance between efficacy and safety for the prevention of stroke, myocardial infarction, and death, although heart failure was not assessed in the study.
From our systematic review and meta-analysis, the lower safety limit for SBP remains undetermined in patients with HFpEF. A recent observational study of the OPTIMIZE-HF registry showed that a discharge SBP level <120 mmHg was associated with a higher risk of HF readmission or all-cause mortality in patients with HFpEF [26], which suggests that SBP lowering below 120 mmHg may not be recommended. However, the low SBP group included elderly patients, patients with a reduced glomerular filtration ratio, and patients who did not receiving an ACE inhibitor or angiotensin receptor blocker in this observational study. Therefore, the lower safety limit for SBP to prevent major adverse events in HFpEF patients should be addressed in future prospective RCTs.
In general, HFpEF is defined when LVEF is ≥50%. The present study includes RCTs that having various definitions of HFpEF, i.e., LVEF ranging from >40% to >50%. Recently, HF with LVEF in the range of 40–49% has been regarded as HF with borderline EF or HF with mid-range EF (HFmrEF) [27, 28]. Thus, it should be considered possible that not only patients with HFpEF but also those who have HF with borderline EF or HFmrEF were included in the present study.
At baseline, mean SBP was relatively well-controlled at ~134 mmHg, and the average SBP reduction was as small as 3-4 mmHg in both the intervention and control groups. This level of SBP may be a possible reason why drug intervention failed to show a significant decrease in all-cause mortality and cardiovascular mortality. On the other hand, despite this finding, it is notable that the drug intervention with SBP lowering in patients with HFpEF decreased HF hospitalization and increased renal dysfunction. We cannot deny the possibility that drug-specific effects independent of BP might have influenced the results of this study in addition to the BP lowering effects.
With regard to the treatment of HFpEF with hypertension, first-line antihypertensive agents to improve the prognosis have not been established because of the lack of compelling evidence based on RCTs [9, 10, 22]. Our systematic review and meta-analysis were not able to examine this problem. Thus, future RCTs should address this issue in the pharmaceutical treatment of HFpEF.
Study limitations
There were several limitations in this study, including (1) for RCTs analyzed in the present study, the prevalence of hypertension varied, i.e., it ranged from 28 to 100% in each study group, (2) the definitions of renal dysfunction and hypotension were not identical in the RCTs, and (3) independent drug effects in addition to BP lowering effects may have influenced the results of this study.
Conclusion
In patients with HFpEF, SBP lowering to ~130 mmHg was related to a risk reduction of HF hospitalization. Nevertheless, careful attention should be paid to potential increases in renal dysfunction and other adverse events. Further RCTs are needed to confirm the treatment effects of intensive BP lowering in patients with HFpEF.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245.
Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004;43:317–27.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9.
Shah SJ, Kitzman DW, Borlaug BA, van Heerebeek L, Zile MR, Kass DA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation. 2016;134:73–90.
Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol. 2006;47:76–84.
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–69.
Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the national heart, lung, and blood institute. Circulation. 2009;119:3070–7.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, et al. CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362:777–81.
Zi M, Carmichael N, Lye M. The effect of quinapril on functional status of elderly patients with diastolic heart failure. Cardiovasc Drugs Ther. 2003;17:133–9.
Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. PEP-CHF Investigators. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–45.
Yip GW, Wang M, Wang T, Chan S, Fung JW, Yeung L, et al. The Hong Kong diastolic heart failure study: a randomised controlled trial of diuretics, irbesartan and ramipril on quality of life, exercise capacity, left ventricular global and regional function in heart failure with a normal ejection fraction. Heart. 2008;94:573–80.
Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. I-PRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–67.
Deswal A, Richardson P, Bozkurt B, Mann DL. Results of the randomized aldosterone antagonism in heart failure with preserved ejection fraction trial (RAAM-PEF). J Card Fail. 2011;17:634–42.
Yamamoto K, Origasa H, Hori M. J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15:110–8.
Edelmann F, Wachter R, Schmidt AG, Kraigher-Krainer E, Colantonio C, Kamke W, et al. Aldo-DHF Investigators. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA. 2013;309:781–91.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. TOPCAT Investigators. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–92.
Miura M, Sakata Y, Miyata S, Shiba N, Takahashi J, Nochioka K, et al. SUPPORT Trial Investigators. influence of left ventricular ejection fraction on the effects of supplemental use of angiotensin receptor blocker olmesartan in hypertensive patients with heart failure. Circ J. 2016;80:2155–64.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104.
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Solomon SD, Verma A, Desai A, Hassanein A, Izzo J, Oparil S, et al. Exforge intensive control of hypertension to evaluate efficacy in diastolic dysfunction investigators. Effect of intensive versus standard blood pressure lowering on diastolic function in patients with uncontrolled hypertension and diastolic dysfunction. Hypertension. 2010;55:241–8.
Bangalore S, Toklu B, Gianos E, Schwartzbard A, Weintraub H, Ogedegbe G, et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017;130:707–19. e8.
Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 2018;3:288–97.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–327.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr. HK has received honoraria from Daiichi Sankyo Co., Mitsubishi Tanabe Pharma Co., Shionogi & Co., Dainippon Sumitomo Pharma Co., and Takeda Pharmaceutical Co. Dr. RS received honoraria from Medtronic Co., Boehringer Ingelheim Co., Eli Lilly & Co. and Mitsubishi Tanabe Pharma Co. Dr. TO received honoraria from Sanwa Kagaku Kenkyusho Co. Dr. KM received honoraria from Daiichi Sankyo Co., MSD KK., Actelion Pharmaceuticals Japan,and Nippon Boehringer Ingelheim Co. Dr. KM received research support from Bayer Co., Eisai Co., Bristol-Myers Squibb Co., Astellas Pharma Inc., MSD KK., Daiichi-Sankyo Co., Actelion Pharmaceuticals Japan., Teijin Pharma and Nippon Boehringer Ingelheim Co. The remaining authors declare they have no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawano, H., Fujiwara, A., Kai, H. et al. Effects of blood pressure lowering in patients with heart failure with preserved ejection fraction: a systematic review and meta-analysis. Hypertens Res 42, 504–513 (2019). https://doi.org/10.1038/s41440-019-0216-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0216-8