Abstract
The introduction in the past few years of advanced optical coherence tomography (OCT) techniques has greatly increased our understanding of the choroid, which is the most important vascular layer of the eye. Our study aimed to assess choroidal thickness by using swept-source OCT (SS-OCT) in essential hypertensive patients (EHs) with and without early-stage chronic kidney disease (CKD). We enrolled 100 EHs, of whom 65 were without kidney damage, and 35 had stage 1−3 CKD. In all of the participants, SS-OCT and a routine biochemical workup were performed. Glomerular filtration rate (GFR) was estimated by the CKD Epidemiology Collaboration equation (eGFR). CKD was defined in agreement with the Kidney Disease Outcomes Quality Initiative Kidney Disease: Improving Global Outcomes 2002 guidelines. OCT measurements were performed according to the Early Treatment Diabetic Retinopathy Study (ETDRS) protocol, which divides the macula into nine subfields. The circular grid consists of three concentric rings. EHs with CKD showed thinner choroidal thicknesses than those without it (all p < 0.05), even after adjustment for potential confounding factors. Overall choroidal thickness correlated significantly and directly with eGFR (r = 0.36) and negatively with urinary albumin excretion (r = –0.39). The association of choroidal thickness with CKD was confirmed in multiple logistic regression analyses once the effects of age and other confounding variables were accounted for. The odds ratio of having early-stage CKD associated with a standard deviation increase in overall choroidal thickness was 0.43 (0.24–0.75, 95% confidence interval; p = 0.007). In conclusion, our study confirms the close relationships between changes in ocular microcirculation and renal dysfunction.
Similar content being viewed by others
Introduction
The kidney and eye are inextricably linked in arterial hypertension and other systemic diseases [1]. Alterations of the renal microcirculation have been documented in animal models of hypertensive renal damage, [2] and microvasculature changes have been suggested to play a major etiological role in a large proportion of subjects with chronic kidney disease (CKD) [1, 3,4,5]
Changes in the structure and function of the microvasculature, in addition to being related to the development of hypertension by affecting flow resistance and tissue perfusion, underlie much of the organ damage associated with high blood pressure (BP) and appear to be crucial for its pathogenesis and progression [1, 6]. Traditionally, the retina has been considered the easiest accessible window to study the state of the systemic microcirculation [5, 7], even though the choroid is the most important vascular layer of the eye.
Per unit weight, the choroid has the highest blood flow of any tissue in the body and is the vascular supply to the outer retina, retinal pigment epithelium (RPE), and possibly a portion of the optic nerve and is the only source of metabolic exchange for the avascular fovea [8].
The choroid plays a central role in the pathophysiology of many retinal diseases and can be damaged directly by acute and chronic severe elevation of BP [9, 10].
Quantitative assessment of the choroid has always been a challenging task with conventional imaging modalities, such as indocyanine green angiography and ultrasonography, because of limited image resolution and repeatability. Histological evaluation is difficult due to the lack of samples and might not be accurate owing to changes in the choroid after fixation; however, our understanding of the choroid has greatly increased over the past few years since the introduction of the enhanced depth imaging protocol for spectral-domain optical coherence tomography (SD-OCT), thus enabling the obtaining of cross-sectional images of the choroid in living eyes [11].
In particular, much attention has been paid to choroidal thickness (CTh).
It is reasonable to hypothesize that morphological alterations of the choroid, this being a pure vascular structure, could be the local expression of a more generalized vascular injury [9, 12]. However, studies exploring CTh in patients with cardiovascular (CV) risk factors or with CV diseases have shown inconsistent results.
Uncomplicated hypercholesterolemia has been associated with choroidal thickening [13], whereas cigarette smoking [14], ocular ischemic syndrome [15], chronic heart failure [16], and coronary artery disease [17] have been linked to a thinner choroid. Diabetes without retinopathy [18, 19] and carotid artery stenosis [20, 21] have shown variable associations with CTh.
There are only limited and conflicting data in the literature on the relationships of mild to moderate essential hypertension and its early renal sequelae with CTh [22,23,24,25].
There are several inherent limitations of the enhanced depth imaging protocol for SD-OCT that likely could in part explain these conflicting observations. These include the required averaging of 50–100 B scans to achieve high contrast and low speckle noise and the SD-OCT wavelength, which might not allow for accurate detection of the choroidal–scleral boundary in some cases, because of low penetration through the RPE. Furthermore, most studies using SD-OCT have used manual segmentation only at one point or a limited number of points, leading to greater variations because of focal thickening or thinning of the choroid. Swept-source OCT (SS-OCT) has the potential to overcome some of these limitations. It uses a different light source (wavelength-tunable laser) and detection method (dual-balanced photodetector), and it has good adaptability to longer imaging wavelengths. Together with higher imaging speed for dense scanning and subsequent three-dimensional image reconstruction, these features offer potential advantages in documenting the choroid, as well as highly reproducible measurements of CTh.
Balmforth et al. [25], using SD-OCT, showed choroidal thinning in adults with mild to moderate CKD with and without concomitant hypertension, compared to therapy-naive hypertensive patients with normal renal function or healthy controls.
To our knowledge, no studies have used SS-OCT to assess the relationship between renal function and CTh in patients with early-stage CKD.
Our study aimed to analyze the relationships of stage I–III CKD with CTh in essential hypertensive patients using SS-OCT.
Materials and methods
The population of this cross-sectional study was selected from Caucasian hypertensive patients consecutively attending the Unit of Nephrology and Hypertension and European Society of Hypertension Excellence center of the University of Palermo between May 2016 and May 2017.
Written informed consent was obtained from all of the patients after the nature of the study was explained to them. The study protocol followed the tenets of the Declaration of Helsinki and was approved by the local review board.
The exclusion criteria were:
-
age <20 years old and >70 years old;
-
known diabetes or fasting glycemia >126 mg/dl;
-
Systemic or ocular diseases (glaucoma, uveitis, high myopia, age-related macular degeneration, etc.) and/or a history of ophthalmic surgery that might have affected the choroidal vascular network;
-
nephroparenchymal, renovascular, malignant or endocrine hypertension or obstructive sleep apnea syndrome;
-
known proteinuria and hematuria;
-
nephritic diseases and hereditary renal diseases;
-
estimated GFR (eGFR)<15 ml/min/1.73 m2;
-
heart failure;
-
positive history or clinical signs of coronary artery disease;
-
positive history or clinical signs of cerebrovascular disease;
-
major non-CV diseases; and
-
unreliable 24-h urine collection (i.e., creatinine excretion <10 mg/kg for women and <15 mg/kg for men was considered undercollection; urinary creatinine output>30 mg/kg in men and >25 mg/kg in women was considered overcollection).
Study design
Careful clinical histories and physical examinations were performed, and routine blood chemistry, urine examination, and semiquantitative screening for microalbuminuria were obtained in all of the subjects.
Secondary forms of hypertension were excluded, as previously described [26] Patients who reported smoking cigarettes regularly during the past year were considered current smokers.
Body weight, height, and waist circumference were measured by a nurse.
Measurements
Clinic BP was considered the mean of three consecutive measurements obtained at 2-min intervals by an electronic oscillometric validated [27] device (WatchBP Office, Microlife AG, Widnau, Switzerland) 20 after 5 min of rest in a sitting position.
Routine biochemical parameter determination was performed with standard techniques using an autoanalyzer.
Low-density lipoprotein cholesterol was calculated by the Friedewald formula. Semiquantitative determination of microalbuminuria was performed by immunochemical urinary dipstick test (Micral-Test II Boehringer Mannheim, GmbH Mannheim, Germany). When this test was positive and in participants with evidence of gross proteinuria on standard urine examination (1+ or more), 24-h urine collections were performed on nonworking days to obtain quantitative measurements of urinary albumin excretion (UAE). In subjects with urinary tract infections, UAE was determined only after appropriate antibacterial treatment. The patients were advised to avoid excessive physical efforts on the day before and during the 24-h urine collections. Collections were postponed in female participants reporting menstruation and in all subjects with febrile illnesses at the time of collection. UAE was assayed by immunoturbidimetry on the Cobas Mira analyzer (Roche Instruments, Rotkreuz, Switzerland). Microalbuminuria was defined as a UAE between 30 and 300 mg/day, detected on reliable 24-h urine collections. Persons with UAE >300 mg/day were excluded from the study.
Creatinine was measured using the Creatinine Plus standardized enzymatic assay (Roche Diagnostics). eGFR was calculated using the CKD Epidemiology Collaboration (CKD-EPI) equation [28].
The classification proposed by the Kidney Disease Outcomes Quality Initiative Kidney Disease: Improving Global Outcomes (K/DOQI) 2002 clinical practice guidelines for CKD was used to define the first three stages of renal function impairment [29].
The stages of CKD were defined as follows: stage I, eGFR >90 ml/min/1.73 m2 and 24-h AER >20 μg min− 1; stage II, eGFR of 60–89 ml/min/1.73 m2 and 24-h AER >20 μg min; and stage III, eGFR of 30–59 ml/min/1.73 m2. All of the patients underwent complete eye examinations, including best-corrected visual acuity with Early Treatment Diabetic Retinopathy Study (ETDRS) charts, intraocular pressure measurements, and anterior-segment and dilated fundus evaluations. A single examiner, not aware of the clinical and biohumoral data of the patient, established the presence and level of hypertensive retinopathy, using the Keith, Wagener, and Barker classification [30]. The retino-choroidal district was evaluated morphologically by SS- OCT (DRI Triton, Topcon Inc., Japan), always in the morning during the same temporal interval (10–12 a.m.). All of the scans were performed by a single operator. The right eye was examined first. A standardized protocol was followed for all of the scans. Poor-quality scans were rejected or repeated.
The scans were then read and analyzed by two specialized ophthalmologists. Because no significant differences were noted between the two eyes, only one eye of each subject was randomly selected for analysis using a random number generator. If the image quality of the selected eye was deemed insufficient, the contralateral eye was chosen for analyses.
Quantitative analysis
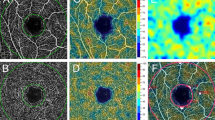
The retinal thickness (from the inner limiting membrane to the inner surface of the RPE) and CTh (from the outer surface of the RPE to the choroidal–scleral interface, CSI) were automatically calculated by the OCT mapping software. OCT measurements were performed according to the ETDRS protocol [31]. The ETDRS map divides the macula into nine subfields. The circular grid is centered over the fovea and consists of three concentric rings 1, 3, and 6 mm in diameter, respectively. The inner and outer rings are further divided into quadrants: temporal, nasal, superior, and inferior (Fig. 1a).
Measurements are displayed for each of the nine regions of the ETDRS grid for both the retina and the choroid. Furthermore, we calculated the average of the individual values of the four quadrants separately for the inner and outer rings. The average of all nine regions of the ETRDS grid (including the inner, the outer, and the central rings) was also calculated.
A single observer measured the CTh perpendicularly from the outer portion of the hyperreflective line, corresponding to the RPE, to the CSI (Fig. 1b).
Statistical analysis
The study was planned to have a sample size of 100 participants. This figure was calculated on the basis of previous investigations exploring a similar issue [25], assuming the finding of a coefficient of correlation between choroidal CTh and eGFR of at least 0.35. Thus, it was estimated that the study would have 95% power to detect the expected result (with α < 0.05).
Normal distribution of the continuous variables was assessed using the Kolmogorov–Smirnov test, and the assumption of satisfactory Gaussian distribution was met for all of the examined parameters, except for UAE, which showed a positively skewed distribution. This variable, measured only in a subset of the study population, was reported as the median and interquartile range (IQR). It was logarithmically transformed (base 10) to better satisfy distributional assumptions before parametric tests were used. All of the other normal distributed continuous variables were expressed as the mean ± standard deviation.
Categorical variables were expressed as percentage values.
The whole study population (n = 100) was divided into four subgroups: patients without CKD (no CKD) and patients with CKD divided into three stages of increasing severity, as previously defined.
Differences between subgroups were evaluated using analysis of variance (ANOVA), followed, if the overall F test was significant, by Dunnett’s post hoc test, where the no CKD group was used as the control. Adjustment for age, drug treatment for hypertension (yes = 1; no = 0), diastolic BP, serum glucose, and triglycerides was performed by analysis of covariance (ANCOVA).
For the categorical variables, comparisons were performed using the χ2 test, with the Monte Carlo method for computation of exact two-tailed α-values.
Simple regression analyses and Pearson’s correlation coefficients were used to test the relationships between chorioretinal measures and the other variables. To assess the associations of UAE with other parameters, we calculated Spearman’s rank coefficients. To assess the independent relationships between the examined variables, stepwise multiple regression models were built, including each chorioretinal parameter as the outcome variable and the variables associated with it in bivariate analyses (age, serum glucose, serum triglycerides, diastolic BP) as regressors.
Finally, we used multiple logistic regression modeling to determine the odds ratios (ORs) of having stage III CKD, microalbuminuria, or overall stage I–III CKD associated with a standard deviation increase in each CTh measure, independently of age, anti-hypertensive therapy, serum glucose, serum triglycerides, and diastolic BP. The same analyses were replicated considering CTh measures, instead of continuous variables as dichotomous ones (1 = lowest quartiles; 0 = the remaining quartiles), and overall stages I–III was the outcome variable.
In all of the multiple regression analyses, a backward stepwise procedure was used, with α = 0.15 as the cutoff for the entry or removal of variables. Collinearity was assessed by calculating the variance inflation factor (VIF): variables with VIF ≥2 were excluded from the models.
The null hypothesis was rejected with a two-tailed p < 0.05.
The statistical analyses were performed using the IBM SPSS Statistics software package, version 22 for Macintosh (SPSS, Chicago, IL, USA).
Results
Table 1 summarizes the main demographic and clinical data of the four subgroups into which the population was divided: patients without CKD (no CKD) and patients with CKD divided into three stages of increasing severity. This latter group included 30 subjects with microalbuminuria, of whom 9 also showed an eGFR <60 ml/min/1.73 m2.
In the subset of the entire study population in which a urine dipstick for microalbuminuria was positive, and 24-h UAE was determined, the median value (and IQR) of urinary albumin was 41 (31–175) mg/day.
The patients with stage III CKD were older and tended to have higher levels of serum triglycerides than those without kidney disease. The sex distribution, smoking habit, BP, BMI, waist circumference, serum glucose, hemoglobin, HDL, LDL, and total cholesterol were not significantly different between the two groups. As shown in Supplementary table 1, most of the study population (66%) was treated with anti-hypertensive drugs at enrollment. However, no difference was observed between the two groups regarding the proportion of patients pharmacologically treated for hypertension, the distribution of the various classes of BP-lowering drugs, and the percentage of subjects treated with other CV therapies.
Patients pharmacologically treated for hypertension were older and had thinner CThs than untreated subjects (Supplementary table 2), but these latter differences lost statistical significance after correction by ANCOVA for age. No significant differences were found between men and women or between smokers and non-smokers regarding choroidal and retinal thicknesses (Supplementary table 2).
As presented in Table 2a, patients with stage III CKD exhibited lower values of the measures of CTh, compared to those without CKD.
These differences remained significant even after adjustment by ANCOVA for age, body mass index, serum glucose, serum triglycerides, and systolic and diastolic BPs (Fig. 2).
Differences in choroidal thicknesses between hypertensive subjects with normal renal function and with stage 1–3 CKD. The values are given as the mean ± S.E.M. and are adjusted for age, drug treatment for hypertension, serum glucose, serum triglycerides, and diastolic BP. P values reported above the histograms are obtained by ANCOVA. *P < 0.05 vs. no CKD (Dunnett’s post hoc test)
The differences were less pronounced when we examined the retinal thickness measurements. Only some of these (Table 2b) measurements were statistically significant, but all of the differences were no longer significant once the effect of the confounding factors listed above was considered.
The bivariate analyses of correlation (Table 3) disclosed significant associations of choroidal, but not retinal, thickness measurements with age, eGFR, serum triglycerides (except choroidal central ring thickness), and glycemia (only choroidal average outer ring thickness). The relationships of CTh measurements with eGFR remained statistically significant even considering the effect of age (Fig. 3) and other covariates in multiple linear regression analyses (Table 3). In the subjects in whom the urine dipstick for microalbuminuria was positive (n = 30) 24-h UAE was determined. In this subset of the study population, the Spearman’s correlation analyses revealed that albuminuria was strongly and inversely related to all of the CTh measures (central ring: −0.380, p = 0.038; average inner ring −0.376, p = 0.04; average outer ring: −0.472, p = 0.0085; overall average: −0.398, p = 0.0294). No significant correlation was detected between any retinal thickness measurements and 24-h UAE.
Three-dimensional graph depicting the best-fit regression surface describing the multivariate relationship among overall choroidal thickness (dependent variable), age and estimated glomerular filtration rate (eGFR) (both predictor variables). The corresponding regression equation is the following: overall choroidal thickness = 0.4752 × (eGFR) − 1.3427 × (Age) + 280.35
We also performed multiple logistic regression analyses, in which stage 3 CKD was regarded as the dependent variable, while age, anti-hypertensive therapy, triglycerides, glycemia, diastolic BP, and each CTh measurement, separately from the others, were included as explanatory variables. A standard deviation (SD) increase in each CTh measure was associated with a significantly reduced chance of having an eGFR < 60 ml/min/1.73 m2: central ring, OR: 0.457 (0.231–0.902); p = 0.024; average inner ring, OR 0.381 (0.187–0.778); p = 0.008; average outer ring, OR 0.392 (0.192–0.797); p = 0.01; and average overall ring, OR 0.355 (0.182–0.692); p = 0.002.
When in the same model we replaced, as the outcome variable, stage 3 CKD with microalbuminuria, an SD increase in each CTh measure was also independently related with a reduced probability of having microalbuminuria: central ring, OR: 0.523 (0.318–0.861); p = 0.011; average inner ring, OR 0.397 (0.230–0.686); p = 0.001; average outer ring, OR 0.392 (0.224–0.686); p = 0.001; and average overall ring, OR 0.569 (0.352–0.920); p = 0.021.
We ran again the multiple regression model considering overall stage 1–3 CKD as dependent variables, and using the same covariates, we included it in the previous multivariate analyses. An SD increase in each CTh measure was associated with a significantly reduced chance of having CKD: central ring, OR: 0.549 (0.327–0.920); p = 0.023; average inner ring, OR 0.434 (0.249–0.755); p = 0.003; average outer ring, OR 0.452 (0.261–0.783); p = 0.005; and average overall ring, OR 0.428 (0.243–0.7543); p = 0.007.
Similarly, when CTh parameters were expressed as categorical variables (1 = lowest quartiles; 0 = the remaining quartiles), subjects belonging to the lowest quartiles of the CTh distribution had significantly greater odds of having stage 1–3 CKD than those with greater CTh, independently of potential confounding factors (Supplementary figure 1).
DISCUSSION
The concept that the retinal vasculature might be regarded as a window through which the body microcirculation can be observed in life easily, safely, and repeatedly has been known for more than a century and is part of the cultural knowledge of every physician [5, 32].
Less investigated are the relationships between extraocular vascular diseases and alterations of the choroid, although the latter is a highly vascularized structure that plays an important role in the control of the metabolism and volume of the eye [8, 9]. The structural evaluation of the choroid in vivo was for a long time limited by its deep location, behind the RPE, making it more difficult to reliably image. Our understanding of the choroid has been vastly augmented in recent years, since the introduction of the enhanced depth imaging protocol for SD-OCT, which has allowed for obtaining cross-sectional images of the choroid in living eyes. Our study was the first to use SS-OCT to analyze the relationships between stage I–III CKD and chorioretinal thicknesses in a group of nondiabetic essential hypertensive patients without CV complications.
The main results of our study can be summarized as follows.
-
(a)
The estimated GFR showed a direct association with CTh that was independent of age and other potentially confounding factors. In other words, when the renal function decreases, there is a progressive thinning of the choroid.
-
(b)
In subjects with a positive dipstick for microalbuminuria or with gross proteinuria, in whom 24-h urinary albumin was determined, inverse relationships were observed between the UAE and the choroidal and retinal thicknesses.
-
(c)
An independent association was detected of stage III CKD and overall stage I–III CKD with a reduction in CTh.
Our findings seem to be, at least in part, in keeping with Balmforth et al.’s [25] data, in which a European multicenter study recruited 150 patients, including 50 hypertensive subjects with normal renal function, 50 patients with CKD, and 50 healthy controls. The authors reported a direct relationship between eGFR and CTh and a negative one between the latter and proteinuria. The same authors observed thinning of the retinal and choroidal thicknesses in patients with CKD, compared with both healthy and hypertensive subjects [25]. At variance with this study, we did not find any correlation between eGFR and retinal thickness. The different OCT techniques used (SD-OCT by Balmforth et al. [25], SS-OCT in our study) and the better overall renal function of the CKD patients enrolled in our investigation (eGFR 66 ± 29 ml/min/1.73 m2), compared to that of the CKD patients in the Balmforth study (37 ± 23 ml/min/1.73 m2), might be putative reasons for this inconsistent finding. It is conceivable that the reciprocal relationships between eGFR and retinal thickness could change progressively as renal function worsens.
Previous studies, all based on the SD-OCT method, examined chorioretinal thicknesses in patients with kidney diseases [33, 34]. These studies, however, reported only the central retinal thickness ring in end-stage renal disease (ESRD) in dialytic replacement therapy, which in itself is able to reduce the CTh, likely due to rapid changes in the volume and oncotic pressure of interstitial fluids that hemodialysis can induce [33, 34]. For this reason, we excluded patients with ESRD on dialysis treatment and evaluated only patients with mild to moderate CKD.
In addition, in agreement with the Balmforth’s study, we observed in subjects with albuminuria an inverse relationship between UAE and CTh. Conversely, we did not find any significant correlation of UAE with retinal thickness, likely because of a type II statistical error due to the small number of subjects in whom UAE was measured.
The choroid is a pure vascular structure, and its thinning can reflect microvascular damage that might be the local expression of a more generalized vascular injury. It is reasonable to hypothesize that the oxidative stress, subclinical inflammation, endothelial dysfunction, and early vascular aging (EVA) that characterize CKD, since its initial stages could explain why thinning of the choroid is associated with renal function impairment.
The inverse relationships of choroidal thickness with some markers of endothelial dysfunction and vascular inflammation, such as endothelin-1, asymmetric dimethylarginine, and interleukin-6 serum levels, as well as the association of reduced choroidal thickness with increased arterial stiffness, a well-known index of EVA described by Balmforth et al. [25], seemed to support this hypothesis. Since the vessels of the choroid nourish the outer retinal layers and the RPE, it is possible that retinal alterations could occur secondary to choroidal injury.
Dysfunction of the autonomic nervous system could be evoked as a pathogenic mechanism. CKD is characterized by a state of hyperactivation of the sympathetic nervous system. Choroidal circulation, unlike the retinal circulation, has autonomous innervation. Choroidal thinning could therefore be caused by an increase in the sympathetic tone due to choroidal vascularization. Whatever the basic mechanism of CTh modulation, a possible role could be played by vascular smooth muscle components. The degree of contraction of this muscle component could affect the choroidal thickness.
We did not find any significant correlations between BP values and retino-choroidal thicknesses.
Previous reports have obtained inconsistent results.
Balmforth et al. [25] found no relationship between systolic and diastolic BP and chorioretinal thicknesses, and the latter were not different when comparing hypertensive subjects to normotensive controls. In contrast, Akay et al. [22] and Masis et al. [23] reported that the choroid was thinner in hypertensive patients compared to nonhypertensive patients. In both of these studies, renal function was not assessed; therefore, its effect on the relationship between choroid and BP values was not considered.
However, we cannot exclude the possibility that the use of out-of-office BP measurement techniques, such as 24-h ambulatory BP monitoring (ABPM) or self-measurement of BP at home, which provides a more reliable estimate of the “true” BP burden than clinic BP measurement, might have revealed a correlation between choroidal parameters and BP values.
Indeed, Gök et al. [24] recently, in 116 hypertensive patients who underwent 24-h ABPM and SD-OCT, did not find any significant relationship of choroidal thickness or the average of BP readings recorded over 24 h with circadian BP variability.
In conclusion, our study, using the innovative imaging technique SS-OCT, documented a significant association between early-stage CKD and a reduction in choroidal thickness in patients with primary hypertension.
This finding confirms the close relationship between changes in the ocular microcirculation and renal dysfunction. Further studies with different experimental designs are needed to explain the pathophysiological reasons of our results and to understand whether the information obtained about choroidal thickness with SS-OCT might have CV and renal prognostic implications.
References
Wong CW, Wong TY, Cheng C-Y, Sabanayagam C. Kidney and eye diseases: common risk factors, etiological mechanisms, and pathways. Kidney Int. 2014;85:1290–302. https://doi.org/10.1038/ki.2013.491.
Nag S, Robertson DM, Dinsdale HB. Morphological changes in spontaneously hypertensive rats. Acta Neuropathol. 1980;52:27–34.
Sabanayagam C, Tai ES, Shankar A, Lee J, Sun C, Wong TY. Retinal arteriolar narrowing increases the likelihood of chronic kidney disease in hypertension. J Hypertens. 2009;27:2209–17. https://doi.org/10.1097/HJH.0b013e328330141d.
Gu YM, Petit T, Wei FF, Thijs L, Jacobs L, Zhang ZY, et al. Renal glomerular dysfunction in relation to retinal arteriolar narrowing and high pulse pressure in seniors. Hypertens Res. 2016;39:138–43.
Mulè G, Vadalà M, Geraci G, Cottone S. Retinal vascular imaging in cardiovascular medicine: new tools for an old examination. Atherosclerosis. 2018;268:188–90.
Izzard AS, Rizzoni D, Agabiti-Rosei E, Heagerty AM. Small artery structure and hypertension: adaptive changes and target organ damage. J Hypertens. 2005;23:247–50. https://doi.org/10.1097/00004872-200502000-00002.
Cheung CYL, Ikram MK, Sabanayagam C, Wong TY. Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension. 2012;60:1094–103. https://doi.org/10.1161/HYPERTENSIONAHA.111.189142.
Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res. 2010;29:144–68. https://doi.org/10.1016/j.preteyeres.2009.12.002.
Tan KA, Gupta P, Agarwal A, Chhablani J, Cheng CY, Keane PA. et al. State of science: choroidal thickness and systemic health. Surv Ophthalmol. 2016;61:566–81. https://doi.org/10.1016/j.survophthal.2016.02.007.
Ahn SJ, Woo SJ, Park KH. Retinal and choroidal changes with severe hypertension and their association with visual outcome. Investig Ophthalmol Vis Sci. 2014;55:7775–85. https://doi.org/10.1167/iovs.14-14915.
Ferrara D, Waheed NK, Duker JS. Investigating the choriocapillaris and choroidal vasculature with new optical coherence tomography technologies. Prog Retin Eye Res. 2016;52:130–55.https://doi.org/10.1016/j.preteyeres.2015.10.002.
Novais EA, Badaró E, Allemann N, Morales MS, Rodrigues EB, de Souza Lima R, et al. Correlation between choroidal thickness and ciliary artery blood flow velocity in normal subjects. Ophthalmic Surg Lasers Imaging Retin. 2015;46:920–4.
Wong IY, Wong RL, Zhao P, Lai WW. Choroidal thickness in relation to hypercholesterolemia on enhanced depth imaging optical coherence tomography. Retina. 2013;33:423–8.
Sizmaz S, Küçükerdönmez C, Pinarci EY, Karalezli A, Canan H, Yilmaz G. The effect of smoking on choroidal thickness measured by optical coherence tomography. Br J Ophthalmol. 2013;97:601–4.
Kim DY, Joe SG, Lee JY, Kim J-G, Yang SJ. Choroidal thickness in eyes with unilateral ocular ischemic syndrome. J Ophthalmol. 2015;2015:620372.
Altinkaynak KaraN, Sayin N, Gunes H, Avsar S, Yazici A. Subfoveal choroidal thickness in patients with chronic heart failure analyzed by spectral domain optical coherence tomography. Curr Eye Res. 2014;39:1123–8.
Ahmad M, Kaszubski PA, Cobbs L, Reynolds H, Smith RT. Choroidal thickness in patients with coronary artery disease. PLoS ONE. 2017;20:e0175691 https://doi.org/10.1371/journal.pone.0175691.
Esmaeelpour M, Povazay B, Hermann B, Hofer B, Kajic V, Hale SL, et al. Mapping choroidal and retinal thickness variation in type 2 diabetes using three-dimensional 1060-nm optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:5311–6.
Xu J, Xu L, Du KF, Shao L, Chen CX, Zhou JQ, et al. Subfoveal choroidal thickness in diabetes and diabetic retinopathy. Ophthalmology. 2013;120:2023–8.
Sayin N, Kara N, Uzun F, Akturk IF. A quantitative evaluation of the posterior segment of the eye using spectral-domain optical coherence tomography in carotid artery stenosis: a pilot study. Ophthalmic Surg Lasers Imaging Retin. 2015;46:180–5.
Akcay BİS, Kardes E, Macin S, Unlu C, Ozgurhan EB, Macin A, et al. Evaluation of subfoveal choroidal thickness in internal carotid artery stenosis. J Ophthalmol. https://doi.org/10.1155/2016/5296048.
Akay F, Gundogan FC, Yolcu U, Toyran S, Uzun S. Choroidal thickness in systemic arterial hypertension. Eur J Ophthalmol. 2016;26:152–7. https://doi.org/10.5301/ejo.5000675.
Masis M, Hernandez E, Wu L. Choroidal thickness in patients with systemic hypertension. Invest Ophthalmol Vis Sci. 2011;52:5296.
Gök M, Karabas VL, Emre E, Aksar AT, Aslan MS, Ural D. Evaluation of choroidal thickness via enhanced depth-imaging optical coherence tomography in patients with systemic hypertension. Indian J Ophthalmol. 2015;63:239–43. https://doi.org/10.4103/0301-4738.156928.
Balmforth C, van Bragt JJMH, Ruijs T, Cameron JR, Kimmitt R, Moorhouse R. et al. Chorioretinal thinning in chronic kidney disease links to inflammation and endothelial dysfunction. JCI Insight. 2016;20:e89173. https://doi.org/10.1172/jci.insight.89173.
Mulè G, Nardi E, Guarino L, Cacciatore V, Geraci G, Calcaterra I. et al. Plasma aldosterone and its relationship with left ventricular mass in hypertensive patients with early-stage chronic kidney disease. Hypertens Res. 2015;38:276–83. https://doi.org/10.1038/hr.2014.171.
Stergiou GS, Tzamouranis D, Protogerou A, Nasothimiou E, Kapralos C. Validation of the Microlife Watch BP Office professional device for office blood pressure measurement according to the International protocol. Blood Press Monit. 2008;13:299–303. https://doi.org/10.1097/MBP.0b013e3283057af6.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF,III, Feldman HI. et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Bolton K, Coresh J, Culleton B, Harvey KS, Ikizler TA, Johnson CA. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification,The National Kidney Foundation. Am J Kidney Dis. 2002;39:S1–66.
Keith NM, Wagener HPBN. Some different types of essential hypertension: their course and prognosis. Am J Med Sci. 1939;197:332–43.
Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol (Chicago, Ill 1960). 1985;103:1796–1806.
Gunn RM. Ophthalmoscopic evidence of (1) arterial changes associated with chronic renal diseases and (2) of increased arterial tension. Trans Ophthalmol Soc UK. 1892;12:124–5.
Ulas F, Doğan UÅN, Keles A, Ertilav M, Tekce H, Celebi S. Evaluation of choroidal and retinal thickness measurements using optical coherence tomography in non-diabetic haemodialysis patients. Int Ophthalmol. 2013;33:533–9.
Jung JW, Chin HS, Lee DH, Yoon MH, Kim NR. Changes in subfoveal choroidal thickness and choroidal extravascular density by spectral domain optical coherence tomography after haemodialysis: a pilot study. Br J Ophthalmol. 2014;98:207–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Mulè, G., Vadalà, M., La Blasca, T. et al. Association between early-stage chronic kidney disease and reduced choroidal thickness in essential hypertensive patients. Hypertens Res 42, 990–1000 (2019). https://doi.org/10.1038/s41440-018-0195-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0195-1
Keywords
This article is cited by
-
Evaluation of subclinical changes in recently diagnosed pediatric hypertension patients without hypertensive retinopathy: an OCT study
International Ophthalmology (2023)
-
Hypertensive eye disease
Nature Reviews Disease Primers (2022)
-
Correlations between choroidal thickness and renal function in patients with retinal vein occlusion
Scientific Reports (2020)





