Abstract
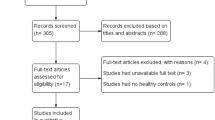
To investigate changes in foveal avascular zone parameters in individuals with prediabetes compared to normoglycemic controls. PUBMED, Scopus and Cochrane Library were searched for published articles comparing the foveal avascular zone between prediabetic individuals and normoglycemic controls as assessed by optical coherence tomography angiography (OCTA). Standardised Mean Difference (SMD) with 95% confidence interval (CI) was computed for the comparison. A total of seven studies were included in our analysis, 6 provided data for the superficial capillary plexus from 345 eyes of individuals with prediabetes and 347 eyes of controls and 4 provided data on the deep capillary plexus from 285 eyes from individuals with prediabetes and 325 eyes of controls. Foveal avascular zone (FAZ) area in the superficial capillary plexus was enlarged in individuals with prediabetes compared to normoglycemic controls (SMD = 0.23, 95% CI = 0.03–0.44, p = 0.03, I2 = 27%, 6 studies). There was no statistically significant change in the deep capillary plexus FAZ area between the two groups (SMD = 1.14, 95% CI = −0.06–2.34, p = 0.06, I2 = 97%, 4 studies). FAZ area in the superficial capillary plexus was larger in individuals diagnosed with prediabetes compared to normoglycemic controls. This finding suggests that prediabetes could induce retinal microvascular changes before the onset of clinical diabetes. More original studies are needed to validate the results of the current meta-analysis.
摘要
研究与血糖正常对照组相比, 糖尿病前期患者的中央凹无血管区 (FAZ) 参数的变化。在PUBMED、Scopus和Cochrane图书馆中搜索已发表的文章, 比较经光学相干断层扫描血管造影 (OCTA) 评估的糖尿病前期患者和血糖正常对照组之间的FAZ。根据标准化均数差 (SMD) 和95%置信区间 (CI) 进行比较。本文共纳入7项研究, 其中6项提供了来自345只糖尿病前期患眼和347只对照眼的浅层毛细血管丛的数据, 4项提供了来自285只糖尿病前期患眼和325名对照眼的深层毛细血管丛的数据。浅层毛细血管丛中的FAZ面积在糖尿病前期个体中较健康对照组扩大 (SMD = 0.23, 95% CI = 0.03–0.44, p = 0.03, I2 = 27%, 6项研究) 。两组之间的深层毛细血管丛FAZ面积变化无统计学差异性 (SMD = 1.14, 95% CI = −0.06–2.34, p = 0.06, I2 = 97%, 4项研究) 。糖尿病临床前期患者的浅层毛细血管丛中的FAZ面积更大。这一发现表明, 糖尿病前期可能在糖尿病临床前期导致视网膜微血管变化。需要更多初始研究来验证当前meta分析的结果。
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93:137–88. https://doi.org/10.1152/physrev.00045.2011.
Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharm. 2020;18:110–6. https://doi.org/10.2174/1570161117666190405165151.
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pr. 2011;94:311–21. https://doi.org/10.1016/j.diabres.2011.10.029.
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pr. 2018;138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46:S19–S40. https://doi.org/10.2337/dc23-S002.
Rooney MR, Fang M, Ogurtsova K, Ozkan B, Echouffo-Tcheugui JB, Boyko EJ, et al. Global prevalence of prediabetes. Diabetes Care. 2023;46:1388–94. https://doi.org/10.2337/dc22-2376.
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–90. https://doi.org/10.1016/S0140-6736(12)60283-9.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2015;2:17 https://doi.org/10.1186/s40662-015-0026-2.
Yin L, Zhang D, Ren Q, Su X, Sun Z. Prevalence and risk factors of diabetic retinopathy in diabetic patients: a community based cross-sectional study. Med (Baltim). 2020;99:e19236 https://doi.org/10.1097/MD.0000000000019236.
Lee KM, Sum WM. Prevalence of diabetic retinopathy in patients with recently diagnosed diabetes mellitus. Clin Exp Optom. 2011;94:371–5. https://doi.org/10.1111/j.1444-0938.2010.00574.x.
Koustenis A Jr, Harris A, Gross J, Januleviciene I, Shah A, Siesky B. Optical coherence tomography angiography: an overview of the technology and an assessment of applications for clinical research. Br J Ophthalmol. 2017;101:16–20. https://doi.org/10.1136/bjophthalmol-2016-309389.
Oliverio GW, Ceravolo I, Bhatti A, Trombetta CJ. Foveal avascular zone analysis by optical coherence tomography angiography in patients with type 1 and 2 diabetes and without clinical signs of diabetic retinopathy. Int Ophthalmol. 2021;41:649–58. https://doi.org/10.1007/s10792-020-01621-z.
Balaratnasingam C, Inoue M, Ahn S, McCann J, Dhrami-Gavazi E, Yannuzzi LA, et al. Visual Acuity Is Correlated with the Area of the Foveal Avascular Zone in Diabetic Retinopathy and Retinal Vein Occlusion. Ophthalmology. 2016;123:2352–67. https://doi.org/10.1016/j.ophtha.2016.07.008.
Ratra D, Dalan D, Prakash N, Kaviarasan K, Thanikachalam S, Das UN, et al. Quantitative analysis of retinal microvascular changes in prediabetic and diabetic patients. Indian J Ophthalmol. 2021;69:3226–34. https://doi.org/10.4103/ijo.IJO_1254_21.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71 https://doi.org/10.1136/bmj.n71.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quailty of nonrandomised studies in meta-analyses. http://www ohrica/programs/clinical_epidemiology/oxford htm 2009 Feb 1. Published online2009:2009.
Arias JD, Arango FJ, Parra MM, Sánchez-Ávila RM, Parra-Serrano GA, Hoyos AT, et al. Early microvascular changes in patients with prediabetes evaluated by optical coherence tomography angiography. Ther Adv Ophthalmol. 2021;13:25158414211047020 https://doi.org/10.1177/25158414211047020.
Li Rudvan AL, Can ME, Efe FK, Keskin M, Beyan E. Evaluation of retinal microvascular changes in patients with prediabetes. Niger J Clin Pr. 2021;24:911–8. https://doi.org/10.4103/njcp.njcp_193_20.
Kirthi V, Reed KI, Alattar K, Zuckerman BP, Bunce C, Nderitu P, et al. Multimodal testing reveals subclinical neurovascular dysfunction in prediabetes, challenging the diagnostic threshold of diabetes. Diabet Med. 2023;40:e14952 https://doi.org/10.1111/dme.14952.
Wang Y, Toyama T, Hashimoto Y, Kawai H, Azuma K, Shiraya T, et al. Association of prediabetes with retinal microvasculature on swept-source optical coherence tomography angiography in the elderly: otassha study. Retina. 2022;42:1130–6. https://doi.org/10.1097/IAE.0000000000003416.
Xu Y, Zhu X, Wang Y, Chu Z, Wang RK, Lu L, et al. Early retinal microvasculopathy in prediabetic patients and correlated factors [published online ahead of print, 2022 Nov 16]. Ophthalmic Res. 2022;https://doi.org/10.1159/000527957.
Zagst AJ, Smith JD, Wang R, Harrison WW. Foveal avascular zone size and mfERG metrics in diabetes and prediabetes: a pilot study of the relationship between structure and function [published online ahead of print, 2023 Jul 26]. Doc Ophthalmol. 2023;https://doi.org/10.1007/s10633-023-09943-w.
Sun Z, Yang D, Tang Z, Ng DS, Cheung CY. Optical coherence tomography angiography in diabetic retinopathy: an updated review. Eye. 2021;35:149–61. https://doi.org/10.1038/s41433-020-01233-y.
Hammes HP, Lin J, Renner O, Shani M, Lundqvist A, Betsholtz C, et al. Pericytes and the pathogenesis of diabetic retinopathy. Diabetes. 2002;51:3107–12. https://doi.org/10.2337/diabetes.51.10.3107.
Tesfamariam B. Free radicals in diabetic endothelial cell dysfunction. Free Radic Biol Med. 1994;16:383–91. https://doi.org/10.1016/0891-5849(94)90040-x.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N. Engl J Med. 1994;331:1480–7. https://doi.org/10.1056/NEJM199412013312203.
Rivera JC, Dabouz R, Noueihed B, Omri S, Tahiri H, Chemtob S. Ischemic Retinopathies: oxidative stress and inflammation. Oxid Med Cell Longev. 2017;2017:3940241.
Su Y, Liu XM, Sun YM, Jin HB, Fu R, Wang YY, et al. The relationship between endothelial dysfunction and oxidative stress in diabetes and prediabetes. Int J Clin Pr. 2008;62:877–82. https://doi.org/10.1111/j.1742-1241.2008.01776.x.
Eliana F, Suwondo P, Makmun LH, Harbuwono DS. AADMA as a marker of endothelial dysfunction in prediabetic women. Acta Med Indones. 2011;43:92–98.
An D, Chung-Wah-Cheong J, Yu DY, Balaratnasingam C. Alpha-smooth muscle actin expression and parafoveal blood flow pathways are altered in preclinical diabetic retinopathy. Invest Ophthalmol Vis Sci. 2022;63:8 https://doi.org/10.1167/iovs.63.5.8.
van Dijk HW, Verbraak FD, Kok PH, Stehouwer M, Garvin MK, Sonka M, et al. Early neurodegeneration in the retina of type 2 diabetic patients. Invest Ophthalmol Vis Sci. 2012;53:2715–9. https://doi.org/10.1167/iovs.11-8997.
van Dijk HW, Verbraak FD, Stehouwer M, Kok PH, Garvin MK, Sonka M, et al. Association of visual function and ganglion cell layer thickness in patients with diabetes mellitus type 1 and no or minimal diabetic retinopathy. Vis Res. 2011;51:224–8. https://doi.org/10.1016/j.visres.2010.08.024.
Şahin M, Şahin A, Kılınç F, Karaalp Ü, Yüksel H, Özkurt ZG, et al. Early detection of macular and peripapillary changes with spectralis optical coherence tomography in patients with prediabetes. Arch Physiol Biochem. 2018;124:75–79. https://doi.org/10.1080/13813455.2017.1361450.
Vujosevic S, Midena E. Retinal layers changes in human preclinical and early clinical diabetic retinopathy support early retinal neuronal and müller cells alterations. J Diabetes Res.2013. https://doi.org/10.1155/2013/905058.
Sachdeva MM. Retinal neurodegeneration in diabetes: an emerging concept in diabetic retinopathy. Curr Diab Rep. 2021;21:65 https://doi.org/10.1007/s11892-021-01428-x.
Campbell JP, Zhang M, Hwang TS, Bailey ST, Wilson DJ, Jia Y, et al. Detailed vascular anatomy of the human retina by projection-resolved optical coherence tomography angiography. Sci Rep. 2017;7:42201 https://doi.org/10.1038/srep42201.
Spaide RF, Klancnik JM, Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:45–50. https://doi.org/10.1001/JAMAOPHTHALMOL.2014.3616.
Spaide RF, Fujimoto JG, Waheed NK. Image artifacts in optical coherence tomography angiography. Retina. 2015;35:2163–80. https://doi.org/10.1097/IAE.0000000000000765.
Yu PK, Mehnert A, Athwal A, Sarunic MV, Yu DY. Use of the retinal vascular histology to validate an optical coherence tomography angiography technique. Transl Vis Sci Technol. 2021;10:29 https://doi.org/10.1167/tvst.10.1.29.
Nakahara T, Hoshino M, Hoshino S, Mori A, Sakamoto K, Ishii K. Structural and functional changes in retinal vasculature induced by retinal ischemia-reperfusion in rats. Exp Eye Res. 2015;135:134–45. https://doi.org/10.1016/j.exer.2015.02.020.
Gómez-Ulla F, Cutrin P, Santos P, Fernandez M, Abraldes M, Abalo-Lojo JM, et al. Age and gender influence on foveal avascular zone in healthy eyes. Exp Eye Res. 2019;189:107856 https://doi.org/10.1016/j.exer.2019.107856.
Author information
Authors and Affiliations
Contributions
All authors report that they meet the current ICMJE criteria for Authorship. DK and CH were responsible for conducting the literature search, extracting and analysing data and drafting the manuscript. NW and SS interpreted the results and critically revised the manuscript. All authors read and agreed with the submission of the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
SS reported receiving financial support from AbbVie, Amgen, Apellis, Bayer, Biogen, Boehringer Ingelheim, Novartis, Eyebiotech, Eyepoint Pharmaceuticals, Janssen Pharmaceuticals, Nova Nordisk, Optos, Ocular Therapeutics, Kriya Therapeutics, OcuTerra, Roche, Stealth Biotherapeutics, Sanofi and is a member of the Eye Editorial Board. All other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kazantzis, D., Holmes, C., Wijesingha, N. et al. Changes in foveal avascular zone parameters in individuals with prediabetes compared to normoglycemic controls: a systematic review and meta-analysis. Eye (2024). https://doi.org/10.1038/s41433-024-03058-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03058-5