Abstract
Background/objective
To test the feasibility of a dry eye disease (DED) symptom stratification algorithm previously established for the general population among patients visiting ophthalmologists.
Subject/methods
This retrospective cross-sectional study was conducted between December 2015 and October 2021 at a university hospital in Japan; participants who underwent a comprehensive DED examination and completed the Japanese version of the Ocular Surface Disease Index (J-OSDI) were included. Patients diagnosed with DED were stratified into seven clusters using a previously established symptom-based stratification algorithm for DED. Characteristics of the patients in stratified clusters were compared.
Results
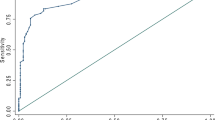
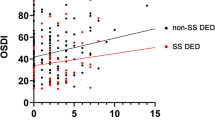
In total, 426 participants were included (median age [interquartile range]; 63 [48–72] years; 357 (83.8%) women). Among them, 291 (68.3%) participants were diagnosed with DED and successfully stratified into seven clusters. The J-OSDI total score was highest in cluster 1 (61.4 [52.2–75.0]), followed by cluster 5 (44.1 [38.8–47.9]). The tear film breakup time was the shortest in cluster 1 (1.5 [1.1–2.1]), followed by cluster 3 (1.6 [1.0–2.5]). The J-OSDI total scores from the stratified clusters in this study and those from the clusters identified in the previous study showed a significant correlation (r = 0.991, P < 0.001).
Conclusions
The patients with DED who visited ophthalmologists were successfully stratified by the previously established algorithm for the general population, uncovering patterns for their seemingly heterogeneous and variable clinical characteristics of DED. The results have important implications for promoting treatment interventions tailored to individual patients and implementing smartphone-based clinical data collection in the future.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data are available in the main text. The code supporting the findings of this study is available from the corresponding author upon reasonable request. Data processing and analysis were performed using STATA version 16.1.
References
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Tsubota K, Yokoi N, Shimazaki J, Watanabe H, Dogru M, Yamada M, et al. New perspectives on Dry eye definition and diagnosis: a consensus report by the asia dry eye society. Ocul Surf. 2017;15:65–76.
Kaido M, Ishida R, Dogru M, Tsubota K. The relation of functional visual acuity measurement methodology to tear functions and ocular surface status. Jpn. J Ophthalmol. 2011;55:451–9.
Belmonte C, Nichols JJ, Cox SM, Brock JA, Begley CG, Bereiter DA, et al. TFOS DEWS II pain and sensation report. Ocul Surf. 2017;15:404–37.
Yamada M, Mizuno Y, Shigeyasu C. Impact of dry eye on work productivity. Clinicoecon Outcomes Res. 2012;4:307–12.
Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15:575–628.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–65.
Inomata T, Shiang T, Iwagami M, Sakemi F, Fujimoto K, Okumura Y, et al. Changes in distribution of dry eye disease by the new 2016 diagnostic criteria from the asia dry eye society. Sci Rep. 2018;8:1918.
Inomata T, Nakamura M, Iwagami M, Shiang T, Yoshimura Y, Fujimoto K, et al. Risk factors for severe dry eye disease: crowdsourced research using DryEyeRhythm. Ophthalmology. 2019;126:766–8.
Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118:615–21.
Midorikawa-Inomata A, Inomata T, Nojiri S, Nakamura M, Iwagami M, Fujimoto K, et al. Reliability and validity of the Japanese version of the ocular surface disease index for dry eye disease. BMJ Open. 2019;9:e033940.
Okumura Y, Inomata T, Iwata N, Sung J, Fujimoto K, Fujio K, et al. A review of dry eye questionnaires: measuring patient-reported outcomes and health-related quality of life. Diagnostics (Basel). 2020;10:559.
Tan G, Li J, Yang Q, Wu A, Qu DY, Wang Y, et al. Air pollutant particulate matter 2.5 induces dry eye syndrome in mice. Sci Rep. 2018;8:17828.
Inomata T, Iwagami M, Nakamura M, Shiang T, Yoshimura Y, Fujimoto K, et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophthalmol. 2020;138:58–68.
Inomata T, Sung J, Nakamura M, Iwagami M, Okumura Y, Iwata N, et al. Using medical big data to develop personalized medicine for dry eye disease. Cornea. 2020;39:S39–S46.
Bradway M, Carrion C, Vallespin B, Saadatfard O, Puigdomènech E, Espallargues M, et al. mHealth assessment: conceptualization of a global framework. JMIR Mhealth Uhealth. 2017;5:e60.
World Health Organization. mHealth: new horizons for health through mobile technologies: second global survey on eHealth. Available at: https://www.who.int/goe/publications/goe_mhealth_web.pdf. Accessed December 6, 2019.
Onnela JP, Rauch SL. Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology. 2016;41:1691–6.
Jain SH, Powers BW, Hawkins JB, Brownstein JS. The digital phenotype. Nat Biotechnol. 2015;33:462–3.
Bottomley A, Jones D, Claassens L. Patient-reported outcomes: assessment and current perspectives of the guidelines of the food and drug administration and the reflection paper of the European medicines agency. Eur J Cancer. 2009;45:347–53.
Weldring T, Smith SM. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:61–68.
Inomata T, Nakamura M, Iwagami M, Midorikawa-Inomata A, Sung J, Fujimoto K, et al. Stratification of individual symptoms of contact lens-associated dry eye using the iPhone app DryEyeRhythm: crowdsourced cross-sectional study. J Med Internet Res. 2020;22:e18996.
Inomata T, Iwagami M, Nakamura M, Shiang T, Fujimoto K, Okumura Y, et al. Association between dry eye and depressive symptoms: Large-scale crowdsourced research using the DryEyeRhythm iPhone application. Ocul Surf. 2020;18:312–9.
Inomata T, Nakamura M, Sung J, Midorikawa-Inomata A, Iwagami M, Fujio K, et al. Smartphone-based digital phenotyping for dry eye toward P4 medicine: a crowdsourced cross-sectional study. NPJ Digit Med. 2021;4:171.
Inomata T, Sung J, Nakamura M, Fujisawa K, Muto K, Ebihara N, et al. New medical big data for P4 medicine on allergic conjunctivitis. Allergol Int. 2020;69:510–8.
Hood L, Friend SH. Predictive, personalized, preventive, participatory (P4) cancer medicine. Nat Rev Clin Oncol. 2011;8:184–7.
Hirosawa K, Inomata T, Sung J, Nakamura M, Okumura Y, Midorikawa-Inomata A, et al. Diagnostic ability of maximum blink interval together with Japanese version of ocular surface disease index score for dry eye disease. Sci Rep. 2020;10:18106.
van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol. 1969;82:10–14.
Inomata T, Iwagami M, Hiratsuka Y, Fujimoto K, Okumura Y, Shiang T, et al. Maximum blink interval is associated with tear film breakup time: a new simple, screening test for dry eye disease. Sci Rep. 2018;8:13443.
Healthcare Engineering Association of Japan Standard Working Group. The guideline for design and operation of hospital HVAC systems: healthcare engineering association of Japan. 2013.
von Luxburg U. A tutorial on spectral clustering. Stat Comput. 2007;17:395–416.
McInnes L, Healy J. UMAP uniform manifold approximation and projection for dimension reduction. ArXiv 2018; https://doi.org/10.48550/arXiv.1802.03426
Tsubota K, Yokoi N, Watanabe H, Dogru M, Kojima T, Yamada M, et al. A new perspective on dry eye classification: proposal by the asia dry eye society. Eye Contact Lens. 2020;46:S2–s13.
Vehof J, Sillevis Smitt-Kamminga N, Nibourg SA, Hammond CJ. Predictors of discordance between symptoms and signs in dry eye disease. Ophthalmology. 2017;124:280–6.
Galor A, Zlotcavitch L, Walter SD, Felix ER, Feuer W, Martin ER, et al. Dry eye symptom severity and persistence are associated with symptoms of neuropathic pain. Br J Ophthalmol. 2015;99:665–8.
Woolf CJ, Safieh-Garabedian B, Ma QP, Crilly P, Winter J. Nerve growth factor contributes to the generation of inflammatory sensory hypersensitivity. Neuroscience. 1994;62:327–31.
Benitez-Del-Castillo JM, Acosta MC, Wassfi MA, Diaz-Valle D, Gegundez JA, Fernandez C, et al. Relation between corneal innervation with confocal microscopy and corneal sensitivity with noncontact esthesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48:173–81.
Yokoi N, Uchino M, Uchino Y, Dogru M, Kawashima M, Komuro A, et al. Importance of tear film instability in dry eye disease in office workers using visual display terminals: the Osaka study. Am J Ophthalmol. 2015;159:748–54.
Tagawa Y, Noda K, Ohguchi T, Tagawa Y, Ishida S, Kitaichi N. Corneal hyperalgesia in patients with short tear film break-up time dry eye. Ocul Surf. 2019;17:55–59.
Acknowledgements
We thank OHAKO, Inc. (Tokyo, Japan) and Medical Logue, Inc. (Tokyo, Japan) for developing the DryEyeRhythm application, and Shiang T, Yoshimura Y, Hirastuka Y, Hori S, Uchino M, and Tsubota K for the initial development of the application.
Funding
This research was supported by JST COI Grant Number JPMJCER02WD02 (TI), JSPS KAKENHI Grant Numbers 20KK0207 (TI), 20K23168 (AMI), 21K17311 (AMI), 21K20998 (AE), and 22K16983 (AE), Kondou Kinen Medical Foundation, Medical Research Encouragement Prize 2020 (TI), Charitable Trust Fund for Ophthalmic Research in Commemoration of Santen Pharmaceutical’s Founder 2020 (TI), Nishikawa Medical Foundation, Medical Research Encouragement Prize 2020 (TI), and the OTC Self- Medication Promotion Foundation (YO). The sponsors had no role in the design or performance of the study, in data collection and management, in the analysis and interpretation of the data, in the preparation, review, approval of the manuscript, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
KN was responsible for methodology, data curation, software, visualization, formal analysis, investigation, writing-original draft preparation, and writing-reviewing and editing. TI was responsible for conceptualization, methodology, validation, investigation, writing-original draft preparation, and writing-reviewing and editing. MN was responsible for software, visualization, formal analysis, investigation, and writing-reviewing and editing. JS conducted the investigation and wrote the original draft, and reviewed and edited the manuscript. AMI performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. MI performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. KF performed data curation, validation, investigation, writing-original draft preparation, and writing reviewing and editing. YA performed data curation, validation, investigation, writing-original draft preparation, and writing-reviewing and editing. YO performed data curation, validation, investigation, writing-original draft preparation, and writing-reviewing and editing. TH performed data curation, validation, investigation, writing-original draft preparation, and writing-reviewing and editing. KF performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. AE performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. MM performed data curation, investigation, writing-original draft preparation, and writing-reviewing and editing. SH performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. JZ performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. MK performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. KH performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. YM performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. RD performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. AM performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing. HK performed validation, investigation, writing-original draft preparation, and writing-reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
The DryEyeRhythm app was created using Apple’s ResearchKit (Cupertino, CA, USA) along with OHAKO, Inc. (Tokyo, Japan) and Medical Logue, Inc. (Tokyo, Japan). TI and YO are the owners of InnoJin, Inc, Tokyo, Japan, for developing DryEyeRhythm. TI reported receiving grants from Johnson & Johnson Vision Care, SEED Co., Ltd, Novartis Pharma K.K., and Kowa Company, Ltd. outside the submitted work, as well as personal fees from Santen Pharmaceutical Co., Ltd., and InnoJin, Inc. The remaining authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagino, K., Inomata, T., Nakamura, M. et al. Symptom-based stratification algorithm for heterogeneous symptoms of dry eye disease: a feasibility study. Eye 37, 3484–3491 (2023). https://doi.org/10.1038/s41433-023-02538-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02538-4