Abstract
Objectives
To investigate the safety profile and the surgical outcomes in a large cohort of subjects undergoing early vitrectomy for unexplained fundus-obscuring vitreous haemorrhage (FOVH).
Methods
Retrospective, single-centre case series of 186 consecutive eyes presenting between January 2018 and February 2020. Primary outcomes included change in best-corrected visual acuity (BCVA), rate of intra-operative retinal tears or retinal detachment (RD), baseline proliferative vitreoretinopathy (PVR), association of demographics with clinical outcomes, and rate of significant adverse events characterised by reoperation.
Results
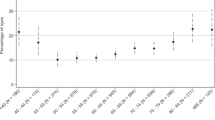
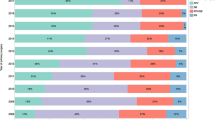
Main final diagnosis was haemorrhagic posterior vitreous detachment (76%) and the overall risk of a retinal tear with or without RD found at the time of surgery was 69%. Vitrectomy was completed within 24 h in 94% of eyes. Rate of RD was 18%; all cases were macula-sparing with no PVR. Mean change in BCVA from baseline to final follow-up was −1.53 ± 0.69 LogMAR, p < 0.001. Time from presentation to surgery was significantly associated with final BCVA (p = 0.036, beta co-efficient 0.097). There was a significant association between presence of RD and age <60 y (OR 0.94, 95%CI [0.90–0.98], p = 0.003). 4.8% required repeated vitrectomy for post-operative RD (4), epiretinal membrane formation (3), removal of oil (1), and recurrent FOVH (1). None of these reoperations were induced by complications during the first surgery.
Conclusion
There is a high rate of retinal breaks in cases with unexplained FOVH, and the risk of a concomitant RD is higher in younger subjects. Early vitrectomy within 24 h appears a safe first-line treatment and yields good clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author and approval by the Clinical Audit Committee. The data are not publicly available due to them containing information that could compromise research participant privacy.
References
Lean JS, Gregor Z. The acute vitreous haemorrhage. Br J Ophthalmol. 1980;64:469–71. https://doi.org/10.1136/bjo.64.7.469.
Sharma S, Walker R, Brown GC, Cruess AF. The importance of qualitative vitreous examination in patients with acute posterior vitreous detachment. Arch Ophthalmol. 1999;117:343–6. https://doi.org/10.1001/archopht.117.3.343.
Sarrafizadeh R, Hassan TS, Ruby AJ, Williams GA, Garreston BR, Capone A Jr. et al. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundusobscuring vitreous hemorrhage. Ophthalmology. 2001;108:2273–8. https://doi.org/10.1016/s0161-6420(01)00822-3.
Tan HS, Mura M, Bijl HM. Early vitrectomy for vitreous hemorrhage associated with retinal tears. Am J Ophthalmol. 2010;150:529–33. https://doi.org/10.1016/j.ajo.2010.04.005.
Dhingra N, Pearce I, Wong D. Early vitrectomy for fundus-obscuring dense vitreous haemorrhage from presumptive retinal tears. Graefes Arch Clin Exp Ophthalmol. 2007;245:301–4. https://doi.org/10.1007/s00417-006-0278-6.
Jaffe NS. Complications of acute posterior vitreous detachment. Arch Ophthalmol. 1968;79:568–71. https://doi.org/10.1001/archopht.1968.03850040570012.
Parchand S, Singh R, Bhalekar S. Reliability of ocular ultrasonography findings for pre-surgical evaluation in various vitreo-retinal disorders. Semin Ophthalmol. 2014;29:236–41. https://doi.org/10.3109/08820538.
Nischal KK, James JN, Mc Allister J. The use of dynamic ultrasound b-scan to detect retinal tears in spontaneous vitreous haemorrhage. Eye. 1995;9:502–6. https://doi.org/10.1038/eye.1995.115.
Jalkh AE, Avila MP, El Markabi H, Trempe CL, Schepens CL. Immersion A- and B-scan ultrasonography. Its use in preoperative evaluation of diabetic vitreous hemorrhage. Arch Ophthalmol. 1984;102:686–90. https://doi.org/10.1001/archopht.1984.01040030542012.
Lorenzo-Carrero J, Perez-Flores I, Cid-Galano M, Fernandez-Fernandez M, Heras-Raposo F, Vazquez-Nuñez R, et al. B-Scan Ultrasonography to Screen for Retinal Tears in Acute Symptomatic Age-Related Posterior Vitreous Detachment. Ophthalmology . 2009;116:94–9. https://doi.org/10.1016/j.ophtha.2008.08.040.
Tseng W, Cortez RT, Ramirez G, Stinnett S, Jaffe GJ. Prevalence and risk factors for proliferative vitreoretinopathy in eyes with rhegmatogenous retinal detachment but no previous vitreoretinal surgery. Am J Ophthalmol. 2004;137:1105–15. https://doi.org/10.1016/j.ajo.2004.02.008.
Duquesne N, Bonnet M, Adeleine P. Preoperative vitreous hemorrhage associated with rhegmatogenous retinal detachment: A risk factor for postoperative proliferative vitreoretinopathy?. Graefes Arch Clin Exp Ophthalmol. 1996;234:677–82. https://doi.org/10.1007/BF00292353.
Cowley M, Conway BP, Campochiaro PA, Kaiser D, Gaskin H. Clinical risk factors for proliferative vitreoretinopathy. Arch Ophthalmol. 1989;107:1147–51. https://doi.org/10.1001/archopht.1989.01070020213027.
Davis M. Natural history of retinal breaks without detachment. Arch Ophthalmol. 1974;92:183–94. https://doi.org/10.1001/archopht.1974.01010010191001.
Morse PH, Aminlari A, Scheie HG. Spontaneous vitreous hemorrhage. Arch Ophthalmol. 1974;92:297–8. https://doi.org/10.1001/archopht.1974.01010010307006.
Winslow RL, Taylor BC. Spontaneous vitreous hemorrhage: etiology and management. South Med J. 1980;73:1450–2. https://doi.org/10.1097/00007611-198011000-00009.
Lindgren G, Sjödell L, Lindblom B. A prospective study of dense spontaneous vitreous hemorrhage. Am J Ophthalmol. 1995;119:458–65. https://doi.org/10.1016/s0002-9394(14)71232-2.
Colyear BH Jr, Pischel DK. Preventive treatment of retinal detachment by means of light coagulation. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1960;41:193–217.
Davis MD. The natural history of retinal breaks without detachment. Trans Am Ophthalmol Soc. 1973;71:343–72.
Melamud A, Pham H, Stoumbos Z. Early Vitrectomy for Spontaneous, Fundus-Obscuring Vitreous Hemorrhage. Am J Ophthalmol. 2015;160:1073–7. https://doi.org/10.1016/j.ajo.2015.07.025.
Ziemianski MC, McMeel JW, Franks EP. Natural history of vitreous hemorrhage in diabetic retinopathy. Ophthalmology. 1980;87:306–12. https://doi.org/10.1016/s0161-6420(80)35232-9.
Rabinowitz R, Yagev R, Shoham A, Lifshitz T. Comparison between clinical and ultrasound findings in patients with vitreous hemorrhage. Eye. 2004;18:253–6. https://doi.org/10.1038/sj.eye.6700632.
Yeung L, Yang KJ, Chen TL, Wang NK, Chen YP, Wan CK., et al. Association between severity of vitreous haemorrhage and visual outcome in primary rhegmatogenous retinal detachment. Acta Ophthalmol. 2008;86:165–9. https://doi.org/10.1111/j.1600-0420.2007.01053.x.
DiBernardo C, Blodi B, Byrne SF. Echographic evaluation of retinal tears in patients with spontaneous vitreous hemorrhage. Arch Ophthalmol. 1992;110:511–4. https://doi.org/10.1001/archopht.1992.01080160089038.
Chen G, Tzekov R, Wensheng L, Jiang F, Mao S, Tong Y. INCIDENCE OF ENDOPHTHALMITIS AFTER VITRECTOMY: A Systematic Review and Meta-analysis. Retina. 2019;39:844–52. https://doi.org/10.1097/IAE.0000000000002055.
Tabandeh H, Flynn HW Jr. Suprachoroidal hemorrhage during pars plana vitrectomy. Curr Opin Ophthalmol. 2001;12:179–85. https://doi.org/10.1097/00055735-200106000-00006.
Chandra A, Xing W, Kadhim MR, Williamson TH. Suprachoroidal hemorrhage in pars plana vitrectomy: risk factors and outcomes over 10 years. Ophthalmology. 2014;121:311–7. https://doi.org/10.1016/j.ophtha.2013.06.021.
Jalil A, Ho WO, Stephen C, Dhawahir-Scala F, Patton N. Iatrogenic retinal breaks in 20-G versus 23-G pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2013;251:1463–7. https://doi.org/10.1007/s00417-013-2299-2.
Heimann H, Zou X, Jandeck C, Kellner U, Bechrakis NE, Kreusel KM, et al. Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006;244:69–78. https://doi.org/10.1007/s00417-005-0026-3.
Williamson TH, Shunmugam M, Rodrigues I, Dogramaci M, Lee E. Characteristics of rhegmatogenous retinal detachment and their relationship to visual outcome. Eye. 2013;27:1063–9. https://doi.org/10.1038/eye.2013.136.
Girard P, Mimoun G, Karpouzas I, Montefiore G. Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. Retina. 1994;14:417–24. https://doi.org/10.1097/00006982-199414050-00005.
Asaria RH, Kon CH, Bunce C, Charteris DG, Wong D, Luthert PJ, et al. How to predict proliferative vitreoretinopathy: a prospective study. Ophthalmology. 2001;108:1184–6. https://doi.org/10.1016/s0161-6420(01)00553-x.
Zhang T, Zhang J, Sun X, Tian J, Shi W, Yuan G. Early vitrectomy for dense vitreous hemorrhage in adults with non-traumatic and non-diabetic retinopathy. J Int Med Res. 2017;45:2065–71. https://doi.org/10.1177/0300060517708942.
Tsukahara M, Mori K, Gehlbach PL, Mori K. Posterior Vitreous Detachment as Observed by Wide-Angle OCT Imaging. Ophthalmology. 2018;125:1372–83. https://doi.org/10.1016/j.ophtha.2018.02.039.
National Cost Collection for the NHS 2020/21. https://www.england.nhs.uk/costing-in-the-nhs/national-cost-collection/#ncc1819.
Author information
Authors and Affiliations
Contributions
PS: Acquired data. BFS: Acquired data; designed the work; drafted and revised the manuscript. EB: performed statistical analysis; performed an important role in interpreting the results. LdC: designed the work; approved the final version of the manuscript; ensured accuracy and integrity of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flores-Sánchez, B.C., Bloch, E., Sanghi, P. et al. Safety profile and surgical outcomes of early vitrectomy in eyes with unexplained fundus-obscuring vitreous haemorrhage. Eye 37, 3191–3196 (2023). https://doi.org/10.1038/s41433-023-02475-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02475-2
This article is cited by
-
Literature- and Experience-Based Consensus for Acute Post-operative Endophthalmitis and Endogenous Endophthalmitis in Taiwan
Ophthalmology and Therapy (2024)