Abstract
Background
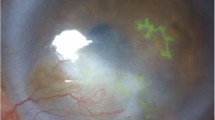
Herpes simplex keratitis (HSK) is the most common but serious infectious keratitis with high recurrence. It is predominantly caused by herpes simplex virus type 1 (HSV-1). The spread mechanism of HSV-1 in HSK is not entirely clear. Multiple publications indicate that exosomes participate in the intercellular communication process during viral infections. However, there is rare evidence that HSV-1 spreads in HSK by exosomal pathway. This study aims to investigate the relationship between the spread of HSV-1 and tear exosomes in recurrent HSK.
Methods
Tear fluids collected from total 59 participants were included in this study. Tear exosomes were isolated by ultracentrifugation, then identified by silver staining and western blot. The size was determined by dynamic light scattering (DLS). The viral biomarkers were identified by western blot. The cellular uptake of exosomes was studied using labelled exosomes.
Results
Tear exosomes were indeed enriched in tear fluids. Collected exosomes own normal diameters consistent with related reports. The exosomal biomarkers existed in tear exosomes. Labelled exosomes were successfully taken up by human corneal epithelial cells (HCEC) in large numbers in a short time. After cellular uptake, HSK biomarkers were detectable by western blot in infected cells.
Conclusions
Tear exosomes should be the latent sites of HSV-1 in recurrent HSK and might be involved in the spread of HSV-1. Besides, this study verifies HSV-1 genes can be indeed transferred between cells by exosomal pathway, providing new inspiration for the clinical intervention and treatment as well as the drug discovery of recurrent HSK.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57:448–62.
Thomas J, Liesegang M. Epidemiology of ocular herpes simplex. Arch Opthalmol. 1989;107:1160–5.
Cabrera-Aguas M, Khoo P, George CRR, Lahra MM, Watson SL. Predisposing factors, microbiological features and outcomes of patients with clinical presumed concomitant microbial and herpes simplex keratitis. Eye 2022;36:86–94.
Kaye S, Choudhary A. Herpes simplex keratitis. Prog Retin Eye Res. 2006;25:355–80.
Morishige N, Jester JV, Naito J, Osorio N, Wahlert A, Jones C, et al. Herpes simplex virus type 1 ICP0 localizes in the stromal layer of infected rabbit corneas and resides predominantly in the cytoplasm and/or perinuclear region of rabbit keratocytes. J Gen Virol. 2006;87:2817–25.
Sibley D, Larkin DFP. Update on Herpes simplex keratitis management. Eye 2020;34:2219–26.
Li L, Li Y, Li X, Xia Y, Wang E, Gong D, et al. HSV-1 infection and pathogenesis in the tree shrew eye following corneal inoculation. J Neurovirol. 2020;26:391–403.
Chen Y, Zhi S, Liang P, Zheng Q, Liu M, Zhao Q, et al. Single AAV-Mediated CRISPR-SaCas9 Inhibits HSV-1 Replication by Editing ICP4 in Trigeminal Ganglion Neurons. Mol Ther Methods Clin Dev. 2020;18:33–43.
Karasneh GA, Shukla D. Herpes simplex virus infects most cell types in vitro: clues to its success. Virol J. 2011;8:481.
Bello-Morales R, Praena B, de la Nuez C, Rejas MT, Guerra M, Galan-Ganga M, et al. Role of microvesicles in the spread of herpes simplex virus 1 in oligodendrocytic cells. J Virol. 2018;92:e00088–18.
Knipe DM, Raja P, Lee JS. Clues to mechanisms of herpesviral latent infection and potential cures. PNAS 2015;112:11993–4.
Wilson AC, Mohr I. A cultured affair: HSV latency and reactivation in neurons. Trends Microbiol. 2012;20:604–11.
Polcicova K, Biswas PS, Banerjee K, Wisner TW, Rouse BT, Johnson DC. Herpes keratitis in the absence of anterograde transport of virus from sensory ganglia to the cornea. PNAS 2005;102:11462–7.
Dua H. Herpes simplex virus in the human cornea. Br J Ophthalmol. 2000;84:559–61.
Anderson MR, Kashanchi F, Jacobson S. Exosomes in viral disease. Neurotherapeutics 2016;13:535–46.
Nomura S, Taniura T, Ito T. Extracellular vesicle-related thrombosis in viral infection. Int J Gen Med. 2020;13:559–68.
Turner DL, Korneev DV, Purdy JG, de Marco A, Mathias RA. The host exosome pathway underpins biogenesis of the human cytomegalovirus virion. Elife 2020;9:e58288.
Patters BJ, Kumar S. The role of exosomal transport of viral agents in persistent HIV pathogenesis. Retrovirology 2018;15:79.
Sadeghipour S, Mathias RA. Herpesviruses hijack host exosomes for viral pathogenesis. Semin Cell Dev Biol. 2017;67:91–100.
Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature 2015;523:177–82.
Aqrawi LA, Galtung HK, Vestad B, Ovstebo R, Thiede B, Rusthen S, et al. Identification of potential saliva and tear biomarkers in primary Sjogren’s syndrome, utilising the extraction of extracellular vesicles and proteomics analysis. Arthritis Res Ther. 2017;19:14.
Wan JCM, Massie C, Garcia-Corbacho J, Mouliere F, Brenton JD, Caldas C, et al. Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 2017;17:223–38.
Zhu S, Huang H, Liu D, Wen S, Shen L, Lin Q. Augmented cellular uptake and homologous targeting of exosome-based drug loaded IOL for posterior capsular opacification prevention and biosafety improvement. Bioact Mater. 2022;15:469–81.
Zhang Y, Liu Y, Liu H, Tang WH. Exosomes: Biogenesis, biologic function and clinical potential. Cell Biosci. 2019;9:19.
Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic Mark M, et al. Tumour exosome integrins determine organotropic metastasis. Nature 2015;527:329–35.
Li SP, Lin ZX, Jiang XY, Yu XY. Exosomal cargo-loading and synthetic exosome-mimics as potential therapeutic tools. Acta Pharm Sin. 2018;39:542–51.
He C, Zheng S, Luo Y, Wang B. Exosome theranostics: biology and translational medicine. Theranostics 2018;8:237–55.
Bang C, Thum T. Exosomes: new players in cell-cell communication. Int J Biochem Cell Biol. 2012;44:2060–4.
Jarmalavičiūtė A, Pivoriūnas A. Exosomes as a potential novel therapeutic tools against neurodegenerative diseases. Pharm Res. 2016;113:816–22.
Borowiec BM, Angelova Volponi A, Mozdziak P, Kempisty B, Dyszkiewicz-Konwinska M. Small extracellular vesicles and COVID19-using the “trojan horse” to tackle the giant. Cells 2021;10:3383.
Bello-Morales R, Ripa I, Lopez-Guerrero JA. Extracellular vesicles in viral spread and antiviral response. Viruses 2020;12:623.
Dreux M, Garaigorta U, Boyd B, Decembre E, Chung J, Whitten-Bauer C, et al. Short-range exosomal transfer of viral RNA from infected cells to plasmacytoid dendritic cells triggers innate immunity. Cell Host Microbe. 2012;12:558–70.
Kalamvoki M, Deschamps T. Extracellular vesicles during herpes simplex virus type 1 infection: an inquire. Virol J. 2016;13:63.
Schorey JS, Cheng Y, Singh PP, Smith VL. Exosomes and other extracellular vesicles in host-pathogen interactions. EMBO Rep. 2015;16:24–43.
Roucourt B, Meeussen S, Bao J, Zimmermann P, David G. Heparanase activates the syndecan-syntenin-ALIX exosome pathway. Cell Res. 2015;25:412–28.
Inubushi S, Kawaguchi H, Mizumoto S, Kunihisa T, Baba M, Kitayama Y, et al. Oncogenic miRNAs Identified in Tear Exosomes From Metastatic Breast Cancer Patients. Anticancer Res. 2020;40:3091–6.
Gurung S, Perocheau D, Touramanidou L, Baruteau J. The exosome journey: from biogenesis to uptake and intracellular signalling. Cell Commun Signal. 2021;19:47.
Funding
This work was financially supported by the Science & Technology Program of Wenzhou (Y20190169, Y2020204), Department of Health of Zhejiang Province (2022KY216).
Author information
Authors and Affiliations
Contributions
HH contributed to experiments design and performance, data analysis and interpretation, and the original draft writing; SL and XZ contributed to sample collection; PZ and QJ contributed to sample preparation; HM contributed to participant recruitments and sample collection; QL contributed to resources, supervision, writing reviewing and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, H., Liu, S., Zhao, X. et al. Role of tear exosomes in the spread of herpes simplex virus type 1 in recurrent herpes simplex keratitis. Eye 37, 3180–3185 (2023). https://doi.org/10.1038/s41433-023-02473-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02473-4