Abstract
Introduction
Dry eye and its related symptoms are the most common causes of referrals to the ophthalmology centers. Since people with dry eye may suffer from different levels of the disease severity, this study aimed to develop a clinical decision support system for diagnosing and determining severity of dry eye disease.
Methods
This research was carried out in two phases in 2020. In the first phase, a questionnaire was designed to identify the most important diagnostic parameters from the cornea specialists’ perspectives (n = 37). In the second phase of the research, a clinical decision support system was designed and implemented by using MATLAB software. Finally, the system was evaluated using patient data which were collected in a teaching hospital (n = 50).
Results
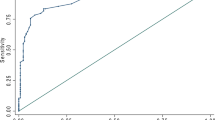
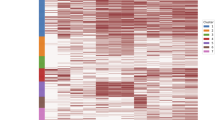
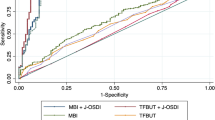
The diagnostic parameters for dry eye disease were filamentary keratitis, meibomian gland dysfunction, score of ocular surface disease index, Schirmer’s test result, tear meniscus height, tear breakup time, and fluorescein staining score. The system output variables were the diagnosis and severity of dry eye disease at four levels for the right and left eyes, separately. The results of the evaluation study showed that the accuracy, sensitivity and specificity of the system were 96.9%, 97.5%, and 93.7%, respectively.
Conclusion
It seems that the system designed in this study can help ophthalmologists to diagnose dry eye disease more accurately and quickly. However, it is recommended to conduct more evaluation studies and include more patients in the future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article.
References
Baudouin C, Aragona P, Van Setten G, Rolando M, Irkeç M, del Castillo JB, et al. Diagnosing the severity of dry eye: a clear and practical algorithm. Br J Ophthalmol. 2014;98:1168–76.
Alshamrani AA, Almousa AS, Almulhim AA, Alafaleq AA, Alosaimi MB, Alqahtani AM, et al. Prevalence and risk factors of dry eye symptoms in a Saudi Arabian population. Middle East Afr J Ophthalmol. 2017;24:67–73.
Sahibi-Nasab S. Prevalence of dry eye in the students of Iran University of Medical Sciences [MSc thesis]. Tehran: Iran University of Medical Sciences; 2018.
Song P, Xia W, Wang M, Chang X, Wang J, Jin S, et al. Variations of dry eye disease prevalence by age, sex and geographic characteristics in China: A systematic review and meta-analysis. J Glob Health. 2018;8:1–10.
Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112:71–82.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
García-Resúa C, Fernández MJG, Penedo MFG, Calvo D, Penas M, Yebra-Pimentel E. New software application for clarifying tear film lipid layer patterns. Cornea. 2013;32:538–46.
Khoshzaban F, Haji-Ali-Nili N, Jabarvand M, Karimi M, Rahimi R, Aliasl J, et al. Review of dry eye disease and its treatment in Iranian traditional medicine. Hist Med J. 2016;8:29–46.
Javadi M-A, Feizi S, Fatehi M. Dry eye syndrome. Bina J Ophthalmol. 2011;6:60–77.
Rezayi S. Dry eye syndrome (DES)/keratoconjunctivitis sicca (KCS). Ophthalmic Nurse. 2015;5:4–6.
Lemp MA, Foulks GN. The definition and classification of dry eye disease. Ocul Surf. 2007;5:75–92.
Mohamadi F, Tahvildari M. Quality of life in dry eye syndrome. Ophthalmic Nurse. 2015;5:14–7.
Pflugfelder SC, Geerling G, Kinoshita S, Lemp MA, McCulley JP, Nelson D, et al. Management and therapy of dry eye disease: report of the management and therapy subcommittee of the international dry eye workshop (2007). Ocul Surf. 2007;5:163–78.
Behrens A, Doyle JJ, Stern L, Chuck RS, McDonnell PJ, Azar DT, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006;25:900–7.
Vaghela C, Bhatt N, Mistry D. A survey on various classification techniques for clinical decision support system. Int J Comput Appl. 2015;116:14–7.
Akbar S, Akram MU, Sharif M, Tariq A, Ullah Yasin U. Decision support system for detection of papilledema through fundus retinal images. J Med Syst. 2017;41:41–66.
Torre-Díez I, Martínez-Pérez B, López-Coronado M, Díaz JR, López MM. Decision support systems and applications in ophthalmology: Literature and commercial review focused on mobile apps. J Med Syst. 2015;39:174–84.
Hashemi H, Khabazkhoob M, Kheirkhah A, Emamian MH, Mehravaran S, Shariati M, et al. Prevalence of dry eye syndrome in an adult population. Clin Exp Ophthalmol. 2014;42:242–8.
Yaqubi G, Shokouhi RS, Hoshyar H, Bayat S, Mohammadzadeh A. The prevalence of dry eye among attendant of Birjand valiaser hospital from 2009-2010. Bina J Ophthalmol. 2012;17:345–50.
Rodriguez JD, Lane KJ, Ousler GW, Angjeli E, Smith LM, Abelson MB. Automated grading system for evaluation of superficial punctate keratitis associated with dry eye. Cornea. 2015;56:2340–7.
Shimazaki J. Definition and diagnostic criteria of dry eye disease: historical overview and future directions. Investig Ophthalmol Vis Sci. 2018;59:7–12.
Barber L, Khodai O, Croley T, Lievens C, Montaquila S, Ziemanski J, et al. Dry eye symptoms and impact on vision-related function across International task force guidelines severity levels in the United States. BMC Ophthalmol. 2018;18:260–9.
Yazdani-ibn-Taz MK, Han MM, Jonuscheit S, Collier A, Nally JE, Hagan S. Patient-reported severity of dry eye and quality of life in diabetes. Clin Ophthalmol. 2019;13:217–24.
Bahmani-Kashkouli M, Alemzadeh SA, Aghaei H, Pakdel F, Abdolalizadeh P, Ghazizadeh M, et al. Subjective versus objective dry eye disease in patients with moderate-severe thyroid eye disease. Ocul Surf. 2018;16:458–62.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276–82.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Casp J Intern Med. 2013;4:627–35.
Savini G, Prabhawasat P, Kojima T, Grueterich M, Espana E, Goto E. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008;2:31–55.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–74.
Tsubota K, Yokoi N, Watanabe H, Dogru M, Kojima T, Yamada M, et al. A new perspective on dry eye classification: proposal by the Asia dry eye society. Eye Contact Lens. 2020;46:2–13.
Akpek EK, Amescua G, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK, et al. Dry eye syndrome preferred practice pattern. Ophthalmology. 2019;126:286–334.
Sullivan BD, Whitmer D, Nichols KK, Tomlinson A, Foulks GN, Geerling G, et al. An objective approach to dry eye disease severity. Investig Ophthalmol Vis Sci. 2010;51:6125–30.
Remeseiro B, Barreira N, García-Resúa C, Lira M, Giráldez MJ, Yebra-Pimentel E, et al. IDEAS: a web-based system for dry eye assessment. Comput Methods Prog Biomed. 2016;130:186–97.
López MM, López MM, de la Torre Díez I, Jimeno JCP, López-Coronado M. A mobile decision support system for red eye diseases diagnosis: experience with medical students. J Med Syst. 2016;40:151.
Salem BR, Solodovnikov VI. Decision support system for an early-stage Keratoconus diagnosis. J Phys Conf Ser. 2019;1419:012023.
Giannaccare G, Pellegrini M, Sebastiani S, Moscardelli F, Versura P, Campos EC. In vivo confocal microscopy morphometric analysis of corneal subbasal nerve plexus in dry eye disease using newly developed fully automated system. Graefes Arch Clin Exp Ophthalmol. 2019;257:583–9.
Remeseiro B, Mosquera A, Penedo MG. CASDES: a computer-aided system to support dry eye diagnosis based on tear film maps. IEEE J Biomed Health Inform. 2015;20:936–43.
Funding
This study was funded and supported by Iran University of Medical Sciences, Tehran, Iran (IUMS/SHMIS_98-4-37-17170).
Author information
Authors and Affiliations
Contributions
FE and HA (2nd author) conceptualized and designed the study. FE also prepared the first draft of the paper. HA (2nd author) supervised the study and commented on the paper. HA (3rd author) helped with conducting the study and commented on the paper. All authors have read and approved the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ebrahimi, F., Ayatollahi, H. & Aghaei, H. A clinical decision support system for diagnosing and determining severity of dry eye disease. Eye 37, 1619–1624 (2023). https://doi.org/10.1038/s41433-022-02197-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02197-x