Abstract
Purpose
To review ophthalmic trauma malpractice claims in the Ophthalmic Mutual Insurance Company (OMIC) database to determine the frequency and causes of litigation.
Methods
A retrospective case series analysis of ophthalmic trauma claims from 2009 to 2019 was completed. Cases were selected only if the injury was secondary to trauma (e.g., fall, gunshot wound, paintball injury, etc.); iatrogenic traumatic surgical injuries were excluded.
Results
31 closed cases associated with 40 total claims related to ophthalmic trauma out of 2565 claims (1.56%) in the OMIC database were analysed. 13 of the 31 cases (41.9%) were decided for the plaintiff. In decisions for the plaintiff, the median settlement amount was $330,000 (range $125,000–$1,000,000). The most frequent initial diagnoses were corneal abrasion (n = 10), hyphema (n = 5) and open-globe injury (n = 5), and the most common final diagnoses were endophthalmitis (n = 8), intraocular foreign body (n = 7) and retinal detachment (n = 7). The most common causes of malpractice litigation were a delay in referral or follow-up (n = 11) and failure to get appropriate imaging (n = 8). In the 13 cases decided for the plaintiff, experts concluded nine did not meet standard of care.
Conclusions
Ophthalmic trauma malpractice claims are very uncommon in the United States, however, the payout is higher than non-trauma settlements, and approximately 40% of cases were decided for the plaintiff. Care could be improved with a careful history and complete ophthalmic examination (with dilated fundoscopy), imaging in appropriate patients, meticulous documentation, and early sub-specialist referral when the diagnosis or management plan was unclear.
Similar content being viewed by others
Introduction
From 2006–2011, there were 11,929,955 emergency department (ED) visits in the United States related to ophthalmic complaints [1]. In 2010, eye-related visits represented approximately 1.5% of all visits to the ED [2]. A recent Eyenet article reported that EDs across the country are struggling to maintain ophthalmology coverage [3]. Indeed, in rural regions of California in 2014, ophthalmology coverage in emergency departments was often less than 50% [4] and in Florida in 2020, only approximately 7% of rural hospitals had an ophthalmologist available on call [5]. It should not go unnoticed that in regions without ophthalmology coverage in the ED, there is a growing interest from the optometric community to expand their scope of practice by seeking hospital privileges in order to provide ED coverage for ocular injuries [6]. The increased use of ambulatory surgical centers, unfamiliar or poorly maintained ophthalmic equipment in the ED, and growth of sub-specialization in ophthalmology are frequently cited for the lack of ophthalmologists participating in ED call [3], however, poor reimbursement and liability concerns also contribute to this decreased interest in call coverage [7, 8].
Annually, roughly 7.5% of all physicians will face a malpractice lawsuit [9]. Ophthalmologists, historically, have had fewer claims than the average physician and lower rates of payments per claim [10, 11]. But even in low-risk specialties such as ophthalmology, approximately 5% of ophthalmologists will be named in a malpractice suit by age 45, and 19% by age 65 [9]. The Ophthalmic Mutual Insurance Company (OMIC) database contains all the professional liability claims brought against OMIC-insured physicians and was used in this study to evaluate the number, cause, and payments related to ophthalmic trauma malpractice cases [12, 13]. Until now, the OMIC database has not been evaluated for malpractice claims related to ophthalmic trauma. Our objective was to identify common diagnoses and provider practices that led to claims against OMIC-insured physicians. By educating ophthalmologists on the clinical patterns of ophthalmic trauma related to malpractice claims, this review of claims data aims to improve patient care and prevent future malpractice litigation, and to provide education on the actual frequency and risk of malpractice litigation in ophthalmic trauma in order to encourage trauma call coverage.
Methods
A retrospective analysis of closed trauma-related claims litigated against OMIC-insured ophthalmologists from 2009 to 2019 was completed. A claim is defined as a written notice or demand for money or services, including the institution of a lawsuit or arbitration proceeding; there may be multiple claims per case. Specific claims were identified by one author (A.M.M.) in March 2020 by searching the OMIC database for terms related to ophthalmic trauma: open globe, laceration (corneal, scleral), intraocular foreign body, rupture, penetrating, perforating, firework, chemical burn, thermal burn, abrasion, foreign body (peribulbar, intraorbital, corneal, conjunctival, orbital, periorbital, eyelid, lacrimal), hyphema, microhyphema, iridodialysis, cyclodialysis, laceration (eyelid, eyebrow, canalicular, nasolacrimal), fracture, retrobulbar hemorrhage, retrobulbar hematoma, commotio, choroidal rupture, sclopetaria, traumatic optic neuropathy, and shaken baby syndrome.
Cases were selected only if the injury was secondary to trauma; iatrogenic surgical injuries not related to a repair of an ophthalmic traumatic injury were excluded. The data also excluded open claims. All cases were reviewed independently by A.M.M. and at least two additional co-authors to ensure that the injury was secondary to trauma or repair of a traumatic injury. The claims data summary and litigation files of the defense attorneys for each case were reviewed. Individual patient medical records were not reviewed. The study complied with the Health Insurance Portability and Accountability Act and adhered to the tenets of the Declaration of Helsinki. Institutional review board was not required as data collection was approved through OMIC.
Data collected by the authors included: decision for defendant vs plaintiff, year of claim, plaintiff sex and age, state (location), adherence to the standard of care as assessed by OMIC board and committee members and/or outside defense experts, verdict, means of resolution, and settlement or judgment payment. Initial and final diagnosis in every case were identified; these were the critical diagnoses for the case determined by the co-authors. There could be multiple initial and final diagnoses for each case.
An additional analysis was completed to assess any errors in diagnosis or management, and these were evaluated by two co-authors and A.M.M for each case. Cases were assessed as either (1) correct diagnosis, correct management, (2) correct diagnosis, wrong management, and (3) wrong diagnosis, wrong management. Secondly, all cases were then separately assessed for cause of misdiagnosis or management. There were five categories: (1). Ophthalmologist accepted ED diagnosis and did not see the patient. (2). Proper imaging not ordered. (3). Delay in follow-up or referral. (4). Medical documentation issue. (5). Other. Certain cases were deemed non-applicable for this analysis if the authors felt that there was no diagnosis or management error. Disagreements were discussed and resolved as a group for all data collected.
Results
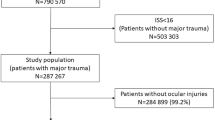
Overall, there were 31 closed cases associated with 40 total claims related to ophthalmic trauma out of 2,565 claims (1.56%) in the OMIC database (Table 1; Supplemental Table 1). Baseline characteristics of patients were recorded (Supplemental Table 2). The median age at time of trauma was 41 years (range 1.5–72). Twenty-six (83.9%) patients were male. Florida (n = 5), Illinois (n = 5) and Massachusetts (n = 3) were the states with the greatest number of cases. The number of decisions for the plaintiff (n = 13) and defendant (n = 18) were analysed (Fig. 1A). All 13 decisions for the plaintiff were pre-trial settlements. The means of resolution for the defendant cases are presented in Fig. 1B. Of the 18 decisions in favor of the defendant, 12 were closed without payment and there were jury verdicts in four. In the two other cases, one was a motion of summary judgment (i.e., a motion was filed in court to have the case decided without a trial in favor of the defendant) and in the other case, an optometrist settled out of court and the OMIC insured ophthalmologist was found to be not liable. In decisions for the plaintiff, the median settlement amount was $330,000 (range $125,000–$1,000,000). The median settlement amount for all OMIC cases during the same time period was $137,500 (range $450–$3,375,000). No jury decisions resulted in a payment.
Case Information
All the cases decided for the plaintiff are summarized in Table 1 and for defendant in Supplemental Table 1. There were a wide variety of mechanisms of injury, but the most common causes of traumatic injury were fall (n = 5) and metal striking metal with intraocular foreign bodies (IOFB) (n = 4). The initial and final diagnoses of the cases were assessed (Fig. 2A, B). For patients initially diagnosed with corneal abrasions (n = 10), they were subsequently diagnosed with IOFB (n = 4), other open globe injuries (n = 2), endophthalmitis (n = 4), and ulcer (n = 3). Patients with a final diagnosis of endophthalmitis (n = 8) were initially diagnosed with open globe injury (n = 2), corneal abrasion (n = 4), vitreous hemorrhage (n = 1) and hyphema (n = 1). Further, in patients with a final diagnosis of IOFB (n = 7), six patients were initially misdiagnosed with either a corneal abrasion (n = 4) or open globe injury (n = 2). Of the injuries, 18 would need final management by a retina specialist, six by a corneal specialist, five by an oculoplastics specialist, and one by a glaucoma specialist.
Initial and final visual acuities were recorded. The initial visual acuity was not available for 12 patients because they were taken in the ED and were not available in the OMIC database. In the cases decided for the plaintiff (n = 13), only one patient had a final visual acuity better than 20/200. Five patients had no light perception (NLP) vision and of these, three underwent enucleation or evisceration. In the cases decided for the defendant (n = 18), nine eyes had a final vision better than 20/200. Of the nine eyes with vision worse than 20/200, five eyes were NLP, and three of these underwent enucleation.
Cause of Malpractice Claims
Upon review of the cases in the OMIC database, certain general trends in malpractice claims were identified and summarized in Table 2. In addition, to further classify the cause of a malpractice claim, an assessment of the diagnosis and management was completed (Fig. 3A). In the majority of cases decided for the defendant (n = 13) there was the correct diagnoses and correct management, while the majority of cases for the plaintiff involved a wrong diagnosis and wrong management (n = 10). The authors also studied the specific cause of the malpractice claim (Fig. 3B). Individual cases could have multiple causes, but the most common were a delay in referral or follow-up (n = 11) and failure to get appropriate imaging (n = 8). In the cases involving a delay in referral or follow-up, the most common subspecialities needing referral were retina (n = 7) and cornea (n = 2). “Other” cases were classified as other due to delay in starting antibiotics (n = 2), failure to order proper laboratory testing (n = 2), poor surgical technique (n = 2), failure to see patient prior to surgery (n = 1), and staff members turning a trauma patient away from clinic (n = 1).
Finally, the evaluations of whether the providers met the standard of care are presented in Fig. 3C. In one case, which was found in favor of the plaintiff, an OMIC expert evaluation was not obtained because the co-defendant was found liable. An expert evaluation was not obtained in approximately half of the cases found in favor of the defendant, because they were closed before expert assessment was obtained. One defendant case was classified as “other” because the expert felt that the insured ophthalmologist had met the standard of care, but the co-defendant optometrist working for the provider had not. Further, in three cases for the defendant and plaintiff each the standard of care decision was “mixed,” i.e., the expert reviewers had differing opinions on the liability.
Discussion
Malpractice claims related to ophthalmic trauma are rare and in the OMIC database represent only 1.56% of claims. Previously reported rates of ophthalmic malpractice cases in the United States are about 4% [14], which is similar to that of about 3% in the UK [11]. In the OMIC database, the median settlement for ophthalmic trauma is roughly $200,000 higher than for other types of ophthalmic malpractice claims, but were similar to the mean compensation payment across multiple other medical specialities [10, 15]. The higher compensation rate is likely due to the frequent severe vision loss associated with ophthalmic trauma [16]. In the United States Eye Injury Registry (USEIR), approximately 25% of ophthalmic injuries result in a final visual acuity of less than 20/200 [17]. In our study, 12 of 13 cases that were ruled in favor of the plaintiff had a final visual outcome of 20/200 or worse and roughly 1/3 of the traumatized eyes had a final vision of NLP. Thus, although malpractice claims related to ophthalmic trauma are not common, the severity of visual loss associated with these injuries, especially if there was mismanagement, often results in larger settlement amounts.
One of the most notable observations of these OMIC trauma-related cases is the initial misdiagnosis of a penetrating eye injury as a corneal abrasion by either an ophthalmologist (6.5%) or a non-ophthalmologist (12.9%). It is important in corneal abrasion injuries to have a high suspicion for an occult open globe injury. Further, a diagnostic error such as this is sometimes compounded when the treating ophthalmologist who follows the patient thereafter does not perform a thorough and complete ophthalmic examination or order appropriate diagnostic imaging. In open globe and IOFB injuries, too often (25.8%) a dilated fundoscopic examination or adjunctive imaging such as B-scan ultrasonography by a trained ophthalmologist, plain film imaging if CT is not available, or computed tomography (CT) of the orbit was not done. When the eye examination is not suggestive of globe rupture, but the mechanism of injury involves metal striking metal or a sharp object striking the globe, there should be strong suspicion for an occult open globe injury and possible IOFB. A previous study has shown that CT scan is the most reliable method for identifying suspected IOFBs when compared to B-scan ultrasonography or clinical eye examination [18]. If vegetable matter is suspected in the wound and a metallic IOFB has been excluded, MRI imaging may also be helpful [19]. CT imaging has a high specificity (approximately 75–100%) but low sensitivity (approximately 40–75%) for identifying open globe injuries. CT findings of changes in globe contour, volume loss, absence of lens, retinal detachment, and vitreous hemorrhage are the most predictive signs of an open globe injury [20,21,22]. However, CT imaging alone cannot be relied upon to diagnose an occult open globe and a comprehensive clinical examination including a dilated fundoscopic examination should be done [20, 21]. Treating ophthalmologists should have a low threshold for surgical evaluation under anesthesia if they are unable to rule out a ruptured globe by clinical examination and imaging [22]. This situation is not uncommon with ocular trauma in children [23].
Patients diagnosed with a traumatic corneal abrasion should be monitored for ulcer formation. In our study there was four cases of corneal ulcer formation (12.9%) and two fungal ulcers (6.5%). One of the fungal cases was mismanaged and resulted in a decision for the plaintiff. This case involved a delay in culturing the ulcer, treating the fungal keratitis, and referral to a corneal specialist. Although in the United States bacterial keratitis is most frequently associated with contact lens use, in South East Asia and South India, trauma is the largest risk factor for microbial keratitis [24,25,26]. In Florida, trauma has been found to be the most common cause of fungal keratitis [27, 28]. Initial daily follow-up and cultures of a corneal ulcer are typically indicated in patients with corneal trauma. Non-healing ulcers should raise concern for fungal infection and early referral to a corneal specialist should be considered [24, 27, 28].
Another striking observation was the frequency (n = 5; 16.1%) of undetected IOFBs resulting in endophthalmitis, siderosis, retinal detachment, and/or proliferative vitreoretinopathy all resulting in decisions for the plaintiff. Mismanagement of these cases resulted in delay of referral to a retinal specialist and removal of the IOFB. It is critical, in ophthalmic trauma, that patients are monitored for pigmentary retinopathy, iris heterochromia, pupillary mydriasis, and cataract development to rule out siderosis [29,30,31]. It should be noted that even when the electroretinogram (ERG) demonstrates decreased b-wave amplitudes in patients with an IOFB, visual acuity and other clinical signs may improve after IOFB removal [29, 31]. In addition, our series had multiple cases (n = 6, 19.4%) of open globe (n = 4) or IOFB-related (n = 2) trauma that developed endophthalmitis. Two cases were related to either failure or delay in prescribing systemic antibiotics. The incidence of endophthalmitis in patients treated with systemic antibiotics after open globe injury is approximately 1–3% [19, 32, 33]. Further- multiple randomized controlled studies have not found a difference in rates of endophthalmitis between intravenous versus oral antibiotics [19, 32, 33]. Patients with an IOFB and delayed wound closure, contaminated wounds, or ruptured lens capsule should raise increased suspicion for endophthalmitis and the treating ophthalmologist should have a lower threshold for referral to a retina specialist [19].
A previous review of malpractice litigation related to oculoplastic surgery found that iatrogenic injury, legal blindness, and cranial nerve injury resulted in a higher likelihood of payment to the plaintiff (p < 0.05) [34]. The five orbital cases in this series represent a unique category of malpractice claims and were either related to injuries sustained during surgical repair of the initial traumatic injury, or due to poorly performed informed consent. Two of the orbital injury cases were decided for the plaintiff. One case involved an optic nerve injury which occurred during orbital fracture repair and the other involved exploration for an intra-orbital foreign body resulting in an iatrogenic open globe. Both cases resulted in a final visual acuity less than 20/200. A third case due to retrobulbar hematoma after orbital fracture repair, which is known to occur after approximately 1% of orbital fracture repairs [35, 36] was decided for the defendant.
The two cases of poor informed consent involved oculoplastics cases. In the above mentioned retrobulbar hematoma after orbital fracture repair case, the written informed consent indicated that the patient should stop the use of aspirin for two weeks prior to surgery and the patient was not verbally advised of the increased risk of hemorrhage of patients on blood-thinning medications. The surgeon waited only three days off aspirin before performing the surgery. In another case involving evisceration for post-traumatic endophthalmitis, the surgeon obtained informed consent from a family member of the injured patient instead of waiting until the patient was able to give consent. These two cases demonstrate the importance of the informed consent process and the crucial role it plays in causing plaintiffs to initiate a claim [34, 37]. OMIC has numerous informed consent documents available on the company’s website for many ophthalmic trauma surgical procedures [38,39,40,41,42].
Poor communication between an optometrist or ED physician and the treating ophthalmologist was another common cause (n = 8, 25.8%) of malpractice claim observed in this study. Half of these cases resulted in a plaintiff decision. With the rise in teleophthalmology for emergency department triage [4, 5], it is even more critical that the on-call ophthalmologist ask the referring provider appropriate questions to determine whether they have made the correct diagnosis, have completed an appropriate examination with suitable imaging, have a proper treatment plan, and have arranged follow-up. The on-call ophthalmologist should have a low threshold for evaluating the patient—in person—regardless of the time of day or night. For example, a pediatric case in this series involving decreased vision with hyphema resulted in NLP vision because the emergency department did not perform an intraocular pressure (IOP) check and the ophthalmologist did not ask whether the patient had a history of sickle cell disease [43, 44]. The patient’s elevated IOP resulted in a secondary central retinal artery occlusion (CRAO) and blindness in the involved eye. It should be noted that depending on state laws, the provider can be held liable for any medical advice given over the phone, and careful documentation of telemedicine consults should be practiced as with all patient encounters [45]. The on-call ophthalmologist may wish to consider using a telemedicine consent in these sitations [46].
If an ophthalmic practice employs optometrists who treat ophthalmic trauma, it is important to observe and discuss trauma cases with them. In two cases, defendants were sued as their employed optometrists mismanaged trauma cases; both of these cases were dismissed for the defendant, but their optometrists settled out of court. Critically, ophthalmologists as supervisors with the highest credentials are at risk for legal action in mismanaged trauma cases by their employees. In addition, the on-call ophthalmologist should give feedback to ED providers if a case of ophthalmic trauma is misdiagnosed or mismanaged. Patients referred from the ED should have close follow-up and office staff should be notified of the patient’s demographic information to track the patient in case they do not present for appointments. One case in this series involved office staff turning away an ED patient who had no insurance because the ophthalmologist had not alerted the staff that the patient was told to come in from the ED. Lastly, it is critical to refer to appropriate ophthalmic subspecialties in complex cases when the diagnosis or management protocol is unclear [45]. Delay in follow-up to the comprehensive ophthalmologist or referral to a subspecialist was an important factor in 11 cases in this study, of which retina was the most common subspecialty with delayed referral (n = 7).
There are limitations to this study. The OMIC database is restricted to claims brought against OMIC insureds which represent approximately 30% of privately insured US ophthalmologists. (There are approximately 18,000 active US ophthalmologists and OMIC insures about 5000, but approximately 8000 are self-insured by their hospital system or covered by federal tort laws as Veterans Affairs providers). Thus, malpractice claims of ophthalmologists with other insurance would not have been identified during this search [47]. Another limitation is that not all data was complete for every case and the authors did not have direct access to the individual patient medical records. Further, we did not look at the ophthalmic subspecialty distribution of different types of suits. Future studies should evaluate the practice patterns of the referring providers to see if subspecialists are more likely to have a case outside of their specialty area. Finally, the small sample size limited any statistical analysis.
Malpractice claims related to ophthalmic trauma are very uncommon in the United States, however, 42% of cases were found for the plaintiff and the settlement payments were higher than for non-trauma cases due to poor visual outcomes. But, if the on-call ophthalmologists had performed a careful history and complete ophthalmic examination (with dilated fundoscopy) and imaging in appropriate patients, the number of cases in this study might have been greatly reduced. Performance of a thorough informed consent, meticulous documentation, and early sub-specialist referrals when the diagnosis or management plan is unclear, are all critical factors in providing excellent patient care and also avoiding a malpractice claim. Finally, as the leaders in the care of ophthalmic trauma, it is critical that ophthalmologists maintain coverage of emergency departments throughout the United States.
Summary
What was known before:
-
Decreasing call coverage- In the United States, there is a decrease in ophthalmologist coverage particularly in rural regions, and liability concerns have been found to be a contributing factor.
-
Ophthalmology is a low-risk subspecialty for malpractice- Ophthalmologists face few claims and have lower payments, however approximately 20% of ophthalmologists will face a lawsuit by 65.
What this study adds:
-
Larger settlement amounts for ophthalmic trauma malpractice- Overall malpractice claims are very low for ophthalmic trauma, but due to the severity of the vision loss in these injuries they result in larger settlement amounts than other ophthalmic fields.
-
Corneal abrasion- corneal abrasion misdiagnosis was a frequent cause of litigation. Frequently, this was due to a missed open globe or intraocular foreign body with subsequent lack of imaging or referral to subspecialist for management.
References
Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134(Mar):312–9.
Vaziri K, Schwartz SG, Flynn HW Jr, Kishor KS, Moshfeghi AA. Eye-related emergency department visits in the United States, 2010. Ophthalmology 2016;123(Apr):917–9.
American Academy of Ophthalmology. Who’s on call? Emergency care crisis looms. https://www.aao.org/eyenet/article/whos-on-call-emergency-care-crisis-looms. 2019. Accessed 10 December 2020
Wedekind L, Sainani K, Pershing S. Supply and perceived demand for teleophthalmology in triage and consultations in California Emergency Departments. JAMA Ophthalmol. 2016;134(May):537–543.
Tauber J, Ayoub S, Shah P, Wu M, Tsui E, Schuman JS et al. Assessing the demand for teleophthalmology in Florida Emergency Departments. Telemed J E Health. 2020 Jun. Epub ahead of print.
American Optometric Association. Why doctors of optometry should seek hospital privileges. https://www.aoa.org/news/practice-management/perfect-your-practice/why-doctors-of-optometry-should-seek-hospital-privileges?sso=y. 2015. Accessed 10 December 2020
American Academy of Ophthalmology. On-call compensation for ophthalmologists. https://www.aao.org/clinical-statement/oncall-compensation-ophthalmologists. 2014. Accessed 10 December 2020
Eyeworld. Ocular Trauma and the uninsured. https://www.eyeworld.org/article-ocular-trauma-and-the-uninsured. 2010. Accessed 10 December 2020
Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N. Engl J Med. 2011;365:629–636.
Thompson AC, Parikh PD, Lad EM. Review of ophthalmology medical professional liability claims in the United States from 2006 through 2015. Ophthalmology 2018;125(May):631–641.
Mathew RG, Ferguson V, Hingorani M. Clinical negligence in ophthalmology: fifteen years of national health service litigation authority data. Ophthalmology 2013;120(Apr):859–64.
Morley M, Menke AM, Nanji KC. Ocular anesthesia-related closed claims from Ophthalmic Mutual Insurance Company 2008–2018. Ophthalmology 2020;127(Jul):852–858.
Wiggins RE Jr, Gold RS, Menke AM. Twenty-five years of professional liability in pediatric ophthalmology and strabismus: the OMIC experience. J AAPOS. 2015;19(Dec):535–40.
Engelhard SB, Salek SS, Justin GA, Sim AJ, Woreta FA, Reddy AK. Malpractice litigation in ophthalmic trauma. Clin Ophthalmol 2020;14(Jul):1979–1986.
Schaffer AC, Jena AB, Seabury SA, Singh H, Chalasani V, Kachalia A. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992–2014. JAMA Intern Med. 2017;177(May):710–718.
Kuhn F, Morris R, Witherspoon CD, Mann L. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol. 2006;13(Jun):209–16.
Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5(Sep):143–69.
Patel SN, Langer PD, Zarbin MA, Bhagat N. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular foreign bodies in open globe injury. Eur J Ophthalmol. 2012;22(Mar-Apr):259–68.
Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW Jr. Endophthalmitis following open-globe injuries. Eye 2012;26(Feb):212–7.
Joseph DP, Pieramici DJ, Beauchamp NJ Jr. Computed tomography in the diagnosis and prognosis of open-globe injuries. Ophthalmology 2000;107(Oct):1899–906.
Arey ML, Mootha VV, Whittemore AR, Chason DP, Blomquist PH. Computed tomography in the diagnosis of occult open-globe injuries. Ophthalmology 2007;114(Aug):1448–52.
Crowell EL, Koduri VA, Supsupin EP, Klinglesmith RE, Chuang AZ, Kim G, et al. Accuracy of computed tomography imaging criteria in the diagnosis of adult open globe injuries by neuroradiology and ophthalmology. Acad Emerg Med. 2017;24(Sep):1072–1079.
Li X, Zarbin MA, Bhagat N. Pediatric open globe injury: a review of the literature. J Emerg Trauma Shock. 2015;8(Oct-Dec):216–23.
Lin A, Rhee MK, Akpek EK, Amescua G, Farid M, Garcia-Ferrer FJ, et al. American Academy of Ophthalmology Preferred Practice Pattern Cornea and External Disease Panel. Bacterial Keratitis Preferred Practice Pattern®. Ophthalmology 2019;126(Jan):P1–P55.
Chidambaram JD, Venkatesh Prajna N, Srikanthi P, Lanjewar S, Shah M, Elakkiya S, et al. Epidemiology, risk factors, and clinical outcomes in severe microbial keratitis in South India. Ophthalmic Epidemiol. 2018;25(Aug):297–305.
Upadhyay MP, Karmacharya PC, Koirala S, Shah DN, Shakya S, Shrestha JK, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol. 2001;85(Apr):388–92.
Rosa RH Jr, Miller D, Alfonso EC. The changing spectrum of fungal keratitis in south Florida. Ophthalmology 1994;101(Jun):1005–13.
Liesegang TJ, Forster RK. Spectrum of microbial keratitis in South Florida. Am J Ophthalmol. 1980;90(Jul):38–47.
Kannan NB, Adenuga OO, Rajan RP, Ramasamy K. Management of ocular siderosis: visual outcome and electroretinographic changes. J Ophthalmol. 2016;2016:7272465.
Zhu L, Shen P, Lu H, Du C, Shen J, Gu Y. Ocular trauma score in Siderosis Bulbi with retained intraocular foreign body. Med (Baltim). 2015;94(Sep):e1533.
Casini G, Sartini F, Loiudice P, Benini G, Menchini M Ocular siderosis: a misdiagnosed cause of visual loss due to ferrous intraocular foreign bodies-epidemiology, pathogenesis, clinical signs, imaging and available treatment options. Doc Ophthalmol. 2020 Sep. Epub ahead of print.
Tabatabaei SA, Soleimani M, Behrooz MJ, Sheibani K. Systemic oral antibiotics as a prophylactic measure to prevent endophthalmitis in patients with open globe injuries in comparison with intravenous antibiotics. Retina 2016;36(Feb):360–5.
Du Toit N, Mustak S, Cook C. Randomised controlled trial of prophylactic antibiotic treatment for the prevention of endophthalmitis after open globe injury at Groote Schuur Hospital. Br J Ophthalmol. 2017;101(Jul):862–867.
Svider PF, Blake DM, Husain Q, Mauro AC, Turbin RE, Eloy JA, et al. In the eyes of the law: malpractice litigation in oculoplastic surgery. Ophthalmic Plast Reconstr Surg. 2014;30(Mar-Apr):119–23.
Shew M, Carlisle MP, Lu GN, Humphrey C, Kriet JD. Surgical treatment of orbital blowout fractures: complications and postoperative care patterns. Craniomaxillofac Trauma Reconstr. 2016;9(Nov):299–304.
Bregman JA, Vakharia KT, Idowu OO, Vagefi MR, Grumbine FL. Outpatient surgical management of orbital blowout fractures. Craniomaxillofac Trauma Reconstr. 2019;12(Sep):205–210.
Lin YK, Liu KT, Chen CW, Lee WC, Lin CJ, Shi L, et al. How to effectively obtain informed consent in trauma patients: a systematic review. BMC Med Ethics. 2019;20(Jan):8.
Ophthalmic Mutual Insurance Company. Open Globe Repair Consent Form. https://www.omic.com/open-globe-repair-consent-form/. 2019. Accessed 11 December 2020.
Ophthalmic Mutual Insurance Company. Orbital Fracture Repair Consent Form. https://www.omic.com/orbital-fracture-repair-consent-form/. 2016. Accessed 11 December 2020
Ophthalmic Mutual Insurance Company. Evisceration/Enucleation Consent Form. https://www.omic.com/eviscerationenucleation-consent-form/. 2016. Accessed 11 December 2020
Ophthalmic Mutual Insurance Company. Anticoagulant consent form. https://www.omic.com/anticoagulant-consent/. 2020. Accessed 11 December 2020.
Ophthalmic Mutual Insurance Company. Refusal of recommended medical or surgical treatment. https://www.omic.com/refusal-of-recommended-medical-or-surgical-procedureintervention/. 2020. Accessed 11 December.
Iftikhar M, Mir T, Seidel N, Rice K, Trang M, Bhowmik R et al. Epidemiology and outcomes of hyphema: a single tertiary centre experience of 180 cases. Acta Ophthalmol. 2020 Oct https://doi.org/10.1111/aos.14603. Epub ahead of print.
SooHoo JR, Davies BW, Braverman RS, Enzenauer RW, McCourt EA. Pediatric traumatic hyphema: a review of 138 consecutive cases. J AAPOS. 2013;17(Dec):565–7.
Colón VF. 10 ways to reduce medical malpractice exposure. Physician Exec 2002;28(Mar-Apr):16–8.
Ophthalmic Mutual Insurance Company. Telemedicine Consent form. https://www.omic.com/telemedicine-consent-form/. 2020. Accessed 11 December 2020
American Academy of Ophthalmology. American Academy of Ophthalmology Renews Partnership with Ophthalmic Mutual Insurance Company. https://www.aao.org/newsroom/news-releases/detail/american-academy-of-ophthalmology-renews-partnersh. 2012. Accessed 10 December 2020
Author information
Authors and Affiliations
Contributions
G.A.J. conceived the work. A.M.M. acquired the data. All authors played an important role in interpreting the results, drafting and revising the manuscript, approving the final version, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
Dr. Pelton is a Board member of Ophthalmic Mutual Insurance Company (OMIC). Dr. Rapuano is a Committee member of OMIC. Dr. Menke is an employee of OMIC. The other authors do not have any conflicts of interests.
Disclaimer
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of the Defense Health Agency, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Navy, the Department of the Army, Department of Defense, the Uniformed Services University of the Health Sciences or any other agency of the U.S. Government. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Justin, G.A., Woreta, F.A., Colyer, M.H. et al. Ophthalmic Trauma Malpractice in the Ophthalmic Mutual Insurance Company Database. Eye 37, 109–119 (2023). https://doi.org/10.1038/s41433-021-01893-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01893-4