Abstract
Aim
To compare the associated discomfort and safety between transcutaneous (Tskin) and transconjunctival (Tconj) approaches of local anaesthetic (LA) administration in lower eyelid surgery.
Methods
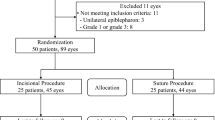
A prospective randomised controlled trial comparing Tskin and Tconj LA in patients undergoing bilateral lower eyelid surgeries for horizontal laxity. Patients were randomised to receive LA via Tskin to one side and Tconj to the fellow side. LA injection was administered in a slow fashion accompanied by distraction (tapping of patient’s forehead). Self-reported discomfort from the injections was rated using a 0–10 numerical rating scale. A single blinded assessor graded photographs for eyelid bruising (0 = absent, 1 = mild, 2 = moderate, 3 = severe).
Results
A total of 30 patients (mean age ± SD, 75.9 ± 6.7 years) were enrolled. The overall pain score (mean ± SD) was statistically lower for the Tconj than the Tskin group (3.90 ± 2.28 versus 5.33 ± 2.23, p = 0.017). More patients in the Tconj group reported substantially less pain (score of ≤3) in comparison to the Tskin group (56.7% versus 23.3%, p = 0.017). In individual patients, the Tconj pain score was found to be significantly lower than the Tskin side (p = 0.008). Bruising scores were higher in the Tskin group, but this was not statistically significant (p = 0.13). No other adverse effects were found.
Conclusion
Tconj delivery of LA in lower eyelids with horizontal laxity is safe and associated with less discomfort and bruising than the conventional Tskin route.
Trial registration number:
NCT04102878.
Similar content being viewed by others
Introduction
Eyelid surgeries are commonly performed under local anaesthesia (LA) in an outpatient setting. This has the advantage of reduced surgical time, increased patient convenience, less expense and avoidance of complications associated with systemic anaesthesia. LA administration, however, can be painful and thus can induce significant anticipatory patient anxiety and fear [1, 2]. It can also cause unsightly post-operative bruising with associated patient discomfort, prolonged recovery and other adverse effects [3]. To deliver the best care and optimise patient satisfaction, it is prudent to select a route of LA administration that will cause the least amount of pain, bruising and adverse effects.
Studies have found that the pain felt during the administration of peribulbar anaesthesia (for cataract surgery and other intraocular procedures) is reduced when the injection is administered transconjunctivally (Tconj) rather than transcutaneously (Tskin) [4, 5] and bruising/haematoma formation is also less common with Tconj delivery [6]. Apart from the work by Rafailov et al. (2015), we did not find any trials comparing Tconj and Tskin LA administration in oculoplastic procedures [7]. The aforementioned authors demonstrated that anaesthetic given Tconj in conjunction with lidocaine 2% gel, was less painful compared to Tskin administration. Lidocaine 2% gel is not widely available in United Kingdom (UK) hospitals and no published studies have compared the two routes of anaesthetic administration, when used only in combination with topical anaesthetic drops.
The aim of this study is to compare the level of patient discomfort and safety profile between Tconj and Tskin approaches of LA administration in lower eyelid surgery.
Methods
This study was reviewed and approved by the UK National Research Ethics Service and took place at Southampton General Hospital (University of Southampton NHS Trust). The study was also registered as a clinical trial (ClinicalTrials.gov Identifier: NCT04102878). Informed consent was given by all participants. Participant identifiable data were anonymised at point of collection and stored securely.
The study included patients aged 18 years or older, with horizontal laxity of the lower lids who required similar surgery for both lower lids. Exclusion criteria were (i) substantially different procedures performed on the two sides, (ii) procedures not amenable to Tconj anaesthesia, (iii) a past history of lower lid surgery on one side, (iv) patients requiring sedation or general anaesthesia, or (v) patients unable to consent for the study. Known bleeding disorders and concurrent use of antiplatelet/anticoagulant medication were recorded but were not exclusion criterion.
Administration of LA was performed by the same surgeon (WFS) for all cases. Patients received LA via Tskin to one lower eyelid and Tconj to the contralateral side. The study was single-blinded with respect to patient discomfort, and double-blinded with respect to bruising post-injection.
The primary outcome measure for the study was patient-reported discomfort during LA administration. The secondary outcome measure was the extent of visible bruising post-injection. The route of anaesthetic administration (Tconj versus Tskin) and the eyelid (right versus left) to be injected and operated on first were randomly assigned by an independent researcher. Randomisation was carried out using the random number generator function in Excel (Microsoft, 2018).
Administration of LA
Prior to LA injection, 0.5% proxymetacaine drops were instilled to the conjunctival fornices bilaterally followed by 1% tetracaine drops. LA injections consist of a 50:50 mixture of 0.5% bupivacaine and 1% lidocaine with adrenaline 1:200,000 and delivered using a 27 g hypodermic needle. Tconj injections were performed with the lax lower eyelid digitally distracted away from the globe and the needle directed into the inferior fornix conjunctiva and/or lateral canthus. Injections were delivered in a slow manner to decrease patient discomfort [8]. The volume of LA administered was the same for both the Tskin and Tconj eyelids (2–3 mls). Distraction with finger tapping of patients’ forehead was performed for all injections.
Self-reported pain score
Immediately following LA injection, patients were asked to rate the discomfort experienced from the injection on each side, using a 0–10 numerical rating scale (NRS), where 0 represented no pain and 10 represented the worst pain ever experienced. An NRS was used in this study, as it is a validated scale that requires little patient instruction, has lower failure rates than visual analogue scoring (VAS) in studies of pain perception, provides scores for parametric analysis and has been shown to be just as sensitive as the VAS [9, 10].
Assessment for post-LA bruising
Photographs of the patient’s eyelids were taken before and immediately after LA administration (Figs. 1a–f and 2a–f). These photographs were anonymised and objectively graded by an independent assessor for the presence or absence of bruising using a scale from 0 to 3: absent = 0, mild = 1, moderate = 2 and severe = 3.
Statistical analysis
Statistical analysis was performed using Excel (Microsoft, 2018). An unpaired student t test was used to compare the overall pain scores of both groups. A paired t test was used to compare the Tconj and Tskin pain scores for each individual patient. The overall bruising scores for both groups were compared using the Mann–Whitney U test. Tconj and Tskin bruising scores of the same patient were analysed using the Wilcoxon Signed rank test. A p < 0.05 was considered statistically significant.
Results
Thirty patients (21 men and 9 women) were enrolled in this study. The mean age was 75.9 years (range 62–94). All patients underwent bilateral lower lid lateral tarsal strip surgeries, while 13 of them also had additional bilateral medial spindle surgeries. All procedures took place between March and August 2019. Table 1 summarises the characteristics of the study population. Table 2 outlines the clinical parameters (pain and bruising scores) following LA administration.
Pain score
The overall mean pain score was statistically lower for the Tconj than the Tskin group (mean, 3.90 versus 5.33; unpaired student t test, p = 0.017). Paired t test analysis showed that the pain score for the Tconj side was significantly lower than the Tskin side in the same patient (p = 0.008). More patients in the Tconj group reported substantially less pain (score of ≤3) in comparison to the Tskin group (Fisher’s exact test, p = 0.017) (Table 2).
LA-related eyelid bruising
Figures 1c–f & 2c–f illustrate the appearance of the eyelids immediately following the delivery of LA injections. The mean bruising score was higher in the Tskin eyelid compared to Tconj though not statistically significant (mean, 0.8 versus 0.5; p = 0.13). Eighteen patients recorded a bruising score of zero in the Tconj group in comparison to 12 patients in the Tskin group (Fisher’s exact test, p = 0.19). Wilcoxon signed rank test did not show any statistical difference in eyelid bruising between the Tconj and Tskin groups (z = −1.59, p = 0.11). No adverse effects of LA administration were encountered in this study.
Discussion
Pain secondary to LA administration can be reduced through several methods such as warming of the anaesthetic solution [10, 11] or alkalinisation with sodium bicarbonate [12, 13]. Slowing the rate of injection and numerous ‘distraction’ techniques, can also reduce pain [8, 14, 15]. Rafailov et al.’s work showed Tconj LA to be less painful in chalazion incision and drainages, punctoplasties, and lesion biopsies of both upper and lower lids, but with the added premedication of 2% lidocaine gel [7]. In our study, we focused on a single procedure, the lateral tarsal strip (+/− medial spindle) and compared two different LA administration techniques (Tskin versus Tconj) in the same individual. This has the advantage of minimising any potential confounding factors such as patient anxiety and concurrent antiplatelet/anticoagulant medication.
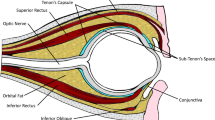
We hypothesise that injections via Tconj route through the lower conjunctival fornix were less painful than Tskin due to the avoidance of direct trauma to major nerve trunks of the lower eyelid. This theory would fit with findings from other papers that have found Tconj injections to be less painful than Tskin [4, 7, 16]. In the Tskin approach [10], the pain response begins at the level of the keratinocytes. These cells express functional sensory receptors, which in response to harmful stimuli, release substances that stimulate nociceptive sensory neurons [17]. Human cadaver studies have shown that lower eyelid somatosensory fibres from the infraorbital and zygomaticofacial nerves run superficial to the periosteum within and beneath the epimysium of the orbicularis oculi muscle (OOM) and then run perpendicular to OOM to reach the epidermis as free nerve endings [18]. In contrast to the Tskin approach, LA administration via Tconj minimises the direct stimulation of the nociceptive sensory neurons, which are located in the skin.
One study has shown that the number of nerve endings in the bulbar conjunctiva are greatest in conjunctiva located under the upper lid, followed by the interpalpebral conjunctiva, with the fewest nerve endings found in the conjunctiva covered by the lower lid [19]. However, this study focused on the bulbar conjunctiva, and we could find no similar study looking at the sensory supply of the tarsal conjunctiva. Along with free nerve endings, the conjunctiva contains nerve endings with ‘end-bulbs’, which are irregularly distributed and thought to be a sign of degenerative and regenerative nerve changes. Given that these end-bulbs are found more commonly in older patients, we speculate that conjunctival nociceptive sensation may diminish with aging [20]. Further studies of Tconj LA administration in different age groups would help to clarify this point. These two studies provide further possible mechanisms for the reduced pain perception found with the Tconj approach in this study.
In the lower eyelid, the larger palpebral vessels lie between the tarsus and OOM [21]. Direct trauma to the OOM and vascular arcades of the lower eyelid is avoided in the Tconj route, which may explain the reduced bruising we found compared with the Tskin route. Bruising was more severe in patients on anticoagulant therapy, although not found to be of statistical significance. Further studies could be done to compare the severity of bruising associated with different approaches of LA injection in lower eyelid surgery.
Study limitation
We do acknowledge that this study has a small sample size; we have adopted a robust study design to minimise any potential confounding factors that may affect the study outcome.
Conclusion
In summary, this study demonstrates that in lower eyelid surgery associated with horizontal laxity, LA administered via the Tconj route is safe and overall is less painful than the more conventional Tskin route. However, we caution that the Tconj technique should only be considered in individuals with lower eyelid horizontal laxity as this allows easy distraction of the lid away from the globe and safe administration of LA into the conjunctival space.
Summary
What was known before
-
There is very little in the literature comparing transcutaneous and transconjunctival routes of local anaesthetic administration in lower eyelid surgery.
What this study adds
-
This randomised controlled trial of 30 patients, demonstrates that in lower eyelid surgery with horizontal laxity, transconjunctival administration of local anaesthetic is associated with less pain than when given transcutaneously. There were no adverse effects with both modes of administration and transconjunctival administration was associated with less bruising.
References
Shafer A, Fish MP, Gregg KM, Seavello J, Kosek P. Preoperative anxiety and fear: a comparison of assessments by patients and anesthesia and surgery residents. Anesth Analg. 1996;83(Dec):1285–91.
Sharma A, Pant R, Priyadarshi S, Agarwal N, Tripathi S, Chaudhary M. Cardiovascular changes due to dental anxiety during local anesthesia injection for extraction. J Maxillofac Oral Surg. 2019;18(Mar):80–7.
McCaughey W. Adverse effects of local anaesthetics. Drug Saf. 1992;7(Jun):178–89.
Sweeney EJ, Barber K, Prosser JA. A comparison of percutaneous and perconjunctival routes of administration of peri-ocular anaesthesia for day case cataract surgery. Anaesthesia. 1993;48(Apr):336–8.
Bohlender T, Weindler J, Schroeder P, Ruprecht KW. [Transcutaneous or transconjunctival peribulbar anesthesia?]. Ophthalmologe . 1997;94(May):324–6.
McGrath LA, Bradshaw CP. Transconjunctival approach to peribulbar block. Clin Ophthalmol. 2013;7:1073–6.
Rafailov L, Kulak A, Weedon J, Shinder R. Comparison of lidocaine gel-assisted transconjunctival and transcutaneous local anesthesia for outpatient eyelid surgery. Ophthalmic Plast Reconstr Surg. 2015;31:470–3.
Gupta A, Tomlins PJ, Ng ATW, Reuser TT. Alleviating pain in oculoplastic procedures by reducing the rate of injection of local anaesthetic. Open Ophthalmol J. 2015;9:156–8.
Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–404.
Arndt KA, Burton C, Noe JM. Minimizing the pain of local anesthesia. Plast Reconstr Surg. 1983;72:676–9.
Bell RW, Butt ZA. Warming lignocaine reduces the pain of injection during peribulbar local anaesthesia for cataract surgery. Br J Ophthalmol. 1995;79:1015–7.
Christoph RA, Buchanan L, Begalla K, Schwartz S. Pain reduction in local anaesthetic administration through pH buffering. Ann Emerg Med. 1988;17:117–20.
Welch MN, Czyz CN, Kalwerisky K, Holck DE, Mihora LD. Double-blind, bilateral pain comparison with simultaneous injection of 2% lidocaine versus buffered 2% lidocaine for periocular anesthesia. Ophthalmology. 2012;119:2048–52.
Ing E, Philteos J, Sholohov G, Ta Kim D, Nijhawan N, Mark PW, et al. Local anesthesia and anxiolytic techniques for oculoplastic surgery. Clin Ophthalmol. 2019;13:153–60.
Gostimir M, Hussain A. A systematic review and meta-analysis of methods for reducing local anesthetic injection pain among patients undergoing periocular surgery. Ophthalmic Plast Reconstr Surg. 2019;35(Apr):113–25.
Farahi F, Haghi F, Latifi SM. Comparison of low volume transconjunctival anterior peribulbar anesthesia with transcutaneous posterior peribulbar anesthesia. Bina J Ophthalmol. 2012;1:48–51.
Talagas M, Lebonvallet N, Berthod F, Misery L. Lifting the veil on the keratinocyte contribution to cutaneous nociception. Protein Cell. 2020;11:239–50.
Hwang K, Nam YS, Choi HG, Han SH, Hwang SH. Cutaneous innervation of lower eyelid. J Craniofacial Surg. 2008;19:1675–7.
Knusel O, Vonwiller O. Vitale Farbungen am menschlichen Auge. Z fur Augenheilkd. 1922;49:157–88.
Oppenheimer DR, Palmer E, Weddell G. Nerve endings in the conjunctiva. J Anat. 1958;92:321–52.5.
Erdogmus S, Govsa F. The arterial anatomy of the eyelid: importance for reconstructive and aesthetic surgery. J Plast Reconstr Aesthet Surg. 2007;60:241–5.
Author information
Authors and Affiliations
Contributions
MJ was responsible for writing the paper, conducting statistical analyses, design of tables and figures, referencing and editing the paper. KC was responsible for writing the paper, conducting statistical analyses, obtaining patient consent, obtaining patient photographs. RN was responsible for registering trial for ethical approval, designing consent form, obtaining patient consent, obtaining patient photographs, evaluating patient photographs. AJ was responsible for designing study protocol and registering trial for ethical approval. WFS was responsible for designing the trial, performing the local anaesthetic injections in all patients, obtaining patient consent, obtaining patient photographs, contributing to data analysis, editing of the paper. All authors reviewed the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jawad, M., Chow, K., Nicholson, R. et al. Transconjunctival versus transcutaneous local anaesthetic administration for lower eyelid surgery: a randomised controlled trial. Eye 36, 1094–1099 (2022). https://doi.org/10.1038/s41433-021-01588-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01588-w