Abstract
Purpose
To compare the visual and anatomical outcomes of two different treatment strategies (non-internal limiting membrane (ILM) peeling and fovea-sparing ILM peeling) for retinoschisis with foveal detachment (FD) in highly myopic eyes.
Design
A retrospective cohort study.
Methods
Ninety-five eyes from 92 highly myopic patients with retinoschisis with FD were divided into two groups, including 44 eyes from 43 patients who received 23-gauge, 3-port vitrectomy without ILM peeling (group A) and 51 eyes from 49 patients who received vitrectomy with fovea-sparing ILM peeling (group B). All eyes also underwent cataract surgery.
Results
There were no significant differences between the two groups in terms of sex, age, diopters, axial length (AL), or central foveal thickness (CFT) before surgery (P > 0.05). One month after surgery, foveoschisis and FD were resolved in 74.47% of the eyes in group B and in only 12.50% of those in group A. Six months after surgery, foveoschisis and FD were resolved in 96.08% of the eyes in group B and in only 72.73% of those in group A (P < 0.05). There were no significant differences between the two groups in terms of BCVA 6 months after surgery. The postoperative complication was macular holes, which were found in seven eyes (15.90%) in group A and in one eye (1.96%) in group B (P < 0.05).
Conclusion
Highly myopic eyes with FD that underwent fovea-sparing ILM peeling appeared to obtain a better anatomical outcome than those that did not undergo non-ILM peeling. The two procedures obtained similar results in terms of visual function.
Similar content being viewed by others
Myopic retinopathy is one of the most common causes of irreversible visual impairment and blindness due to the high incidence rate of high myopia [1]. Myopic foveoschisis (MF), a common finding in the macula of highly myopic eyes [2], is one of the major causes of poor vision in eyes with pathologic myopia. Based on optical coherence tomography (OCT) images of the macular region, MF can be divided into three stages: isolated retinoschisis, retinoschisis with foveal detachment (FD), and retinoschisis with a macular hole (MH) [3]. Patients with isolated retinoschisis may have stable vision for a long time. However, when retinoschisis progresses to FD or FD progresses to MH, the patient’s visual acuity drops sharply, and MH retinal detachment may easily develop [4]. Thus, stage II (retinoschisis with FD) is the best time to start surgical treatment.
At present, the mainstream treatment for retinoschisis with FD is vitrectomy. Studies have shown that vitrectomy could result in good anatomical and visual outcomes in highly myopic eyes [5,6,7,8,9,10,11,12,13,14,15]. However, how to address the ILM remains controversial. Some studies proposed vitrectomy without ILM peeling and showed that the prevalence of postoperative MH was much lower than that in ILM peeling cases, but the recovery rate may not be satisfactory [12, 16]. In contrast, people who promote ILM peeling believe that it can increase the recovery rate but that postoperative MH may occur (8–18%) [17, 18] and result in poor postoperative VA. Recently, some researchers have proposed a fovea-sparing ILM technique to reduce the risk of iatrogenic MH formation [19,20,21,22,23,24]. Could fovea-sparing ILM peeling increase the anatomic resolution and reduce the incidence of postoperative MHs in FD patients at the same time? Comparing non-ILM peeling with fovea-sparing ILM peeling, which procedure is better? For these purposes, we designed this study. This study analyzed 95 eyes from 92 patients with MS and FD treated with PPV without ILM peeling or with ILM peeling that avoided the foveal area to determine which procedure is better for treating this disease.
Methods
This retrospective interventional case series included all patients who presented with decreased visual acuity due to retinoschisis with FD in highly myopic eyes and underwent vitrectomy from July 2011 to November 2017. From July 2011 to December 2015, the patients underwent vitrectomy without ILM peeling. From December 2015 to November 2017, the patients underwent vitrectomy with ILM peeling that avoided the foveal area. The Medical Ethics Committee of the Beijing Tongren Hospital approved the study protocol, and all participants gave informed consent. A refractive status, the best corrected visual acuity (BCVA), A-mode ultrasonography, color fundus photography (Topcon TRC-50, Tokyo, Japan), and retinal OCT (Stratus OCT; Carl Zeiss Meditec, Dublin, CA, USA) were routinely performed for each patient pre- and post-operation. FD was identified by OCT. All patients followed up for at least 6 months.
This clinical interventional study included all patients who presented with a loss in visual acuity because of FD in highly myopic eyes with an axial length (AL) of >27.0 mm. Patients with stage I and III MF, who were <30 years old, who had a history of vitrectomy, or who had any other fundus or system diseases were excluded.
Patients were divided into two groups according to their operative method. Forty-four eyes from 43 patients in group A were treated with a standard 23-gauge, 3-port pars plana vitrectomy (PPV) without ILM peeling, and 51 eyes from 49 patients in group B were treated with PPV with ILM peeling that avoided foveal area. All eyes also underwent cataract surgery. All procedures were performed by the same surgeon (ALD).
A standard 23-gauge PPV, combined with phacoemulsification and intraocular lens implantation, was performed. After cataract surgery, 0.1–0.2 mL of triamcinolone acetonide (20 mg/mL) was injected into the vitreous cavity to visualize the vitreous. A core vitrectomy was performed, and the posterior hyaloid membrane was removed from the macular surface by aspiration with the vitrector or a flute tip needle. The ILM was not peeled in the cases in group A (Video 1). The ILM was visualized by indocyanine green and peeled off with forceps in a donut-like shape (fovea sparing, ~1 PD) in group B (Video 2). Finally, fluid–gas exchange was carried out, and gas or silicone oil was applied as padding (the tamponades were mainly inert gas, though two cases had silicone oil and some cases had air because there had been no inert gases in the TR eye center since November 2017). All patients were kept in a prone position for at least week after surgery.
At the postoperative follow-up examinations, measurement of visual acuity and OCT were routinely performed. All patients completed more than 6 months of follow-up.
Statistical analysis was performed using a commercially available statistical software package (SPSS for Windows, version 23.0, IBM-SPSS, Chicago, IL). The measurements of BCVA were converted into the logarithm of the minimum angle of resolution (logMAR). The parameters are presented as the means ± standard deviations. Mean age, refractive error, AL, central foveal thickness (CFT) and visual acuity were analyzed with Student’s t test. Differences in the incidence rates of OCT findings were analyzed by corrected chi-square test. A P value < 0.05 was considered statistically significant.
Results
The present study included 95 eyes from 92 patients. All eyes had a posterior staphyloma. Patients in group A and group B did not differ significantly (all P > 0.05) in age (49.93 ± 10.36 years vs. 51.45 ± 9.95 years; t = −0.94, P = 0.46), refractive error (−16.56 ± 4.79 D vs. −14.88 ± 3.52 D; t = 1.75; P = 0.59), AL (29.92 ± 1.75 mm vs. 29.56 ± 1.49 mm; t = −1.01, P = 0.32), CFT (634.37 ± 132.42 µm vs. 613.88 ± 184.05 µm; t = −1.26, P = 0.21), or preoperative BCVA (0.90 ± 0.52 logMAR vs. 1.07 ± 0.39 logMAR; t = −1.02; P = 0.32) (Table 1).
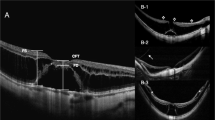
Postoperatively, anatomic success was defined as a CFT decrease of more than 90%. One month after surgery, 74.47% of eyes in group B and 12.50% in group A achieved anatomic success (P = 0.02) (Figs. 1 and 2). Six months after surgery, 96.08% of eyes in group B and 72.73% of eyes in group A achieved anatomic success (P < 0.01). There were no significant differences between the two groups in terms of the change in BCVA 6 months after surgery (P = 0.81) (Table 2).
Tamponades included air, inert gases (C2F6, C3F8, and SF6), and silicon oil. The details of the tamponades are shown in Table 3. There was no significant difference in the proportion of the three tamponades between the two groups (P > 0.05).
The postoperative complication was MH, which was found in seven eyes (15.90%) in group A and in one eye (1.96%) in group B (P = 0.02). All eight eyes underwent a second operation. The ILM in the foveal area was peeled and packed into the MH. Four eyes were filled with C3F8, and the others were filled with silicone oil (because there were no inert gases at that time). MHs in six eyes were resolved after the second operation.
Discussion
This surgical interventional case series study showed that patients with myopic retinoschisis with FD can be successfully treated by PPV combined with fovea-sparing ILM peeling with better anatomical outcomes and fewer postoperative complications than those treated with non-ILM peeling.
PPV is the mainstream surgery for MF. It can alleviate vitreous traction to the retina. When MF develops into FD, there are usually very few retinal tissues remaining and covering the top of the retinal detachment area. A degrading retina leads to MHs being easily formed in highly myopic eyes. Less irritation and injury are necessary to maintain the stability of the macular area and avoid postoperative MH formation. In previous studies, PPV with ILM peeling has been shown to easily cause iatrogenic MHs [1].
In this study, two procedures (non-ILM peeling/fovea-sparing ILM peeling) were compared, and the results showed that these two methods have their own advantages. While non-ILM peeling is easy and shortcuts may bring less injury to the macula, fovea-sparing ILM peeling can achieve better healing and fewer postoperative complications (i.e., MHs). In this study, 1 month after surgery, 74.47% of eyes in group B exhibited healing of foveoschisis and FD, whereas only 12.50% in group A did. Six months after surgery, foveoschisis and FD were completely resolved in 96.08% of eyes in group B and in only 72.73% of those in group A. The recovery rate in group B was higher than that in group A in both the short and long term.
The two procedures obtained similar results in terms of visual function. The postoperative BCVA was improved in both groups. The increasing extent of BCVA had no significant differences between group A and group B. The results for visual recovery were similar to those of previous studies: the final VA appears to not be affected by the ILM processing method in the macular area. Many properties may impact postoperative BCVA in highly myopic patients with FD, such as baseline BCVA, choroid membrane atrophy of the macular area, duration of macular detachment, phacoemulsification, age. The operation procedure is not the only determinant.
Some doctors invented the fovea-sparing ILM peeling technique to avoid postoperative MHs. In support of their technique was Seppey et al. [19] who analyzed six patients with MF. All patients underwent fovea-sparing ILM peeling and a 23% SF6 tamponade. Both BCVA and CFT were significantly improved after surgery. No patient developed an MH. They believed that this surgical technique may reduce the risk of MH formation. Lee et al. [9] reviewed ten MF eyes that received vitrectomy with fovea-sparing ILM peeling. After surgical intervention, the MF resolved in all ten eyes. The mean BCVA and CFT were both significantly improved. None of the ten eyes developed MHs. They thought that this technique minimized the traction force over the extremely thinned foveal tissue and brought good anatomic and visual results in highly myopic eyes. Jin et al. [20] performed fovea-sparing ILM peeling using multiple parafoveal curvilinear peels in 20 eyes with MF. Both the postoperative BCVA and CFT were better than the preoperative BCVA and CFT. Postoperative OCT examinations showed that full-thickness MHs did not develop in any case. They thought fovea-sparing ILM peeling using multiple parafoveal curvilinear peels prevented the development of postoperative full-thickness MHs in eyes with MF. In addition, some doctors compared total ILM peeling with fovea-sparing ILM peeling in MF patients. Elwan et al. [21] compared vitrectomy with whole macula ILM peeling and fovea-sparing ILM peeling in 28 MF patients. There was statistically significant improvement in the final BCVA within each group. CFT significantly decreased postoperatively within each group. However, there were no significant differences in the final BCVA and CFT between the two groups. No MHs were recorded in either group. They believed vitrectomy with complete ILM peeling resulted in comparable outcomes to those achieved with preservation of the epi-foveal membrane in treating MF cases. Shimada et al. [22] compared vitrectomy with whole macula ILM peeling and fovea-sparing ILM peeling in 45 FD patients. MHs developed in 16.7% of eyes in the complete ILM peeling group and in no eyes in the fovea-sparing ILM peeling group. The postoperative BCVA was significantly better than the preoperative BCVA in the fovea-sparing ILM peeling group but not in the complete ILM peeling group. They considered that fovea-sparing ILM peeling resulted in better visual and anatomic outcomes for the treatment of FD and reduced the development of a full-thickness MH. Ho et al. [23] reviewed 19 eyes with MF and divided them into two groups according to the extent of ILM peeling and followed them for more than 3 years. MHs developed in 28.6% of eyes in the total ILM peeling (TP) group and in none of the fovea-sparing group. Long-term CFT thinning and decreased vision were found in the TP group but not in the fovea-sparing group. The inner segment/outer segment line recovered better in the fovea-sparing group. They thought that fovea-sparing ILM peeling correlated with better anatomical and visual results than total peeling, prevented long-term foveolar retinal thinning, and successfully saved the fovea from MH formation. Previous studies compared fovea-sparing ILM peeling with total ILM peeling. However, no study focused on non-ILM peeling and fovea-sparing ILM peeling. Non-ILM peeling is also a popular choice to treat FD.
Some controversies remain regarding the choices of tamponade in patients with MF. In our study, the tamponade included air, inert gas (C2F6, C3F8, and SF6) and silicone oil. The lack of inert gas in China affected our choice for tamponade. When there was no inert gas, we could only fill eyes with room air or silicone oil. The principle of gas selection was as follows: for eyes with serious FD, an inert gas was chosen that could remain in the eyes a long time. The ratio of air tamponade was 13.6% in group A and 15.7% in group B. The ratio of inert gas tamponade was 86.2% in group A and 80.4% in group B. The ratio of silicone oil tamponade was 0.0% in group A and 3.9% in group B. There was no significant difference in the proportion of the three tamponades between the two groups. We believe that the use of these tamponades did not affect our results. Meng et al. [24] conducted a meta-analysis study about ILM peeling and gas tamponade for MF, and nine studies that included 239 eyes were selected. They found that the proportion of foveoschisis resolution between the tamponade group and the non-tamponade group was similar, and they conjectured that gas tamponade had no significant impact on either the resolution of MF or visual acuity. Ma et al. [25] conducted an intravitreal injection of 0.2–0.3 mL C3F8 as an initial treatment for FD patients and found that FD resolved completely in 70% of eyes. They believed that injection of inert gas (C3F8) into the vitreous cavity alone could cure FD in most patients.
MF is more likely to occur in eyes with a posterior staphyloma [26]. Posterior staphyloma in combination with an increase in the length of the vitreous cavity generally leads directly and indirectly to increased vitreofoveal traction and vitreoretinal arterial traction, which has been considered a possible cause of MF [27,28,29]. In the present study, since all patients enrolled in the two groups had posterior staphyloma, we were not able to evaluate whether this confounding factor could influence the result, and this needs further investigation in the future.
The limitations of the current study include the following: first, this was not a randomized study. The differences in the composition of the two groups, even if not statistically significant, may have influenced the statistical analysis. Second, the present study focused on the controversy between non-ILM peeling and fovea-sparing ILM peeling. Concerning the controversy between total ILM peeling and fovea sparing, this study is not able to clarify this issue.
In conclusion, fovea-sparing ILM peeling in association with PPV, compared with PPV without ILM peeling, resulted in a shorter recovery time, higher recovery rate, and fewer postoperative complications in highly myopic eyes with MF and FD. The postoperative retinal function recovery was similar.
Summary
What was known before
-
Myopic foveoschisis with foveal detachment had been treated by vitrectomy without ILM peeling as well as foveal sparing ILM peeling in an attempt to reduce the occurrence of postoperative complications.
What this study adds
-
We performed this retrospective study to assess which is the best method for improving anatomical and functional outcomes, and to reduce the incidence of postoperative macular holes.
References
Xu L, Wang Y, Li Y, Wang Y, Cui T, Li J, et al. Causes of blindness and visual impairment in an urban and rural area in Beijing: the Beijing Eye Study. Ophthalmology. 2006;113:1134. 1–11.
You QS, Peng XY, Xu L, Chen CX, Wang YX, Jonas JB. Myopic maculopathy imaged by optical coherence tomography. The Beijing Eye Study. Ophthalmology. 2014;121:220–4.
Ikuno Y, Sayanagi K, Soga K, Oshima Y, Ohji M, Tano Y. Foveal anatomical status and surgical results in vitrectomy for myopic foveoschisis. Jpn J Ophthalmol. 2008;52:269–76.
Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T, Mochizuki M. Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol. 2006;142:497–500.
Qi Y, Duan AL, Meng X, Wang N. Vitrectomy without inner limiting membrane peeling for macular retinoschisis in highly myopic eyes. Retina. 2016;36:953–6.
Kobayashi H, Kishi S. Vitreous surgery for highly myopic eyes with foveal detachment and retinoschisis. Ophthalmology. 2003;110:1702–7.
Kim KS, Lee SB, Lee WK. Vitrectomy and internal limiting membrane peeling with and without gas tamponade for myopic foveoschisis. Am J Ophthalmol. 2012;153:320–6.
Figueroa MS, Ruiz-Moreno JM, Gonzalez del Valle F, Govetto A, de la Vega C, Plascencia Raquel N, et al. Long-term outcomes of 23-gauge pars plana vitrectomy with internal limiting membrane peeling and gas tamponade for myopic traction maculopathy. Retina. 2015;35:1836–43.
Lee CL, Wu WC, Chen KJ, Chiu LY, Wu KY, Chang YC. Modified internal limiting membrane peeling technique (maculorrhexis) for myopic foveoschisis surgery. Acta Ophthalmol. 2017;95:128–31.
Zheng B, Chen Y, Chen Y, Zhao ZQ, Zhang ZD, Zheng JW, et al. Vitrectomy and internal limiting membrane peeling with perfluoropropane tamponade or balanced saline solution for myopic foveoschisis. Retina. 2011;31:692–701.
Al-Badawi AH, Abdelhakim MASE, Macky TA, Mortada HA. Efficacy of non-fovea-sparing ILM peeling for symptomatic myopic foveoschisis with and without macular hole. Br J Ophthalmol. 2019;103:257–63.
Kwok AK, Lai TY, Yip WW. Vitrectomy and gas tamponade without internal limiting membrane peeling for myopic foveoschisis. Br J Ophthalmol. 2005;89:1180–3.
Hirakata A, Hida T. Vitrectomy for myopic posterior retinoschisis or foveal detachment. Jpn J Ophthalmol. 2006;50:53–61.
Scott IU, Moshfeghi AA, Flynn HW Jr. Surgical management of macular retinoschisis associated with high myopia. Arch Ophthalmol. 2006;124:1197–9.
Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007;125:767–72.
Huang Y, Huang W, Ng DSC, Duan AL. Risk factors for development of macular hole retinal detachment after pars plana vitrectomy for pathologic myopic foveoschisis. Retina. 2017;37:1049–54.
Rizzo S, Giansanti F, Finocchio L, Caporossi T, Barca F, Bacherini D, et al. Vitrectomy with internal limiting membrane peeling and air tamponade for myopic foveoschisis. Retina. 2019;39:2125–31.
Iida Y, Hangai M, Yoshikawa M, Ooto S, Yoshimura N. Local biometric features and visual prognosis after surgery for treatment of myopic foveoschisis. Retina. 2013;33:1179–87.
Seppey C, Wolfensberger TG. Vitrectomy with fovea-sparing internal limiting membrane peeling for myopic foveoschisis. Klin Monbl Augenheilkd. 2017;234:497–500.
Jin H, Zhang Q, Zhao P. Fovea sparing internal limiting membrane peeling using multiple parafoveal curvilinear peels for myopic foveoschisis: technique and outcome. BMC Ophthalmol. 2016;16:180–5.
Elwan MM, Abd Elghafar AE, Hagras SM, Abou Samra WA, Saleh SM. Long-term outcome of internal limiting membrane peeling with and without foveal sparing in myopic foveoschisis. Eur J Ophthalmol. 2019;29:69–74.
Shimada N, Sugamoto Y, Ogawa M, Takase H, Ohno-Matsui K. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012;154:693–701.
Ho TC, Yang CM, Huang JS, Yang CH, Yeh PT, Chen TC, et al. Long-term outcome of foveolar internal limiting membrane non-peeling for myopic traction maculopathy. Retina. 2014;34:1833–40.
Meng B, Zaho L, Yin Y, Li H, Wang X, Yang X, et al. Internal limiting membrane peeling and gas tamponade for myopic foveoschisis: a systematic review and meta-analysis. BMC Ophthalmol. 2017;17:166–76.
Ma IH, Hsieh YT, Yeh PT, Yang CH, Yang CM. Long-term results and risk factors influencing outcome of gas tamponade for myopic foveoschisis with foveal detachment. Eye. 2020;34:392–9.
Baba T, Ohno-Matsui K, Futagami S, Yoshida T, Yasuzumi K, Kojima A, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135:338–42.
Benhamou N, Massin P, Haouchine B, Erginay A, Gaudric A. Macular retinoschisis in highly myopic eyes. Am J Ophthalmol. 2002;133:794–800.
Ikuno Y, Gomi F, Tano Y. Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol. 2005;139:462–7.
Chan HL, Mohidin N. Variation of multifocal electroretinogram with axial length. Ophthalmic Physiol Opt. 2003;23:133–40.
Acknowledgements
Supported by “Beijing Municipal Administration of Hospitals Incubating Program”, code: PX2016006.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qi, Y., Yan, P., Fan, W. et al. Comparison of fovea-sparing and non-internal limiting membrane peeling for retinoschisis with foveal detachment in highly myopic eyes. Eye 35, 1467–1472 (2021). https://doi.org/10.1038/s41433-020-1108-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1108-5