Abstract
Background/Objectives
Malnutrition risk screening represents a crucial starting point for the successful management of malnourished patients. This study was conducted to (1) examine the effect of the use of a malnutrition screening tool on process indicators of nutritional care and (2) explore healthcare professionals’ perceptions and opinions regarding this tool.
Methods
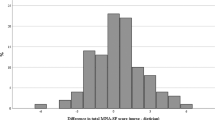
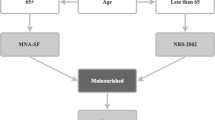
A mixed methods design was used. A controlled pretest–posttest study was conducted to carry out quantitative analyses, and semi-structured, qualitative interviews were held. Quantitative data were analysed with descriptive statistics, Chi-squared tests, Student’s t-tests and Kruskal–Wallis H tests, using SPSS 23. Qualitative data were analysed by performing a qualitative content analysis using MAXQDA 12. Two comparable hospitals participated in the study, representing one intervention group (IG) and one control group (CG). The Graz Malnutrition Screening Tool (GMS) was implemented and used in the IG for at least 1 month, while the CG received no intervention.
Results
The use of the screening tool positively correlated with significant improvements in the process indicators of nutritional care after 1 month, in terms of the number of nutritional interventions and the frequency of documentation of the diagnosis and the patient’s weight and height. The content of the interviews revealed that nearly all professionals involved perceived the overall screening process positively. Few barriers were identified.
Conclusions
The results of this study show that the use of a screening tool has a positive, short-term impact on the hospital’s process quality of nutritional care. Ongoing efforts are required to sustainably maintain these positive changes. During this process, positive attitudes, nomination of motivated ‘opinion-leaders’ and concerted management support are helpful facilitators.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Thomas MN, Kufeldt J, Kisser U, Hornung HM, Hoffmann J, Andraschko M, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. 2016;32:249–54. https://doi.org/10.1016/j.nut.2015.08.021.
Felder S, Lechtenboehmer C, Bally M, Fehr R, Deiss M, Faessler L, et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015;31:1385–93. https://doi.org/10.1016/j.nut.2015.06.007.
Lew CC, Yandell R, Fraser RJ, Chua AP, Chong MF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review. J Parenter Enteral Nutr. 2016. https://doi.org/10.1177/0148607115625638.
Khalatban-Soltani S, Marques-Vidal P. The economic cost of hospital malnutrition in Europe; a narrative review. Clin Nutr ESPEN. 2015;10:e89–94.
Guerra RS, Sousa AS, Fonseca I, Pichel F, Restivo MT, Ferreira S, et al. Comparative analysis of undernutrition screening and diagnostic tools as predictors of hospitalisation costs. J Hum Nutr Diet. 2016;29:165–73. https://doi.org/10.1111/jhn.12288.
Raynaud-Simon A, Revel-Delhom C, Hebuterne X. Clinical practice guidelines from the French Health High Authority: nutritional support strategy in protein-energy malnutrition in the elderly. Clin Nutr. 2011;30:312–9. https://doi.org/10.1016/j.clnu.2010.12.003.
Group DMS. Guideline on malnutrition. In: Kruizenga H, Beijer S, Hulsman-de Waal G, Jonkers-Schultema C, Klos M, Remijnse-Meester W, et al., editors. Recognising, diagnosing and treating malnutrition in adults. Dutch Malnutrition Steering Group. Guidline on malnutrition. 2017. p. 36.
NICE. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. https://www.nice.org.uk/guidance/cg32/chapter/About-this-guideline. 2013.
Mueller C, Compher C, Ellen DM. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. J Parenter Enter Nutr. 2011;35:16–24. https://doi.org/10.1177/0148607110389335.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36:49–64. https://doi.org/10.1016/j.clnu.2016.09.004.
Bueche J, Charney P, Pavlinac J, Skipper A, Thompson E, Myers E, et al. Nutrition care process and model part I: the 2008 update. J Am Diet Assoc. 2008;108:1113–7. https://doi.org/10.1016/j.jada.2008.04.027.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition—an ESPEN Consensus Statement. Clin Nutr. 2015;34:335–40. https://doi.org/10.1016/j.clnu.2015.03.001.
Eglseer D, Halfens RJ, Lohrmann C. Is the presence of a validated malnutrition screening tool associated with better nutritional care in hospitalized patients? Nutrition. 2017;37:104–11. https://doi.org/10.1016/j.nut.2016.12.016.
White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Parenter Enter Nutr. 2012;36:275–83. https://doi.org/10.1177/0148607112440285.
Pirkle CM, Dumont A, Zunzunegui MV. Medical recordkeeping, essential but overlooked aspect of quality of care in resource-limited settings. Int J Qual Health Care. 2012;24:564–7. https://doi.org/10.1093/intqhc/mzs034.
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet. 2013;113:1219–37. https://doi.org/10.1016/j.jand.2013.05.015.
Smith PC. Performance measurement for health system improvement: experiences, challenges and prospects. Cambridge University Press; New York. 2009.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15:523–30. https://doi.org/10.1093/intqhc/mzg081
Omidvari AH, Vali Y, Murray SM, Wonderling D, Rashidian A. Nutritional screening for improving professional practice for patient outcomes in hospital and primary care settings. Cochrane Database Syst Rev. 2013;CD005539. https://doi.org/10.1002/14651858.CD005539.pub2.
Green SM, James EP. Barriers and facilitators to undertaking nutritional screening of patients: a systematic review. J Hum Nutr Diet. 2013;26:211–21. https://doi.org/10.1111/jhn.12011.
Borglin G. The value of mixed methods for researching complex interventions. Oxon: Routledge; 2015.
Creswell JW. A concise introduction to mixed methods research. Sage Publications; Los Angeles. 2014.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2015.
Roller RE, Eglseer D, Eisenberger A, Wirnsberger GH. The Graz Malnutrition Screening (GMS): a new hospital screening tool for malnutrition. Br J Nutr. 2016;115:650–7. https://doi.org/10.1017/s0007114515004924.
Released IC. IBM SPSS statistics for Windows. Version 23.0. Armonk, NY: IBM Corp.; 2015.
Neuendorf K. The content analysis guidebook. 2nd ed. California: SAGE Publications, Inc.; 2017.
Schreier M. Qualitative content analysis in practice. 1st ed. London: SAGE Publications Ltd.; 2012.
GmbH VS-C-S MAXQDA, software for qualitative data analysis. 1989–2018.
Leistra E, van Bokhorst-de van der Schueren MA, Visser M, van der Hout A, Langius JA, Kruizenga HM. Systematic screening for undernutrition in hospitals: predictive factors for success. Clin Nutr. 2014;33:495–501. https://doi.org/10.1016/j.clnu.2013.07.005.
Keller HH, Vesnaver E, Davidson B, Allard J, Laporte M, Bernier P, et al. Providing quality nutrition care in acute care hospitals: perspectives of nutrition care personnel. J Hum Nutr Diet. 2014;27:192–202. https://doi.org/10.1111/jhn.12170.
Green SM, James EP, Latter S, Sutcliffe M, Fader MJ. Barriers and facilitators to screening for malnutrition by community nurses: a qualitative study. J Hum Nutr Diet. 2014;27:88–95. https://doi.org/10.1111/jhn.12104.
Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Lindorff K, Jorgensen LM, et al. A method for implementation of nutritional therapy in hospitals. Clin Nutr. 2006;25:515–23. https://doi.org/10.1016/j.clnu.2006.01.003.
Eide HD, Halvorsen K, Almendingen K. Barriers to nutritional care for the undernourished hospitalised elderly: perspectives of nurses. J Clin Nurs. 2015;24:696–706. https://doi.org/10.1111/jocn.12562.
Boaz A, Baeza J, Fraser A. Effective implementation of research into practice: an overview of systematic reviews of the health literature. BMC Res Notes. 2011;4:212 https://doi.org/10.1186/1756-0500-4-212.
Flodgren G, Parmelli E, Doumit G, Gattellari M, O’Brien MA, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2011;CD000125. https://doi.org/10.1002/14651858.CD000125.pub4.
DeLegge MH, Kelly AT. State of nutrition support teams. Nutr Clin Pract. 2013;28:691–7. https://doi.org/10.1177/0884533613507455.
Hvas CL, Farrer K, Donaldson E, Blackett B, Lloyd H, Forde C, et al. Quality and safety impact on the provision of parenteral nutrition through introduction of a nutrition support team. Eur J Clin Nutr. 2014;68:1294–9. https://doi.org/10.1038/ejcn.2014.186.
Cong MH, Li SL, Cheng GW, Liu JY, Song CX, Deng YB, et al. An interdisciplinary nutrition support team improves clinical and hospitalized outcomes of esophageal cancer patients with concurrent chemoradiotherapy. Chin Med J. 2015;128:3003–7. https://doi.org/10.4103/0366-6999.168963.
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Parenter Enter Nutr. 2013;37:482–97. https://doi.org/10.1177/0148607113484066.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethical approval was obtained from the responsible ethics committee (29-270 ex 16/17). The hospitals participated on a voluntary basis, and all responsible persons (medical and nursing hospital directors) gave their written informed consent. The persons interviewed agreed orally to participate in the interviews. Following the recommendations of the ethics committee, it was not necessary to obtain the informed consent from the patients because we only collected routine data.
Rights and permissions
About this article
Cite this article
Eglseer, D., Schoberer, D., Halfens, R. et al. The impact of using a malnutrition screening tool in a hospital setting: a mixed methods study. Eur J Clin Nutr 73, 284–292 (2019). https://doi.org/10.1038/s41430-018-0339-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0339-z