Abstract
Objectives The aim of this pooled data analysis was to establish if there is an association between a patient's race and the proportion of successful outcomes of endodontic treatments, and if so, what factors may determine this association.
Methodology Data collected from four prospective clinical outcome studies were pooled. Patients were recalled 12 months after the completion of the treatment. Treatment outcome was determined by clinical findings and cone beam computed tomography examination. Statistical analysis included the description of categorical and continuous variables and simple binary logistic regression models, chi-squared tests and Kruskal-Wallis tests.
Results Data from 301 patients were available. Of these patients, 43 were Black (14.3%), 50 were from a Non-Black Minority Ethnic (NBME) group (16.6%) and 208 were white (69.1%). The risk of an unfavourable outcome was higher in teeth with short root canal fillings (OR = 3.36; p = 0.002), when a preoperative radiolucency was present (OR = 2.59; p = 0.019) and when an intra-operative root canal perforation was detected (OR = 5.25; p = 0.016).
Multiple regression models showed that Black (OR = 2.28; p = 0.05) and NBME patients (OR = 3.07; p = 0.008) had a higher risk of an unfavourable result compared to white patients.
Conclusions Black and NBME patients had a significantly higher failure rate of root canal treatments compared to white patients. All other known pre-, intra- and post-operative risk factors for root canal treatment failure were present in similar proportions in BME and white patients.
Key points
-
Clinicians need to be aware that Black and non-Black minority ethnic patients may have less successful outcomes of root canal treatments compared to white patients.
-
This information can create awareness about differences in racial outcomes.
-
Clinicians can ensure extra care is taken to follow endodontic treatment protocols thereby reducing discrepancies.
Similar content being viewed by others
Introduction
In England, 5.6 million NHS patients received root canal treatment between 2014-2015, not including privately treated cases.1 Radiographic and clinical findings have been widely accepted in research to determine the success or failure of endodontic treatments, as suggested by Strindberg in 1956.2,3,4 The success of an endodontic treatment is determined by the presence or absence of apical pathology and clinical signs and symptoms. Cone beam computed tomography (CBCT) offers a more sensitive and accurate method of detecting apical periodontitis compared to periapical radiographs.5 Outcome studies utilising CBCT scanning therefore may offer more insight into the factors that affect the outcome of endodontic treatment.6,7,8
Most clinical research is directed upon the outcomes of treatment healthcare professionals provide, focusing on the methods, materials and treatment protocols. There is substantive evidence, however, that broader social determinants impact how health care is provided. One social determinant that has been shown to impact on health and health care is race, with research showing that Black, Asian and Minority Ethnic patients often receive a lower quality of health care and are less likely to receive preventative treatments. The US Institute of Medicine published the Unequal treatment report, which also took into consideration factors which are often used to explain such racial disparities.9 This has been documented in relation to heart disease, hypertension and diabetes,10,11 as well as cancer diagnosis, including cervical, breast, colorectal, lung and prostate cancer.12,13,14,15 This has even been noted in infant mortality rates and infantile quality of care,16 with Black mothers in the UK being five times more likely to die after complications from childbirth and pregnancy compared to white women.17 While the majority of research on the relationship between race and health focuses on general health, there is a growing body of work exploring the relationship between racism and oral health inequalities.18,19,20
The terms race and ethnicity are commonly used as terms to classify human diversity; race as a broad category to group people upon their ancestral origin and physical characteristics and ethnicity as those that share a common cultural tradition, values or religion. Both are considered to be social constructs that are without scientific or biologic meaning.21 They are, however, helpful in research and are used as determinants of people's access to education, health care and when focusing on inequalities in health outcomes. The category of race has, therefore, been used in this study.22
Research on unconscious biases suggests that while some people hold conscious biases and express their prejudice beliefs openly, this is largely deemed unacceptable. In contrast, many people have unconscious biases, which may affect their decisions and actions without them being aware.
Though the impact that racial bias has upon medical outcomes have been extensively researched, there is very little research focused on its impact on dental outcomes.
We performed a pooled analysis of four prospective clinical trials investigating the outcome of endodontic treatments, undertaken at King's College London Dental Institute. The aim of this pooled data analysis was to establish if the outcome - root canal treatment - is affected by patient race, and if so, what factors may be the cause of this inconsistency.
Materials and methods
This is a retrospective analysis of data collected from four prospective clinical outcome studies which were pooled, including two studies on primary root canal treatments23,24 and two endodontic retreatment studies.7,25 Ethical approval to extract and analyse data from four studies were granted by National Research Ethics Service (NRES) London Bridge and Dulwich Research Ethics Committees (20/WM/0013), NRES West London Research Ethics Committees (13/LO/1171) and NRES Westminster Research Ethics Committee (08/H0804/79).
All patients included in these studies were referred to Guys Dental Hospital for the management of primary or secondary endodontic disease.
The inclusion criteria for the four studies have been described7,23,24,25 in the online Supplementary Information and Tables 1, 2 and 3. Common exclusion criteria included: those pregnant; unrestorable teeth; immunosuppressed patients and teeth with periodontal probing depths exceeding 3 mm; immature teeth; and teeth with internal/external root resorption. Patients who had more than one tooth treated and patients with missing information on socioeconomic background were also excluded. All patients underwent a full assessment, including routine medical and dental history, pain history and a soft and hard tissue examination. Digital periapical radiographs and CBCT scans were taken for all cases pre-operatively and 12 months after treatment as described in the original papers.23,24,25,26 Data regarding race (both patient and operator), patient medical history, root length and root curvature were extracted from patients' dental records and the likely socioeconomic status (SES) of the patient was determined via the index of multiple deprivation (IMD).27 Race was self-reported by study participants and race categories (Black and white) were defined by investigators based on the 2021 UK Census.28 An additional analysis was carried out, including grouping individuals who self-reported being Asian (Bangladeshi, Chinese, Indian, Pakistani) or from a non-Black Minority Ethnic (NBME) group due to small individual sample sizes. Patients were asked to complete a questionnaire which included demographic information upon admission into the hospital, if they wished to do so. Data on patients' race was taken from this.
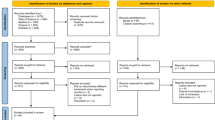
All other data, including endodontic outcome determined by CBCT, pre-operative presence of a sinus tract, pre-operative presence of pain, swelling, obturation length and intra-operative root perforation, were available, as they had already been collected in the selected studies (Fig. 1).
Clinical intervention
Both primary root canal treatments and re-treatments were completed in one visit, or two visits with an interappointment calcium hydroxide medication using a standardised protocol7,23,24,25 (see online Supplementary Information), consistent with European Society of Endodontology guidelines,29 or an additional enhanced infection protocol.24 Operative procedures were undertaken by 35 endodontic residents, of which 14 were white and 21 were Asian or from a minority ethnic group, under the direct supervision of specialist endodontic staff at Guy's and St Thomas' NHS Foundation Trust, London, UK. None of the operators were Black (no Black endodontic resident was attending the programme). All received appropriate training and standardisation before the start of the studies. Where indicated, teeth were restored with cuspal coverage restorations within one month of the completion of the root canal treatment by the endodontic residents7 or by the referring dentists.23,24,25
Outcome assessment
Patients were recalled 12 months after the completion of the treatment. Treatment outcome in this review was determined based on the clinical and CBCT radiographic findings only7,23,24,25 (see online Supplementary Information and Table 4).
Outcome was classified as follows:
-
Favourable - functional and asymptomatic teeth with absence or decreased size of periapical radiolucency
-
Unfavourable - non-functional, symptomatic teeth and teeth with unchanged, new, or enlarged periapical radiolucency.
Data analysis
The influence of patients' race on the outcome of the treatment was the primary variable of the research. The aforementioned recorded variables were also analysed, including: sex and race of the operator and patient; the likely SES of the patient based on IMD scores; patient medical history; root length; root curvature; pre-operative presence of a sinus tract; pre-operative presence of pain; swelling; intra-operative root perforation; and obturation length. Root canal anatomy (including curvature) and quality of the root canal treatments (length and presence or absence of voids) were measured at root-level; the highest value of tooth curvature was extrapolated at tooth-level.
Statistical analysis included the description of categorical (absolute and relative frequencies) and continuous variables (mean, standard deviation, range and median) for the total sample, differentiating by outcome (favourable/unfavourable). Simple binary logistic regression models were performed to study probability of failure according to independent variables. Non-adjusted odds ratio (OR) and 95% confidence intervals (CI) were obtained. Relevant variables (p <0.1) were selected to enter into a multiple model and adjusted OR were obtained. A receiver operating characteristic curve, corresponding area under curve and indexes and rates of diagnostic and predictive validity were obtained in order to check the reliability of the model as a predictive tool. Chi-squared tests and Mann-Whitney U tests were used to study the association between race and clinical variables. All variables showing differences by race were entered into a multiple binary logistic model in order to assess their potential confounding effects. A 5% significance level was used and a logistic model reached power at 96% in order to detect OR = 2.5 in proportions of the binary outcome between two groups at a confidence interval of 95%. Analogously, power was estimated at 80% in order to detect OR = 2.0 in proportions (25% versus 40%).
Results
A total of 148 teeth from the four clinical trials were excluded due to missing data on patient/operator race, socioeconomic background, or because the patient had more than one tooth treated (see online Supplementary Information and Figure 1). Data from 301 patients were available. Of these patients, 43 were Black (14.3%), 50 were NBME (16.6%), 208 were white (69.1%), 193 were women (64.1%) and 108 were men (35.9%), with an average age of 44.8 ± 13.7 years. A total of 152 cases (50.5%) were primary root canal treatments and 149 (49.5%) were root canal retreatments.
In total, 86% of treated teeth were molars, 9.6% were premolars, 4% were incisors and 0.3% (one case) was a canine. Furthermore, 51.5% of teeth were in the maxilla and 48.5% in the mandible, with first molars as the most frequently treated teeth (65.4%). Patients presented pre-operatively with symptoms in 53.2% of cases, sinus tracts in 12.8% and buccal swellings in 2.4% of cases. Additionally, 76.1% of teeth also showed pre-operative radiolucencies and intra-operative perforations were reported in 2.4% of cases; 50.5% were treated in one visit and 49.5% in two visits.
The mean tooth curvature was 26.4 ± 11.4 and tooth length was 20.4 ± 2.0. Root canal obturations were judged as flush in 65.5% of the cases, while 21.3% were classified as long and 12.2% short.
Moreover, 78.7% of treated teeth (n = 237) were classified as having a favourable outcome (95% CI: 74.1-83.4%). Reciprocally, there were 21.3% (n = 64) with an unfavourable outcome (95% CI: 16.6-25.9%). Outcome varied according to race, with NBME patients having the highest percentage of an unfavourable outcome at 32%, followed by Black patients at 27.9% and white patients with the lowest percentage of 17.3% (Fig. 2).
The data was subsequently analysed according to all variables using a simple logistic regression model (Tables 3 and 4). NBME patients showed a significantly increased risk of an unfavourable outcome (OR = 2.25; p = 0.0022) compared to white patients, with a 125% increased risk. Black patients also had increased odds of an unfavourable outcome (OR = 1.85; p = 0.111) compared to white patients, but statistical significance was not reached.
The outcome was also influenced by the length of the root canal filling (p = 0.005). If the root canal obturation was short, the risk of an unfavourable result increased more than three times compared to flush root canal obturations (OR = 3.36; p = 0.002). There were, however, similar outcomes of flush and long root canal obturations (p = 0.991).
The presence of a pre-operative radiolucency significantly increased the risk an unfavourable outcome (OR = 2.59; p = 0.019). When radiolucencies were detected, the risk increased more than 2.5 times. Intra-operative perforations also significantly increased the likelihood of an unfavourable result (OR = 5.25; p = 0.016). No aspect of the medical history influenced the likelihood of an unfavourable outcome (p >0.05).
A multiple regression model was conducted to analyse the outcome and the four independent variables: race, presence of a pre-operative lesion, short root canal filling and perforation (Table 5). Black patients showed a twofold increased risk of an unfavourable outcome (OR = 2.28; p=0.05) while NBME patients had a three times higher risk (OR = 3.07; p = 0.008) compared to white patients. The presence of a pre-operative radiolucency, short root canal filling and intra-operative perforation remained as significantly bad prognostic factors.
Further analysis was carried out to describe all the variables according to the race categories in order to look at the association of race with the clinical status of the tooth and patients profile (see Table 5 and online Supplementary Information). Socioeconomic status was associated with race (p <0.001), with white patients having a higher SES compared to Black and NBME patients. White patients more frequently presented with a pre-operative lesion (p = 0.001) and had more root filings which were long (p = 0.001). Black and NBME patients also underwent a higher proportion of primary treatments (p <0.001), with Black patients having a higher proportion of teeth treated in the mandibular region compared to other groups (p = 0.027). Black patients were also found to undergo coronal coverage restoration of the tooth less often (p = 0.015).
The multiple model was extended to include all the relevant factors discriminating between race categories (see online Supplementary Information).
The four key variables remained as significant (perforation, pre-operative lesion and short root filling). Black patients' risk of an unfavourable outcome was almost three times higher (OR = 2.99; p = 0.028) compared to white patients and NBME patients were more than four times at risk (OR = 4.51; p = 0.002) compared to white patients.
Discussion
The results of this study showed that endodontic treatments in Black and NBME patients had a significantly higher failure rate compared to white patients.
The failure rates shown in this study (21.3%) are similar to those of other CBCT outcome studies on the outcome of root canal treatments.6 In agreement with previous literature, root canal fillings which were short in length, the presence of a pre-operative lesion and the occurrence of intra-operative perforations were associated with a significantly higher chance of an unfavourable outcome.
Endodontic treatment is a complex procedure, requiring time and skill, and such operator abilities and experience affects the success of endodontic treatments.3,30 In this study, all operators were endodontic postgraduate students who had been specifically trained and standardised in the technical procedures involved in the four clinical trials. It should also be noted that a higher percentage of Black and NBME patients received primary treatments which was been shown to have a slightly higher success rate (though not statistically significant) compared to retreatment cases26,31 and that there was a lower proportion of Black and NBME patients with pre-operative radiolucencies, which does affect the success of root canal retreatment.3,26These patients also had, overall, a better result in terms of root canal obturation length, with an 82.2% of flush root canal obturations, whereas white patients had a similar result in only 58.3% of the cases.
Limits of the present work include its retrospective nature and the results should be considered as exploratory and need to be confirmed prospectively. The four studies had different primary outcomes, namely: assessing the outcome of root canal retreatments using CBCT in general;25 the assessment of the outcome of root canal retreatments of teeth with different volumes of residual tooth structure; the comparison of the outcome of primary root canal treatments undertaken with either single cone calcium silicate sealer or warm vertical condensation and epoxy-resin sealer;23 and the comparison of a super-sterile infection control protocol with a conventional protocol.24
Despite these limitations, the inclusion and exclusion criteria were similar and so were the overall proportions of successful outcomes in the four studies.
Variations in dental disease between minority ethnic groups are established which largely have been attributed to social inequalities.32 While all treatments carried out in this study were free of charge and travel costs to the clinic for those involved in the studies are reimbursed, thereby limiting the effect that SES may have, it is acknowledged that there will also be indirect costs - such as the ability to take time off work or access to childcare - which are more likely to impact those with lower SES. This said, the treatments compared have similar timeframes and were completed in one or two visits, which suggests that low SES is less likely to be the reason that one treatment is favoured over another. In addition, SES itself was not associated with a worse outcome of root canal treatments in general. Often, disparities in health care outcomes are justified by other baseline factors, such as medical history or periodontal and caries status. In this study, all cases with severe periodontal disease had been excluded from all four trials, while caries activity was never found to be a relevant factor in determining the outcome of endodontic treatments.
Medical history was shown to have no effect on the outcome of treatment, though it is well documented that diabetes can affect the success of endodontic treatments.33 Impaired, non-specific immune response also significantly lowers success rates, as well as smoking.34,35 In all four studies, however, any patient presenting with immunosuppression were excluded and all diabetic patients were controlled through medication or diet, so this is unlikely to have had any affect upon outcome. It is worth noting, however, that the different racial backgrounds of patients may be associated with differences in the immunologic and inflammatory response to bacterial infection.36
Differences in oral health care outcomes between ethnicities do exist and a range of suggestions have been made to account for them. These include differences in oral health knowledge37 and low levels of attendance at dental clinics, despite relatively high levels of dental need.38 In a study exploring ethnic inequalities in access to and outcomes of healthcare, Nazroo et al. (2009) found that while minority ethnic groups made good use of primary care services, reflecting the findings of earlier studies,39,40 they were less likely to use hospital services and there were 'marked inequalities in the use of dental care'. This may be due to ethnic differences in the use of private healthcare,39 to difficulties finding NHS dental services or paying the fees associated with dental care.38 Again though, these differences can largely be accounted for when controlling for SES, suggesting they are linked to the wider social determinants of oral health.41,42 Bastos et al. (2020) also suggest that few papers that look at race-based differences in oral heath also take into account SES and the ways in which the two interact.43
The discrepancies in outcome data reported in this paper persist, suggesting that one of the social determinants, alongside SES, that needs to be addressed is racial bias. The link between the patient's race and the outcome of endodontic treatments may be the result of stereotypes held by providers, resulting in unconscious bias, even though one does not display conscious prejudice or discrimination.44
It is well documented that such stereotypes exist, with data showing that white people view Black, Hispanic and Asian people in a more negative light than they do themselves. For example, 29% of white people were shown to agree with the statement that most Black people are unintelligent and even more violent.45 This is the belief of race science, which has been widely debunked by research and has been shown to hold no basis in scientific fact.46 In certain conditions whereby there are time pressures, emotional responses, such as anger or anxiety, or even an overload of information, these stereotypes can be activated and in turn, can affect behaviour.47
As previously stated, there is limited research on the differences in dental care among minority ethnic groups. There is even less evidence on whether biases affect patient care; however, Patel (2018) showed that whether a patient received extraction or root canal treatment was strongly related to race.48 Clinicians were also shown to have a pro-white bias when tested with a brief implicit association test, suggesting that such biases could affect treatment planning decisions among dentists.
Strategies to counter these outcomes need to be implemented, for example, unconscious bias training and cultural competency training should be made more routinely available. It is also key for individuals to understand that self-reflection and self-critique is required to develop and to acknowledge that each patient has their own culture and uniqueness. This understanding of patient belief systems can in turn become essential and can improve their level of care.49 Together with regular assessments and analysis of outcomes, we can ensure that there is a long-term positive change.
In order for healthcare professionals to deliver objective care, they must be aware of any potential negative associations with specific groups.50 It is our obligation to challenge these ideas, particularly when it is contributing to health inequalities. Further work into making healthcare professionals aware of biases and investigation into strategies to reduce them should be paramount.
Conclusion
Black and NBME patients had a significantly higher failure rate of root canal treatments compared to white patients. Dentists should be aware of the higher chances of failure associated with the treatment of Black and NBME patients and take extra care in following endodontic treatment protocols in order to correct this discrepancy.
References
Dentistry. Root canal treatment claims jump 42% in the last five years. 2016. Available at https://dentistry.co.uk/2016/02/09/root-canal-treatment-claims-on-the-up/ (accessed November 2022).
Strindberg L. The Dependence of the Results of Pulp Therapy on Certain Factors - An Analytical Study Based on Radiographic and Clinical Follow-Up Examinations. Acta Odontol Scand 1956; 14: 1-175.
Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod 1990; 16: 498-504.
Ng Y-L, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int Endod J 2011; 44: 583-609.
Kanagasingam S, Lim C X, Yong C P, Mannocci F, Patel S. Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J 2017; 50: 417-426.
Liang Y-H, Li G, Wesselink P R, Wu M-K. Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod 2011; 37: 326-331.
Al-Nuaimi N, Patel S, Austin R S, Mannocci F. A prospective study assessing the effect of coronal tooth structure loss on the outcome of root canal retreatment. Int Endod J 2017; 50: 1143-1157.
Patel S, Wilson R, Dawood A, Foschi F, Mannocci F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography - part 2: A 1-year post-treatment follow-up. Int Endod J 2012; 45: 711-723.
Betancourt J R, Maina A W. The Institute of Medicine Report 'Unequal Treatment': Implications for academic health centres. Mt Sinai J Med 2004; 71: 314-321.
Smedley B D, Stith A Y, Nelson A R. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. 2003. Available at http://www.nap.edu/openbook.php?isbn=030908265X (accessed November 2022).
Petersen L A, Wright S M, Peterson E D, Daley J. Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Med Care 2002; DOI: 10.1097/00005650-200201001-00010.
Shavers V L, Brown M L. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst 2002; 94: 334-357.
Akinyemiju T, Meng Q, Vin-Raviv N. Race/ethnicity and socio-economic differences in colorectal cancer surgery outcomes: analysis of the nationwide inpatient sample. BMC Cancer 2016; 16: 715.
Soneji S, Tanner N T, Silvestri G A, Lathan C S, Black W. Racial and Ethnic Disparities in Early-Stage Lung Cancer Survival. Chest 2017; 152: 587-597.
Watson M, Grande D, Radhakrishnan A, Mitra N, Ward K R, Pollack C E. Racial Differences in Prostate Cancer Treatment: The Role of Socioeconomic Status. Ethn Dis 2017; 27: 201-208.
Flores G, Escala M E, Hall B G. Dead wrong: the growing list of racial/ethnic disparities in childhood mortality. J Paediatr 2015; 166: 790-793.
MBRRACE-UK. Saving Lives, Improving Mothers' Care. 2018. Available at https://www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202018%20-%20Web%20Version.pdf (accessed November 2022).
Evans C A, Smith P D. Effects of Racism on Oral Health in the United States. Community Dent Health 2021; 38: 138-141.
Kranz A M, Opper I M, Oestrada-Darley I, Goldstein E, Stein B D, Dick A W. Outcomes Associated With State Policies Enabling Provision of Oral Health Services in Medical Offices Among Medicaid-enrolled Children. Med Care 2021; 59: 513-518.
Jamieson L, Peres M A, Guarnizo-Herreño C C, Bastos J L. Racism and oral health inequities; An overview. EClinicalMedicine 2021; 34: 100827.
Murray C. Human Diversity: The Biology of Gender, Race, and Class. New York: Twelve, 2020.
Flanagin A, Frey T, Christiansen S L. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA 2021; 326: 621-627.
Zavattini A, Knight A, Foschi F, Mannocci F. Outcome of Root Canal Treatments Using a New Calcium Silicate Root Canal Sealer: A Non-Randomized Clinical Trial. J Clin Med 2020; 9: 782.
Zahran S. The Impact of an Enhanced Infection Control Protocol on Molar Root Canal Treatment Outcome - A Randomised Clinical Trial. Int Endod J 2021; 54: 1993-2005.
Davies A, Patel S, Foschi F, Andiappan M, Mitchell P J, Mannocci F. The detection of periapical pathoses using digital periapical radiography and cone beam computed tomography in endodontically retreated teeth - part 2: a 1 year post-treatment follow-up. Int Endod J 2016; 49: 623-635.
Al-Nuaimi N, Patel S, Davies A, Bakhsh A, Foschi F, Mannocci F. Pooled analysis of 1-year recall data from three root canal treatment outcome studies undertaken using cone beam computed tomography. Int Endod J 2018; DOI: 10.1111/iej.12844.
Office for National Statistics. English indices of deprivation 2019. 2019. Available at https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed November 2022).
UK Government. List of ethnic groups. 2021. Available at https://www.ethnicity-facts-figures.service.gov.uk/style-guide/ethnic-groups (accessed April 2022).
Löst C. Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921-930.
Weiger R, Axmann-Krcmar D, Löst C. Prognosis of conventional root canal treatment reconsidered. Endod Dent Truamatol 1998; 14: 1-9.
Ng Y-L, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: A systematic review of the literature. Int Endod J 2010; 43: 171-189.
Race Equality Foundation. Oral health and access to dental services for people from Black and minority ethnic groups. 2013. Available at http://raceequalityfoundation.org.uk/wp-content/uploads/2018/03/health_briefing_29-1_0.pdf (accessed November 2022).
Nagendrababu V, Segura-Egea J J, Fouad A F, Pulikkotil S J, Dummer P M H. Association between diabetes and the outcome of root canal treatment in adults: an umbrella review. Int Endod J 2020; 53: 455-466.
Marending M, Peters O A, Zehnder M. Factors affecting the outcome of orthograde root canal therapy in a general dentistry hospital practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 119-124.
Doyle S L, Hodges J S, Pesun I J, Baisden M K, Bowles W R. Factors affecting outcomes for single-tooth implants and endodontic restorations. J Endod 2007; 33: 399-402.
Caires N C M, Espaladori M C, Tavares W L F, de Brito L C N, Vieira L Q, Sobrinho A P R. Influence of genetic regulatory effects modified by environmental immune activation on periapical disease. Braz Oral Res 2019; DOI: 10.1590/1807-3107bor-2019.vol33.0109.
Babu S, Bhat R V, Kumar P U et al. A comparative clinico-pathological study of oral submucous fibrosis in habitual chewers of pan masala and betelquid. J Toxicol Clin Toxicol 1996; 34: 317-322.
Nazroo J Y, Falaschetti E, Pierce M, Primatesta P. Ethnic inequalities in access to and outcomes of healthcare: Analysis of the Health Survey for England. J Epidemiol Community Health 2009; 63: 1022-1027.
Nazroo J Y. The health of Britain's ethnic minorities: findings from a national survey. London: Policy Studies Institute, 1997.
Rudat Kai. Black and Minority Ethnic Groups in England. London: Health Education Authority, 1994.
Watt R G, Sheiham A. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol 2012; 40: 289-296.
Watt R G. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol 2007; 35: 1-11.
Bastos J L, Constante H M, Celeste R K, Haag D G, Jamieson L M. Advancing racial equity in oral health (research): more of the same is not enough. Eur J Oral Sci 2020; 128: 459-466.
Patel N, Patel S, Cotti E, Bardini G, Mannocci F. Unconscious Racial Bias May Affect Dentists' Clinical Decisions on Tooth Restorability: A Randomized Clinical Trial. JDR Clin Trans Res 2019; 4: 19-28.
National Research Council, Division of Behavioural and Social Sciences and Education, Committee on Population, Panel on Race, Ethnicity and Health in Later Life. Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda. In Bulatao R, Anderson N B (eds) Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda. Washington: National Academies Press, 2004.
Fredrickson G M. Racism: A Short History. Princeton: Princeton University Press, 2015.
Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Int Med 2007; 22: 882-887.
Patel N, Patel S, Cotti E, Bardini G, Mannocci F. Unconscious Racial Bias May Affect Dentists' Clinical Decisions on Tooth Restorability: A Randomized Clinical Trial. JDR Clin Trans Res 2019; 4: 19-28.
Juarez J A, Marvel K, Brezinski K L, Glazner C, Towbin M M, Lawton S. Bridging the gap: a curriculum to teach residents cultural humility. Fam Med 2006; 38: 97-102.
Ashton C M, Haidet P, Paterniti D A et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med 2003; 18: 146-152.
Acknowledgements
The authors thank Juan Luis Gómez Martínez (St Halley Statistics) for his valuable help in the statistical analysis of the data used in this study.
Author information
Authors and Affiliations
Contributions
Neha Patel: investigation, data curation and writing - original draft. Sasha Scambler: writing - review and editing and supervision. Mohammadreza Ranjbari: investigation and data curation. Mohammad Alhammad: investigation, data curation and formal analysis. Abdulaziz Bakhsh: investigation and data curation. Francesco Mannocci: conceptualisation, methodology, writing - review and editing and supervision.
Corresponding author
Ethics declarations
The authors whose names are listed above certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honouraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
This research was undertaken with the understanding and written consent of each participant and according to the Declaration of Helsinki 2008. Ethical approval to extract and analyse data from four studies were granted by NRES London Bridge and Dulwich Research Ethics Committees (20/WM/0013), NRES West London Research Ethics Committees (13/LO/1171) and NRES Westminster Research Ethics committee (08/H0804/79).
Supplementary Information
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2022
About this article
Cite this article
Patel, N., Scambler, S., Ranjbari, M. et al. The influence of patient race on the outcome of endodontic treatments: a pooled analysis of one-year recall data from four cone beam computed tomography outcome studies. Br Dent J (2022). https://doi.org/10.1038/s41415-022-5335-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-5335-y