Abstract
Introduction Children requiring a general anaesthetic (GA) for caries-related dental extractions are at high risk of developing new dental caries. It is therefore important to maximise opportunities for prevention.
Aim To explore the use and scope for fissure sealants among children requiring caries-related dental extractions under GA and investigate ongoing oral health support following treatment under GA.
Methods Service evaluation (baseline at GA and two years later) including dental examination and structured interview questionnaires, involving children (aged five to 15 years) attending Birmingham Dental Hospital for caries-related dental extractions under GA.
Results Of 352 children, 62.5% had at least one sound and sealable first permanent molar at the time of the GA (77% of 6-8-year-olds). Of those that could be followed up two years later (39), 5% had clinical evidence of sealants in first permanent molars. Two thirds saw a dentist after the GA and, of these, 85% had received oral hygiene instruction, 77% dietary advice and 15% application of fluoride varnish. One third presented with untreated dentine caries in at least one first permanent molar recorded as sound at baseline.
Conclusion There is an unmet need for preventive treatments, particularly sealants, in this high-risk group. The two-year incidence of caries in first permanent molars that are sound at the time of the GA is high. There may be scope for the provision of fissure sealants as part of the GA encounter.
Similar content being viewed by others
Key points
-
Highlights an unmet need for preventive treatments, particularly sealants, in children requiring caries-related GA extractions.
-
Reports the two-year incidence of caries in first permanent molars that were sound at the time of the GA is high.
-
Suggests there may be scope for the provision of fissure sealants in secondary care, as part of the GA encounter.
Introduction
Dental treatment under GA remains the most common reason for hospital admissions for children aged five to nine years in England.1The frequency of repeat GA for caries-related dental extractions is also relatively high.2,3,4 Research highlights the importance of a more proactive approach to prevention in these children.2,3,5,6,7 Aggressive treatment of caries at the time of the GA, education of parents and active follow-up are thought to be key factors to achieve the best outcomes following dental treatment under GA.8
Unfortunately, some of the affected families may have unfavourable oral health-related attitudes and behaviours including low compliance with follow-up appointments.9,10,11 Furthermore, though there appears to be a general under-utilisation of dental services among this high-risk group, the oral health support received by these children also appears to be low.5,6,7,12,13,14 Studies exploring parents' opinions on the delivery of oral health care for children referred for dental treatment under GA suggest preventive advice was inconsistent and treatment inadequate.6,7,12,13 A survey of dental GA providers in Yorkshire and Humber reported that over half of providers failed to mention the need for further preventive care in discharge letters sent back to referring dentists.15 Another study to investigate referring general dental practitioners' (GDP) views on promoting better oral health for their patients, concluded 'challenges on all fronts', due to which, many of these children were being failed on 'multiple levels'.14
Studies reporting on preventive care for children requiring dental treatment under GA often focus on advice and interventions received before the GA, but it is equally important to examine the support provided afterwards. This should help to identify any gaps in care and inform decisions on developing services to optimise the delivery of preventive measures to these children. The GA care pathway itself may present an op portunity to gain access to this high-risk group and deliver preventive care. One possible option is to provide fissure sealants in the context of the GA encounter. Fissure sealants have been shown to be both efficacious and cost-effective,16,17 and professional guidelines support their use in high caries risk children.18,19 One specific advantage of fissure sealants in this context is that this is a preventive treatment that can be delivered in a single appointment and it does not primarily rely on a behaviour change on behalf of the child or their family.
Birmingham Dental Hospital (BDH) provides a paediatric dental GA service to the area covered by the Birmingham and Solihull primary care trusts (PCT) cluster, but also accepts referrals from the wider West Midlands. This includes an exodontia (extractions only) service, often referred to as the short chair GA (which constitutes the major aspect of the paediatric dental GA service at this hospital), as well as comprehensive dental rehabilitation (including restorative treatment and sealants) under a longer day stay procedure, for children with physical, learning or behavioural comorbidities. A small number of general hospitals also provide a paediatric dental GA service in other areas of the West Midlands (including Sandwell, Walsall and Wolverhampton) and the Birmingham Children's Hospital manages children with complex medical problems.
About 2,000 children each year are seen at the BDH for dental extractions under a GA. Children are clinically assessed on a separate appointment before the GA appointment, where a treatment plan is agreed and consent is obtained. Radiographs are taken if deemed necessary by the assessing clinician. No restorative care is provided under a chair GA and children are discharged back to their referring GDP for subsequent care.
In order to explore the scope for providing fissure sealants as part of the GA encounter, we conducted a service evaluation to evaluate: i) the prevalence of first permanent molars that would be suitable to receive fissure sealants; ii) the oral health support and treatment received in primary care within two years following the GA appointment; and iii) the two-year incidence of caries in first permanent molars that were deemed suitable for fissure sealants at the time of the GA.
Baseline evaluation
Methods
Guidance was sought from the National Research Ethics Service (NRES), now part of the Health Research Authority, on the need for ethics approval; we were advised the project should be 'deemed as service evaluation', and so it was registered as such, with the Birmingham Dental Hospital (Birmingham Community Healthcare NHS Trust), registration number: 44/178.
Children aged five to 15 years who had been referred to the Birmingham Dental Hospital for caries-related dental extractions under a GA were included. Younger children were excluded, as they were unlikely to have erupted first permanent molars.
A separate pre-GA assessment appointment was only introduced in 2014, so at the time of the baseline evaluation (2012), children had GA extractions completed at the same visit. During this appointment, one of the clinicians undertaking GA assessments (SEK) was required, as part of the clinical dental examination, to collect data on the condition of first permanent molars. Where possible, teeth were dried with a 3-in-1 syringe and each first permanent molar was classified, as either unerupted/partially erupted, sound and fissure sealable, carious (including early or suspect lesions), restored, fissure-sealed, hypomineralised and/or hypoplastic, scheduled for extraction, missing (previously extracted) or other. Data were collected on case report forms (CRF) and, if appropriate, more than one option could be selected for each molar. However, the sound and sealable option was restricted to teeth that were free from any clinical signs of active caries including any visual changes in enamel (such as white or brown decalcification) suggestive of early caries. The first 30 children were also examined by the project lead (AR) to advise on use of the scoring criteria and assess consistency in recording. No radiographs were taken for the purposes of this service evaluation but any available were referred to.
All parents were asked if they would be agreeable to be contacted by telephone and/or for their child to be recalled, up to two years after the GA. Parents were also invited to complete a self-administered questionnaire. Interpreters (booked for the GA assessment) could help parents with a poor grasp of English. The questionnaire assessed dental attendance behaviours, (including whether patients had a follow-up appointment arranged with their own dentist after the GA) as well as parents' views on the placement of sealants. Ethnicity data was self-reported. Postcode data were used to calculate index of multiple deprivation (IMD) scores,20 which were then related to deprivation deciles. Data collection was carried out over a period of six months from October 2012 to March 2013.
Results
A total of 352 patients with a mean age of 7.2 years were examined (Table 1). Most children were White British (35%) or Asian British Pakistani (40%) with high levels of deprivation (70% of children in the lowest quintile). Sixty-two percent of children (n = 220) had at least one sound and sealable first permanent molar at the time of the GA. Of these, 77% (n = 169) had all four first permanent molars rated as sealable. The proportion of children with sound and sealable first molars varied by age. For example, of 222 children aged six to eight years, 77% (n = 171) had at least one sealable first molar, 81% (n = 141) of whom had four sealable first molars. Only four children in the entire group (1.1%) presented with molars that were already sealed before the GA. Almost three-quarters (73%, n = 257) of parents agreed to be contacted after the GA; of the others, 15%, (n = 53) refused, including one parent of a child that had a sealable molar, and the remainder were 'not sure'.
A total of 214 parents of examined children completed the questionnaire (response rate, 60.8%) (Table 1). Among this group, 78% (n = 166) of children had been referred by a GDP, 16% (n = 35) by a community dental practitioner (CDP) and the remainder had self-referred. Forty-six percent (n = 98) of parents reported taking their child to a dentist for regular check-ups (at least once every six months), 27% (n = 57) for occasional check-ups and another 27% only when their child experienced trouble. At the time of the GA appointment, 15% (n = 33) of children had an appointment booked to see their dentist after the GA, although a further 29% (n = 61) and 16% (n = 35) of parents planned to take their child back to see a dentist within three months and six months of the GA, respectively. However, 29% (n = 61) were simply going to wait to hear from their dentist, while 11% (n = 24) of parents were either not sure or had no plans to take their child back to a dentist in the future. Ten percent (21/214) of children had previously had dental extractions under GA.
Overall, 89.3% (n = 191) of parents wanted their child to have sealants, whereas 8% (n = 18) did not want their child to have sealants, with the remainder being unsure. Of those who wanted sealants, 53% (n = 102) preferred their child to have sealants applied during the GA, 31% (n = 59) just before the GA, and 16% (n = 30) preferred sealants to be applied by their family dentist.
Two-year follow-up
Methods
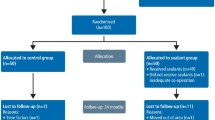
Two years after the GA, CRFs were used to identify children who presented with at least one 'sound and sealable' first permanent molar at the baseline evaluation, and whose parents had agreed to be contacted after the GA. On this basis, clinical (paper) records for 219 patients, were requested from the medical records department at BDH. Two searches retrieved 132 clinical files (60%).
Therefore, a total of 132 parents were sent invitation letters to attend a follow-up appointment. Where possible, non-responders were followed-up with a phone call. Failed appointments were followed up with a phone call and/or letter (Fig. 1). The follow-up included a clinical examination to assess caries experience and evidence of sealants in first permanent molars and parents were asked to complete a questionnaire to evaluate what oral care the child had received during the two years after the GA extractions.
Reviews were carried out by a single examiner (AR), either at the BDH or a community dental clinic. For the clinical examination, a 3-in-1 syringe was used to wash and dry the teeth and a ball-ended probe used to remove soft debris and check for minor cavitations or the presence of sealants. The presence or absence of caries and caries-related treatment (including evidence of sealants), was recorded using the ICDAS (International Caries Detection and Assessment System).21 The examiner had completed online training on the use of ICDAS.
Categories of caries reported on, were:
Any caries: ICDAS codes 1-6
Dentine caries: ICDAS codes 4, 5, 6
Severe caries: ICDAS codes 5, 6.
At the review visit, radiographs (if justified as part of the holistic assessment) were taken, dental students gave preventive advice and, if appropriate, topical fluoride application and sealant placement was offered. Alternatively, parents could choose to return to their child's usual dentist (if they had one) to have these carried out. Post-assessment letters were sent to dental practitioners and, where appropriate, these included a request for completion of any outstanding treatment and/or radiographs.
Follow-up visits were completed from October 2014 to June 2015. Appropriate summary statistics were calculated for the entire patient sample and for subgroups who completed the baseline questionnaire and attended for the follow-up two years later (STATA IC version 12, Stata Corp, College Station, USA).
Results
Overall, contact (by letter or phone call) was achieved with 54% (71/132) of families for whom records were available. Out of these, 63% (45/71) accepted the offer of a follow-up, of whom 87% (39/45) attended the appointment and agreed to complete the questionnaire. This means we saw 55% of the children whose parents could be contacted and 30% (39/132) of the children for whom records were available after two years.
Baseline demographic characteristics for the groups followed up were similar to the whole sample at baseline, except for ethnicity and IMD. Children with follow-up data were more likely to be from the poorest decile and from an Asian British Pakistani background (Table 1).
Of the 39 children attending for review, 92% (n = 36) had been referred for the GA by a primary care dental practitioner, but only 67% (n = 26) returned to see a dentist after the GA. In all cases, this was six months or longer after the GA. Of the 26 children that saw a dentist after the GA, almost three quarters (n = 19) reported to have a check-up once every six months, 19% (n = 5) once a year and the remainder (n = 2) only went to a dentist when having trouble. Most (96%, n = 25) saw a GDP with only one child (4%) being seen by a CDP.
With regards to the procedure for organising check-ups (for those that had received a check-up), 50% of parents (12 out of 24) reported receiving a 'contact us letter' from the dentist advising that a check-up was due. One quarter (n = 6) said an appointment was posted without prior notification and the remaining 25% suggested it was left up to them to contact the practice when they thought a check-up was required. Fifty-eight percent (n = 14) reported receiving reminders (text, phone call, letter) about scheduled appointments.
Table 2 shows the type of dental treatment and preventive advice received, as reported by parents. When asked if their child's dentist had emphasised the importance of prevention to avoid a repeat GA, 38.5% felt this had been done.
Of the 26 children that saw a dentist after the GA, 27% (n = 7) of parents believed their child was anxious about dental treatment and in two cases this anxiety had stopped the dentist from completing treatment that was planned. Only one parent out of seven felt the dentist had offered measures to reduce this anxiety and this was limited to behaviour management techniques.
Opinions on measures that might help parents to look after their child's teeth were wide ranging. Of the group followed-up (n = 39), 62% (n = 24), would have welcomed a reminder about dental appointments and 41% (n = 16) requested more frequent check-ups. Oral health leaflets and school-based programmes were more popular than DVDs or online resources. One third of parents (n = 13) would welcome advice on finding a child-friendly dentist (Table 3).
Clinical data at two years
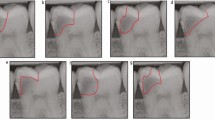
Of the 39 children examined at two years, two thirds (n = 25) presented with some degree of caries (ICDAS 1-6), one third (n = 13) with dentine caries (ICDAS 4-6) and one quarter (n = 9) with severe dentine caries (ICDAS 5-6) in at least one first permanent molar (Table 4). Of the 154 first permanent molars that had been sound and sealable at the time of the GA appointment, 16.9% (26 teeth) had untreated dentine caries (Table 4).
When examining which surfaces of teeth were most affected, of the 92 permanent molar surfaces affected by 'any' caries, 75% (n = 69) were occlusal, and 21% (n = 19) were buccal or palatal. Similarly, two-thirds (22/33) of the surfaces affected by dentine caries were occlusal. Two children (5%) presented with clinical evidence of sealants in first permanent molars and an equal number had fillings in at least one first permanent molar. One child had undergone caries-related extraction of permanent molars at the baseline GA.
Discussion
Our data on preventive care for children undergoing caries-related extractions under GA at Birmingham Dental Hospital highlight an unmet need for preventive treatments. Among the children that could be followed-up, approximately one in six first permanent molars that were caries-free at the time of the GA encounter presented with dentine caries two years later. At the time of the GA appointment, there was a large proportion of children with sealable first permanent molars, most of which did not receive sealants in primary care over a two-year period.
Only 61% of parents completed the baseline questionnaire, introducing scope for some bias and the difficulty in accessing clinical records significantly hampered our ability to contact families for review. We therefore welcome the fact that clinical records have since been transferred to a computer-based system, which should facilitate future efforts to contact patients. Fifty-five percent (39/71) of those that could be contacted, brought their child for the follow-up two years later, which seems reasonable, given that, two years on from the GA, many parents might not remember that they had agreed for their child to be recalled and many were already registered with a local dentist. Parents' ability to recall information accurately may be questionable as well as their understanding of dental treatment offered and provided by dentists. However, an attempt was made to validate parental responses on the provision of sealants by comparisons with clinical data, which suggested reasonable agreement from both sources.
The criteria used to identify and record the condition of first permanent molars at baseline were crude in comparison to ICDAS scoring. However, all baseline data were collected by a single examiner, minimising the scope for variation. Similarly, all data collection for the two-year follow-up visits (using ICDAS) was completed by a single (albeit different) examiner, who had previously instructed the baseline examiner on the application of the baseline scoring criteria. With respect to reporting on caries levels at the two-year review, the small number of children that could be followed-up, compared to the number seen at baseline, mean that any comparisons must be viewed with caution.
The group under investigation seemed representative of the national picture of children requiring GA extractions, in that most patients were seven years of age at the time of the GA.5,6,7,12,22 The sex distribution was also similar to that identified in other studies.5,22,23 Most families were resident in poorer socioeconomic areas, suggesting they were representative of the catchment area, given that Birmingham has high levels of deprivation, with 40% of the population residing in areas deemed to fall in the poorest decile.24 This also lends support to the widely-reported association between deprivation, dental caries and a child's need for extractions under GA.23,25,26 Interestingly, however, a relatively larger proportion (70.3%) of those that returned for a review were from the poorest socioeconomic decile. This seems surprising, given that this is the group we might least expect to attend a follow-up appointment. Children from a variety of ethnic backgrounds were attending for GA extractions; the ethnic profile at baseline was a fair representation of the child population in Birmingham, where around 40% of children are from an Asian background.24 However, of those that returned for a follow-up appointment, almost 60% were Asian British Pakistani, compared with 20% White British, suggesting Pakistani parents were more likely to accept the invitation to a follow-up appointment. This contrasts with past research which suggests that ethnic minorities are often infrequent attenders, due to perceived barriers to dental services such as language and cultural misunderstandings.27
Only 46% of children in the baseline sample were reported to be regular attenders. This is unfavourable compared to attendance behaviours reported in other studies6,12 and suggests ongoing care among this group is even less likely. For those that did return to see a dentist, this was six months or longer after the GA. This falls short of recommendations for high-caries-risk children to be followed-up more frequently.28 Three monthly fluoride applications are recommended for high-caries-risk children,18 which is clearly not feasible if they are only reviewed once every six months.
The provision of fissure sealants (5%) reported in our clinical evaluation was comparable to the UK National Child Dental Health (CDH) Survey which found that 7% of eight-year-olds had evidence of sealants.29 We would have expected a higher prevalence of sealants in our high-risk group. Since most children at the two-year follow-up were co-operative for dental treatment (as reported by parents), other factors are likely to explain this finding, which is consistent with previous studies.5,12
Our observations serve to reinforce earlier calls to maximise the use of fluorides and fissure sealants in high-risk children.12,13 Though the use of fluoride varnish in children by primary care dentists appears to be increasing, as reflected by NHS statistics (with a 20% increase from 2014-15 to 2015-16), fissure sealant applications during the same time have increased to a lesser extent (11%).30 Fissure sealants have been shown to be superior to fluoride varnish for the prevention of caries on occlusal surfaces,31 although this has recently been questioned,32 and might be more appropriate if patients are irregular attenders and unlikely to return for regular fluoride applications.
The two-year incidence of caries in first permanent molars following the dental GA was high. Although the results are not directly comparable with other oral health surveys (due in part to varying caries assessment tools), some degree of comparison is appropriate. A third of the children in our sample presented with untreated dentine caries in at least one first permanent molar two years after the GA, which compares poorly with findings from the most recent UK CDH Survey,29 where one in ten children (9%) at the age of eight years had decay into dentine requiring treatment. This is not surprising and indicates that the need for a dental GA identifies a high-risk population. We also confirmed that occlusal surfaces of permanent molars are most vulnerable to caries.33,34
Clearly, more must be done to prevent new caries among high-risk children following dental extractions under GA. The GA care pathway itself may offer an opportunity to gain access to this high-risk group. Fissure sealants can be carried out under GA; in some units, this service is already provided, where sealants are undertaken as part of a comprehensive programme of dental rehabilitation under intubated GA and is often restricted to patients that are medically compromised or have special care needs. Alternative options are to carry out sealants during the pre-GA assessment appointment, at a separate prevention visit or at a follow up appointment after the GA. A study in London found that 55% of parents would welcome an oral health programme during their pre-assessment clinic6 and, Goodwin et al.4 have reported on a prevention clinic at one hospital in the northwest of England, which parents had to attend before their child could have GA extractions.Intervention prior to the GA seems more appropriate, given that patients may not return after the GA and children might be more anxious because of the GA experience. Whilst capitalising on the opportunity afforded by the GA assessment visit might be the most convenient option, children could also return to their 'family dentist' to have sealants provided, though again, it would be more beneficial for these to be carried out before the GA extractions. Research is required to establish the reason(s) for the unmet need for sealants and further work on closer collaboration between GA centres and referring practitioners might help facilitate delivery of the prevention needed.
This calls for a more proactive approach to prevent new caries in these vulnerable children.6 Our challenge is to develop interventions to maximise the delivery of evidence-based caries preventive measures to this high-risk group. One possible option is to take advantage of the opportunity presented by the GA encounter in secondary care, as a large proportion of children have sealable permanent molars, a significant proportion of which later develop fissure caries in this high-risk population.
Conclusions
This local evaluation suggests that children requiring caries-related GA extractions do not receive adequate oral health care support and caries preventive interventions, neither before nor after the GA. Although oral hygiene instruction and dietary advice had been offered, the use of fissure sealants and topical fluoride application appears to be very low. This is of concern given that many of these children were apparently regular dental attenders and according to their parents not unduly anxious about dental treatment. Consequently, the risk of future caries in permanent teeth remains high. The GA encounter in secondary care in Birmingham could present an opportunity to deliver fissure sealants in this high-risk population.
References
Royal College of Surgeons: Faculty of Dental Surgery. The state of children's oral health in England. London: Faculty of Dental Surgery, 2015. Available at https://www.rcseng.ac.uk/-/media/files/rcs/about-rcs/government-relations-consultation/childrens-oral-health-report-final.pdf (accessed August 2019).
Harrison M, Nutting L. Repeat general anaesthesia for paediatric dentistry. Br Dent J 2000; 189: 37-39.
Albadrii S S, Jarad F D, Lee G T, Mackie I C. The frequency of repeat general anaesthesia for teeth extractions in children. Int J Paediatr Dent 2006; 16: 45-48.
Goodwin M, Sanders C, Pretty I A. A study of the provision of hospital based dental general anaesthetic services for children in the northwest of England: Part 1- a comparison of service delivery between six hospitals. BMC Oral Health 2015; 15. 50.
Kakaounaki E, Tahmassebi J F, Fayle S A. Further dental treatment needs of children receiving exodontia under general anaesthesia at a teaching hospital in the UK. Int J Paediatr Dent 2006; 16: 263-269.
Olley R C, Hosey M T, Renton T, Gallagher J. Why are children still having preventable extractions under general anaesthetic? A service evaluation of the views of parents of a high caries risk group of children. Br Dent J 2011; 210: E13.
Aljafari A K, Scambler S, Gallagher J E, Hosey M T. Parental views on delivering preventive advice to children referred for treatment of dental caries under general anaesthesia: A qualitative investigation. Community Dent Health 2014; 31: 75-79.
Sheller B, Williams B J, Hays K, Mancl L. Reasons for repeat dental treatment under general anaesthesia for the healthy child. Paediatr Dent 2003; 25: 546-552.
Amin M S, Harrison R L. A conceptual model of parental behaviour change following a child's dental general anaesthesia procedure. Paediatr Dent 2007; 29: 278-286.
Jamieson W J, Vargas K. Recall rates and caries experience of patients undergoing general anaesthesia for dental treatment. Paediatr Dent 2007; 29: 253-257.
Hosey M T, Ashbury A J, Bowman A W et al. The effect of transmucosal 0.2 mg/kg midazolam premedication on dental anxiety, anaesthetic induction and psychological morbidity in children undergoing general anaesthesia for tooth extraction. Br Dent J 2009; 207: E2.
Karki A J, Thomas D R, Chestnutt I G. Why has oral health promotion and prevention failed children requiring general anaesthesia for dental extractions? Community Dent Health 2011; 28: 255-258.
Goodwin M, Pretty I A, Sanders C. A study of the provision of hospital based dental General Anaesthetic services for children in the North West of England: Part 2 - the views and experiences of families and dentists regarding service needs, treatment, and prevention. BMC Oral Health 2015; 15: 47.
Aljafari A K, Gallagher J E, Hosey M T. Failure on all fronts: general dental practitioners' views on promoting oral health in high caries risk children - a qualitative study. BMC Oral Health 2015; 15: 45.
Ni Chaollai A, Robertson S, Dyer T A, Balmer R C, Fayle S A. An evaluation of paediatric dental general anaesthesia in Yorkshire and the Humber. Br Dent J 2010; 209: E20.
Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington H V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev 2017; CD001830. DOI: 10.1002/14651858.CD001830.pub5.
Bhuridej P, Kuthy R A, Flach S D, Heller K E, Dawson D V, Kanellis M J, Damiano PC: Four-year cost-utility analyses of sealed and nonsealed first permanent molars in Iowa Medicaid-enrolled children. J Public Health Dent 2007; 67: 191-198.
Public Health England. Delivering better oral health: an evidence-based toolkit for prevention. 3rd ed. London: Public Health England, 2017. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed August 2019).
Scottish Dental Clinical Effectiveness Programme: Prevention and management of dental caries in children: dental clinical guidance. 2nd ed. Dundee: SDCEP, 2018. Available at http://www.sdcep.org.uk/wp-content/uploads/2018/05/SDCEP-Prevention-and-Management-of-Dental-Caries-in-Children-2nd-Edition.pdf (accessed August 2019).
Ministry of Housing, Communities & Local Government. English indices of deprivation 2015. Available at http://imd-by-postcode.opendatacommunities.org/ (accessed August 2019).
International Caries Classification and Management System. Available at https://www.iccms-web.com (accessed August 2019).
Raja A, Daly A, Harper J, Senghore N, White D, Ravaghi V. Characteristics of children undergoing dental extractions under general anaesthesia in Wolverhampton: 2007-2012. Br Dent J 2016; 220: 407-411.
Hosey M T, Bryce J, Harris P, McHugh S, Campbell C. The behaviour, social status and number of teeth extracted in children under general anaesthesia: A referral centre revisited. Br Dent J 2006; 200: 331-334.
Birmingham City Council. Population and census. Available at https://www.birmingham.gov.uk/info/20057/about_birmingham/1294/population_and_census (accessed August 2019).
Prendergast M J, Beal J F, Williams S A. The relationship between deprivation, ethnicity and dental health in 5-year-old children in Leeds UK. Community Dent Health 1997; 14: 18-21.
Locker D. Deprivation and oral health: a review. Community Dent Oral Epidemiol 2000; 28: 161-169.
Newton J T, Thorogood N, Bhavnani V, Pitt J, Gibbons D E, Gelbier S. Barriers to the use of dental services by individuals from minority ethnic communities living in the United Kingdom: findings from focus groups. Prim Dent Care 2001; 8: 157-161.
National Institute for Health and Care Excellence. Dental checks: intervals between oral health reviews. 2004. Available at https://www.nice.org.uk/guidance/cg19 (accessed August 2019).
Health and Social Care Information Centre. Children's Dental Health Survey 2013. Report 2: Dental Disease and Damage in Children: England, Wales and Northern Ireland. 2015. Available at https://files.digital.nhs.uk/publicationimport/pub17xxx/pub17137/cdhs2013-report2-dental-disease.pdf (accessed August 2019).
NHS Digital. NHS dental statistics: England 2015-16. 2016. Available at https://files.digital.nhs.uk/publicationimport/pub21xxx/pub21701/nhs-dent-stat-eng-15-16-rep-v2.pdf (accessed August 2019).
Hiiri A, Ahovuo Saloranta A, Nordblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database Syst Rev 2010; CD003067. DOI: 10.1002/14651858.CD003067.pub3.
Chestnutt, I G, Playle R, Hutchings S et al. Fissure seal or fluoride varnish? a randomized trial of relative effectiveness. J Dent Res 2017; 96: 754-761.
King N M, Shaw L, Murray J J. Caries susceptibility of permanent first and second molars in children aged 5-15 years. Community Dent Oral Epidemiol 1980; 8: 151-158.
Carvalho J C, Ekstrand K R, Thylstrup A. Dental plaque and caries on occlusal surfaces of first permanent molars in relation to stage of eruption. J Dent Res 1989; 68: 773-779.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raja, A., White, D., Kerr, S. et al. Prevention in the context of caries-related extractions under general anaesthesia: an evaluation of the use of sealants and other preventive care by referring dentists. Br Dent J 227, 489–495 (2019). https://doi.org/10.1038/s41415-019-0729-1
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0729-1