Abstract
Introduction Consistent evidence has shown that periodontitis can be considered a risk factor for the development of vascular complications such as myocardial infarction and cerebrovascular accident. The majority of cases of erectile dysfunction (ED) are considered to result from the complication of vascular impairments. Therefore, it is conceivable to hypothesise that periodontitis can also be associated with ED.
Aims To determine whether a possible link between periodontitis and ED exists by reviewing and presenting the current available evidence.
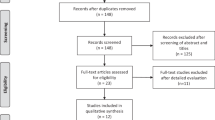
Methods Current, up to June 2018, case-control studies, randomised controlled trials (RCT) and meta-analyses were reviewed.
Results Nine case-control studies and three meta-analyses found significant positive associations between these two conditions, with odds ratios ranging from 1.53 to 5.94. Furthermore, one RCT found a significant improvement in subjective measurements of ED in patients treated for periodontitis.
Conclusions The current associations must be interpreted with caution because of the considerable heterogeneity of the cross-sectional investigations and the short-term character of the only RCT included. Nevertheless, the preliminary results can be taken into consideration for the general physician or the specialist in the motivation of the male patient to visit dental professionals and, if indicated, treated for periodontitis, which may help in managing the vasculogenic form of impotence.
Similar content being viewed by others
Key points
-
Provides a general overview of the relationship between periodontitis and most relevant forms of diseases of vasculogenic origin.
-
Describes generally the pathogenesis of the vasculogenic form of erectile dysfunction.
-
Reports a detailed description of the available scientific evidence regarding the link between periodontitis and erectile dysfunction.
Introduction
Since the last decade of the 1900s, periodontitis has been extensively investigated in relation with systemic diseases.1,2,3,4,5,6 Large epidemiological studies during the 1990s and the first decade of the twenty-first century reported consistent evidence which supported a positive association between periodontitis and systemic conditions such as: atherosclerotic cardiovascular diseases (ACVD); lung infections; rheumatoid arthritis (RA); premature and dysmature birth and other pregnancy complications; and diabetes mellitus type 2 (DM2). Nowadays, the body of evidence is solid enough to state that periodontitis could be considered as a risk factor for most of the above-mentioned diseases and, in particular, for ACVD and DM2.
Current evidence of a link between periodontitis and systemic diseases of vasculogenic origin
After DM2, ACVD is the most investigated systemic disease linked to periodontitis. ACVD is defined as: proven forms of atherosclerosis, acute ACVD events and/or conditions such as angina pectoris, myocardial infarction (MI, heart attack), a cerebrovascular accident (CVA, stroke), peripheral artery disease or death due to fatal heart attack or stroke. Longitudinal studies have reported that subjects affected by periodontitis at the start of the study showed a higher risk of at least 50% (relative risk 1.5) of developing an acute ACVD event in later life (either MI or CVA or death).7 This risk is even higher (twofold over one's 'normal' risk) for males <60 years of age.8
Several biological mechanisms have been proposed in order to explain the possible 'causal' link between ACVD and periodontitis.9 The contribution of inflammation appears to be central in the aetiopathogenesis of atherogenesis, and subsequently endothelial dysfunction and hypertension, which are the underlying cause of acute ACVD events.
Atherosclerosis is the result of a chronic inflammatory process of the intima and media of the arterial wall in the large and small arteries which leads to the formation of atherosclerotic plaques. This chronic inflammatory process leads to a decrease in elasticity of the blood vessel and an increase in thickness of the blood vessel wall. Thicker atherosclerotic plaques occur often in specific places in the arterial system, such as coronary arteries, or in the carotid arteries around the bifurcations of the common carotid artery towards the arteria carotis interna and externa. A meta-analysis found that periodontitis patients had a significant average increase of 0.08 mm of the intima media thickness of the arteria carotis interna.10 In addition to this, an intervention study found that patients with periodontitis showed a significant decrease in thickness of the intima media in the arteria carotis interna after successful periodontal therapy.11
Endothelial dysfunction can be assessed by measuring specific biomarkers in peripheral blood, or by measuring the stiffness of the arterial walls by means of the flow-mediated dilation (FMD), an ultrasonic measurement of the dilatation of an artery when blood flow increases in that artery. A meta-analysis based on seven cross-sectional studies found that patients with periodontitis had a significant average decrease of 5.1% in FMD.10 In addition to this, the authors of the same meta-analysis summarised the result of three investigations which measured the FMD in periodontitis patients after periodontal therapy and the results showed a significant average improvement of 6.6% in FMD.10
Another method to measure arterial stiffness is to measure the speed with which a pulse wave travels down the aortic artery (pulse wave velocity, PWV). An increase of PWV is an indication of a reduced elasticity of the arterial vessel. Although the evidence using this method is still limited, a Dutch investigation showed that patients with periodontitis had a significant increase in PWV compared to patients without periodontitis.12 More interestingly, an intervention study found an improvement in PWV after periodontal therapy in patients affected by both periodontitis and refractory hypertension.13
The measurement of blood pressure is the most common method to assess the condition of the blood vessels. A patient is affected by hypertension when they show a systolic blood pressure of ≥140 mmHg and diastolic blood pressure of ≥90 mmHg or they are using blood pressure lowering medications. Hypertension is an indicator of increased stiffness, endothelial dysfunction and atherosclerosis and increased risk for acute ACVD events. A meta-analysis based on 17 cross-sectional studies found that periodontitis patients had a 50% higher risk (odds ratio of 1.5) of hypertension in comparison with subjects with a healthy periodontium.14 A Brazilian intervention study in patients with refractory hypertension and periodontitis showed a significant reduction of blood pressure at six months after periodontal therapy (from 175 to 157 mmHg and from 105 to 95 mmHg for systolic and diastolic blood pressure, respectively).15 In addition, a Dutch treatment study in patients with periodontitis, but without specifically high blood pressure or other comorbidities, also showed a reduction in systolic blood pressure up to one year after successful periodontal therapy.15
Characteristics of erectile dysfunction
Erection normally occurs as a result of a neurovascular phenomenon characterised by an increase in the arterial flow within the hypogastric-penile bed followed by the subsequent activation of the veno-occlusive mechanism of the corpora cavernosa. Erectile dysfunction (ED) is defined as the persistent inability (longer than three months) of the male to attain and continue a penile erection sufficient for satisfactory sexual intercourse.16 The prevalence of ED increases with age. In the US, the prevalence in men age 40-49 is 9.1%, and it increases to 15.2% in men age 50-59, to 29.4% in men age 60-69, and 54.9% in men >70 years old.17
It is now accepted that the pathogenesis of this disease is multifactorial; it is estimated that about 80% of patients with ED are affected by other comorbidities and that this condition is not related only to psychological and hormonal factors. This has been proven by the increase in prevalence of ED in subjects presenting comorbidities such as physical inactivity, obesity, hypertension, metabolic syndrome, atherosclerosis and AVCD.18
The important role of pathological disorders of the vascular system is now recognised in the aetiology of ED. Penile erection is a haemodynamic process where arterial inflow and restricted venile outflow are involved. Therefore, an impairment of these functions can be a sign of underlying poor vascular function. ED has also been termed as 'penile angina' or vasculogenic impotence and can be predictive for future ACVD events.
Current evidence for a link between periodontitis and erectile dysfunction
Periodontitis has already been identified as a possible risk indicator for many systemic diseases and conditions. An investigation in 2016, based on bioinformatics screening of clinical trial databases, reported that periodontitis had been investigated in relation to 57 different and unique medical conditions, including erectile dysfunction.19 Nevertheless, it has to be acknowledged that periodontitis has not yet proven to be associated to all these conditions, but among them ED has drawn particular attention in the last ten years. Three recent systematic reviews and meta-analyses have summarised the available cross-sectional studies linking periodontal diseases with ED.20,21,22,23,24 The first review20 identified nine other studies which have been performed in various parts of the world (Table 1).23,24,25,26,27,28,29,30,31 The mean age of the male participants in the different studies varied from 35 to 51years, and all nine studies found an association between ED and periodontitis.
The second review22 identified four out of these nine eligible studies to be included in a meta-analysis. These four studies24,27,29,31 included many ED patients and controls (together 38,111 patients and 174,807 controls). The odds ratio (OR) among ED patients to have concomitant periodontitis was three times higher than those without ED (2.97; 95% confidence interval 1.87-5.05) and the association also remained significant for different age categories.
Similar results were shown by a recent meta-analysis.21 The OR obtained by the meta-analysis (2.28; 95% confidence interval 1.50-3.48) suggests a strong association between both diseases. This association remained significant also after considering only studies which adjusted the results for diabetes mellitus (OR 2.10; 95% confidence interval 1.49-2.95). However, the wide confidence interval reported by both meta-analyses indicates the study heterogeneity being very large (almost 100%).
In addition to these results, a recent study in Spain investigated the periodontal condition of patients affected by ED (objectively diagnosed in an andrology clinic) in comparison to subjects from the same clinic without ED.32 All subjects were age matched for comparison and all underwent an extensive periodontal examination. The results showed that patients with ED exhibited a more severe periodontal condition in comparison with controls, in particular a greater number of pockets 4-6 mm (19 ± 20.9 vs 13.9 ± 17.9, p = 0.05 for patients with ED and controls, respectively) and a greater amount of attachment loss (35 ± 31 sites with attachment loss >3 mm vs 23 ± 24, p = 0.01 for patients with ED and controls, respectively).32 Furthermore, an OR of 2.17 (CI 1.06-4.43, p = 0.03) indicated that periodontitis patients were more likely to have ED, independent of other confounders (Table 1). In light of the above-mentioned evidence, we can conclude that the association between ED and periodontitis exists, but it is weakly proven and more well controlled studies are needed.
Several issues on the validity of the putative association between ED and periodontitis need to be mentioned. ED is measured by validated questionnaires, mainly with the International Index of Erectile Dysfunction (IIEF) questionnaire or the abridged version of this (IIEF-5) and rarely have objective measurements of ED been used in the studies.33,34 Furthermore, some of the available studies (Table 1) also used questionnaires for the self-diagnosis of periodontitis. Moreover, many shared co-variables for periodontitis and ED, such as smoking, diabetes, obesity and other lifestyle habits or comorbidities, which could all influence the relationship. These influences are currently not fully accounted for in the statistical analyses.
However, despite these weaknesses in the scientific evidence, the association between periodontitis and ED may truly exist. When considering the strong link between periodontitis and ACVD, and the fact that the majority of cases of ED have at their aetiology a dysfunction in the vascular system, it is highly conceivable that periodontitis is associated with ED. Also, considering that there is a consistent body of literature that demonstrates the beneficial effect of the treatment of periodontitis on biological parameters of ACVD,35,36 it would be interesting to know whether periodontal therapy could alleviate ED complaints or reduce scores on the ED questionnaires.
To date, there is only one periodontitis intervention study in ED patients,23 which was performed in Turkey. This randomised clinical trial (RCT) involved 120 male participants who suffered both from ED based on the 'International Index of Erectile Dysfunction' score (IIEF questionnaire) and periodontitis. At baseline, 60 men were randomly assigned to 'no periodontal treatment' (mean age 36.6 years) and the other half of the study population was assigned to the periodontitis treatment group (mean age 38.1 years). At the three-month postoperative assessment, males who underwent periodontal therapy were shown to have the expected significant improvement in their periodontal condition, but also a significant improvement in their IIEF scores compared to those who did not receive any treatment (Fig. 1a and b). The study results are encouraging and are the first to show that internists and urologists, in addition to checking for ACVD, can also advise their male patients with ED to visit a dental practitioner to assess periodontal status and, if periodontitis is present, to treat it. We cannot assume that periodontal therapy would be the solution for ED, but it could help to improve the vascular condition of the patients,35,36 and therefore be helpful as part of a complete treatment of vasculogenic impotence.
a) and b) Results from the randomised controlled trial of Eltas et al.23 *Significant decrease (p <0.05) in the prevalence of pockets ≥4 mm in patients receiving periodontal therapy (test) in comparison to patients who did not receive any periodontal therapy (controls) at the one-month and three-month assessment; *Significant increase (p <0.05) in the IIEF score in patients receiving periodontal therapy (test) in comparison to the patient who did not receive any periodontal therapy (control) at the three-month assessment
Conclusions
Periodontitis is known to be associated with several systemic conditions and among these the link to cardiovascular disease has been extensively investigated and confirmed by solid and consistent evidence. The condition of the vascular system has been demonstrated to be worse in patients with periodontitis than those without, as measured by various parameters. Based on this evidence, it is conceivable to reason that periodontitis may also be associated with ED and, more specifically vasculogenic impotence, a condition resulting from atherosclerotic changes of arteries and other blood vessels. Ten cross-sectional studies and two meta-analyses point clearly towards this link. Moreover, one short-term treatment study suggests that treatment of periodontitis can decrease ED complaints as assessed by questionnaires alone. These preliminary positive results provide medical staff with information to motivate the male patient to visit a dental professional. If periodontitis is indeed indicated, patients can then receive appropriate periodontal treatment which may, in turn, help to manage their vasculogenic form of impotence.
References
Chapple I L, Genco R, working group 2 of joint EFP/AAP workshop. Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2013; 40 (Spec Iss): S106-S112.
Gulati M, Anand V, Jain N et al. Essentials of periodontal medicine in preventive medicine. Int J Prev Med 2013; 4: 988-994.
Linden G J, Herzberg M C, Working group 4 of joint EFP/AAP workshop. Periodontitis and systemic diseases: a record of discussions of working group 4 of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2013; 40 (Spec Iss): S20-S23.
Sanz M, Kornman K, Working group 3 of joint EFP/AAP workshop. Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2013; 40 (Spec Iss): S164-S169.
Tonetti M S, Van Dyke T E, Working group 1 of the joint EFPAAP workshop. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2013; 40 (Spec Iss): S24-S29.
Friedewald V E, Kornman K S, Beck J D et al. The American Journal of Cardiology and Journal of Periodontology Editors' Consensus: periodontitis and atherosclerotic cardiovascular disease. Am J Cardiol 2009; 104: 59-68.
Humphrey L L, Fu R, Buckley D I, Freeman M, Helfand M. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med 2008; 23: 2079-2086.
Dietrich T, Jimenez M, Krall Kaye E A, Vokonas P S, Garcia R I. Age-dependent associations between chronic periodontitis/edentulism and risk of coronary heart disease. Circulation 2008; 117: 1668-1674.
Schenkein H A, Loos B G. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J Clin Periodontol 2013; 40 (Spec Iss): S51-S69.
Orlandi M, Suvan J, Petrie A et al. Association between periodontal disease and its treatment, flow-mediated dilatation and carotid intima-media thickness: a systematic review and meta-analysis. Atherosclerosis 2014; 236: 39-46.
Piconi S, Trabattoni D, Luraghi C et al. Treatment of periodontal disease results in improvements in endothelial dysfunction and reduction of the carotid intima-media thickness. FASEB J 2009; 23: 1196-1204.
Houcken W, Teeuw W J, Bizzarro S et al. Arterial stiffness in periodontitis patients and controls. A case-control and pilot intervention study. J Hum Hypertens 2016; 30: 24-29.
Vidal F, Cordovil I, Figueredo C M, Fischer R G. Non-surgical periodontal treatment reduces cardiovascular risk in refractory hypertensive patients: a pilot study. J Clin Periodontol 2013; 40: 681-687.
Martin-Cabezas R, Seelam N, Petit C et al. Association between periodontitis and arterial hypertension: A systematic review and meta-analysis. Am Heart J 2016; 180: 98-112.
Bizzarro S, van der Velden U, Teeuw W J, Gerdes V E A, Loos B G. Effect of periodontal therapy with systemic antimicrobials on parameters of metabolic syndrome: A randomized clinical trial. J Clin Periodontol 2017; 44: 833-841.
Lue T F. Erectile dysfunction. N Engl J Med 2000; 342: 1802-1813.
Laumann E O, West S, Glasser D, Carson C, Rosen R, Kang J H. Prevalence and correlates of erectile dysfunction by race and ethnicity among men aged 40 or older in the United States: from the male attitudes regarding sexual health survey. J Sex Med 2007; 4: 57-65.
Leoni L A, Fukushima A R, Rocha L Y, Maifrino L B, Rodrigues B. Physical activity on endothelial and erectile dysfunction: a literature review. Aging Male 2014; 17: 125-130.
Monsarrat P, Blaizot A, Kemoun P et al. Clinical research activity in periodontal medicine: a systematic mapping of trial registers. J Clin Periodontol 2016; 43: 390-400.
Kellesarian S V, Kellesarian T V, Ros Malignaggi V et al. Association Between Periodontal Disease and Erectile Dysfunction: A Systematic Review. Am J Mens Health 2018; 12: 338-346.
Liu L H, Li E M, Zhong S L et al. Chronic periodontitis and the risk of erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res 2017; 29: 43-48.
Wang Q, Kang J, Cai X, Wu Y, Zhao L. The association between chronic periodontitis and vasculogenic erectile dysfunction: a systematic review and meta-analysis. J Clin Periodontol 2016; 43: 206-215.
Eltas A, Oguz F, Uslu M O, Akdemir E. The effect of periodontal treatment in improving erectile dysfunction: a randomized controlled trial. J Clin Periodontol 2013; 40: 148-154.
Keller J J, Chung S D, Lin H C. A nationwide population-based study on the association between chronic periodontitis and erectile dysfunction. J Clin Periodontol 2012; 39: 507-512.
Lee J H, Lee J S, Park J Y et al. Association of Lifestyle-Related Comorbidities With Periodontitis: A Nationwide Cohort Study in Korea. Medicine (Baltimore) 2015; 94: e1567.
Matsumoto S, Matsuda M, Takekawa M et al. Association of ED with chronic periodontal disease. Int J Impot Res 2014; 26: 13-15.
Oguz F, Eltas A, Beytur A, Akdemir E, Uslu M Ö, Güne- A. Is there a relationship between chronic periodontitis and erectile dysfunction? J Sex Med 2013; 10: 838-843.
Sharma A, Pradeep A R, Raju P A. Association between chronic periodontitis and vasculogenic erectile dysfunction. J Periodontol 2011; 82: 1665-1669.
Tsao C W, Liu C Y, Cha T L, Wu S T, Chen S C, Hsu C Y. Exploration of the association between chronic periodontal disease and erectile dysfunction from a population-based view point. Andrologia 2015; 47: 513-518.
Uppal R S, Bhandari R, Singh K. Association between erectile dysfunction and chronic periodontitis: a clinical study. Indian J Dent Res 2014; 25: 430-433.
Zadik Y, Bechor R, Galor S, Justo D, Heruti R J. Erectile dysfunction might be associated with chronic periodontal disease: two ends of the cardiovascular spectrum. J Sex Med 2009; 6: 1111-1116.
Martin A, Bravo M, Arrabal M, Magán-Fernández A, Mesa F. Chronic periodontitis is associated with erectile dysfunction. A case-control study in European population. J Clin Periodontol 2018; 45: 791-798.
Rosen R C, Riley A, Wagner G, Osterloh I H, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997; 49: 822-830.
Rosen R C, Cappelleri J C, Smith M D, Lipsky J, Peña B M. Development and evaluation of an abridged, 5item version of the international index of erectile function (IIEF-5) as a diagnostic tool of erectile dysfunction. Int J Impot Res 1999; 11: 319-326.
Han Y W, Houcken W, Loos B G, Schenkein H A, Tezal M. Periodontal disease, atherosclerosis, adverse pregnancy outcomes, and headandneck cancer. Adv Dent Res 2014; 26: 47-55.
Teeuw W J, Slot D E, Susanto H et al. Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol 2014; 41: 70-79.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bizzarro, S., Loos, B. The link between periodontitis and erectile dysfunction: a review. Br Dent J 227, 599–603 (2019). https://doi.org/10.1038/s41415-019-0724-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0724-6