Abstract
The consequences of no more linings under composite restorations are many and varied. This paper considers a number of these consequences and the impact they may have on the future use of composites in clinical practice.
Similar content being viewed by others
Key points
-
Provides the evidence base for not applying linings under posterior composite restorations, unless therapeutically indicated.
-
Offers dental practitioners evidence-based recommendations regarding the consequences of no linings under posterior composite restorations.
-
Informs those responsible for dental school curricula about contemporary approaches to the management of caries and placement of posterior composite restorations; if necessary, this may lead to a review of dental curricula and the adoption of contemporary practice.
-
Provides clinical teachers with an evidence base for teaching new approaches to the management of caries and placement of posterior composite restorations.
Introduction
The use of direct resin-based composites continues to increase.1,2 This increase has been attributed to various factors, including: increasing patient demand for tooth-coloured restorations; developments in composite and adhesive technologies; improvements in the handling characteristics of composites and related adhesive systems; the introduction of faster and easier composite placement techniques and facilitating devices, and reduced concerns over the longevity of posterior composites,3,4 together with encouraging data on the efficacy of composite repairs; the phase down in the use of dental amalgam; and the progressive shift toward preventatively-orientated, minimum intervention approaches to the restoration of posterior teeth.5
Acceptance that existing evidence does not support the placement of a lining (liner, base or combinations thereof) under posterior composites, irrespective of the depth of the preparation, except in situations where the lining is intended to have therapeutic pulpal effects in deep cavities,5 makes composites quicker and easier. This evidence includes a Cochrane review on cavity liners, data on the performance, resistance to fracture, longevity of restorations with and without linings, and negative findings on the value of linings in preserving pulp vitality,6,7 together with the realisation that the 'seal is the deal' in maintaining the biological integrity of composites in clinical service.
Consideration of the consequences of 'no more linings' under composites is the purpose of this paper. These consequences include:
-
The need to review relevant teaching
-
The challenge to change custom and practice in conservative (operative) dentistry
-
The need to adopt new approaches to the management of caries
-
Increased reliance on adhesive bonding
-
Reductions in the time taken to place composite restorations
-
Enhanced biomechanics of restored tooth units
-
Simplified repair protocols
-
Increased restoration longevity.
Teaching
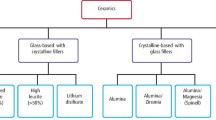
Composites have been taught in dental schools in the UK and many countries around the world for varying periods of time as the material of choice for restoring anterior teeth as well as occlusal and occluso-proximal defects in posterior teeth.3,8,9,10,11 However, important variations in teaching have been reported, notably variations in the selection of liners, base materials and lining techniques.3,12,13 Many dental schools have recently been found to recommend the use of a glass-ionomer (GI) material to line specifically deep cavities to replace dentine and on the understanding that, in bonding to dentine, GI's hermetically seal off the floor and, when present, axial walls of the cavity.3,9 In addition, it remains a widely held view that the antibacterial effects of fluoride release from GI bases are clinically significant throughout the clinical service of the restoration. Such thinking is considered misguided.14,15
Adoption of no more linings under composites will make a major contribution to the harmonisation of teaching on composites, assuming this watershed development does not lead to new variations in the teaching of, for example, the management of caries and adhesive bonding. Bodies such as the European Federation of Conservative Dentistry (EFCD) and the Academy of Operative Dentistry (AOD) could, it is suggested, produce protocols for the placement of lining-free restorations. Ideally, the EFCD, AOD and other bodies with interests in the teaching of state-of-the-art conservative/operative dentistry, should work together to produce the proposed protocols with students and patients being joint beneficiaries of such innovative, international collaboration.
Custom and practice
Changing and harmonising teaching nationally, let alone internationally, can be difficult but the challenge of changing custom and practice in the everyday provision of oral health care can be much greater. With the procedure of placing a lining before the placement of a restoration, except in cavities of minimum depth, so deeply embedded in the thinking of most existing practitioners, it will be no mean feat to achieve widespread practice of no more linings under composites. Perhaps the greatest concerns to overcome are potential damage to the pulp and an increased incidence of postoperative sensitivity, both of which may have negative effects on patient satisfaction and, in turn, confidence in a practitioner and practice. Hopefully, some comfort may be found in the study by von Fraunhofer et al.16 which concluded that there is an increase in microleakage, postoperative sensitivity and potentially secondary caries when a lining is present under a posterior composite.
As and when 'no more linings under composites' statements feature in the aims and objectives of continuing professional development programmes, a shift to the new way of thinking could take many years, if not a generation to achieve. This, it is suggested, is too slow given the implications to patients and oral healthcare systems. If, however, the dental industry can find ways to help change custom and practice in the use of linings through, for example, changing directions and schematics for the use of composite systems, the rate of change could be greatly increased.
Management of caries
Traditionally, dental schools have taught that all caries, except possibly for some residual softened, unstained dentine close to the pulp, should be removed before proceeding to restore a tooth. Thompson et al.17 stated that once isolated from their source of nutrition by a restoration of sufficient integrity, bacteria in caries either die or remain dormant and therefore pose no risk to the tooth. Thus, 'the seal is the deal'.
To date, three literature reviews have concluded that there is substantial evidence that removing all caries in an asymptomatic, vital tooth is not required, especially if one is attempting to avoid pulpal exposure.17,18,19 Indeed, there is increasing evidence that continuing to excavate until the base of the preparation is formed of hard, albeit somewhat discoloured dentine, may do more harm than good. So, 'out with the old and in with the new' contemporary recommendations for the management of caries will be in the best interests of patients, especially given the findings of Blum et al.,20 that the prevalence of postoperative sensitivity after the placement of posterior composites may be up to 20% greater when a lining has been placed. The key to understanding this conundrum may be the creation of microgaps between the dentine and lining in the presence of moisture contamination.21
A further benefit of the adoption of a modern approach to the management of caries will be a reduced need to counter iatrogenic damage caused by the unnecessary, operative exposure of vital dentine, as may occur when, for example, a large round bur is used to render the base of a preparation caries free; a process which may readily result in postoperative discomfort, particularly when a large round bur is applied at speed with little, if any water cooling.
Adhesive bonding
If more caries is to be left in the base of preparations, practitioners may reasonably seek new reassurances on the nature, adequacy and durability of the bond formed between dental adhesive and residual caries-affected dentine in unlined cavities. If this bond suffers certain limitations, does it mean that the integrity of the bond along the cavosurface margin is all the more critical? And what may be the consequences of this bond failing?
Practitioners asking such questions may take comfort in the work of von Fraunhofer et al., who concluded that there is an increase in microleakage, postoperative sensitivity and potentially secondary caries when a lining is present under a posterior composite.16 Also, the work of Yoshiyama et al. showed that the sealing effect of bonding agents on different dentine substrates provides adequate protection and renders the dentine insensitive, reducing or eliminating postoperative sensitivity and possible adverse effects of resins on the pulp.22
Placement times
With no need to place a lining, which may be compound sub-base and base, let alone the use of deep cure composites and simplified caries management, it is anticipated that placement times for state-of-the-art posterior composites will be found to be similar, not significantly different to those for traditional direct restorations of dental amalgam. In considerations of placement times, it is often forgotten that the newly placed composite has been contoured and finished or 'polished'. This is in contrast to a newly placed restoration of dental amalgam which, at most, may have been burnished following contouring.
It may, however, be argued that, in the absence of a lining, there may be all the more reason to use a flowable composite to 'wet' and thereby enhance adaption of the restoration to the prepared tooth surface and, in the process, extend placement times. The polymerisation shrinkage and modulus of elasticity of flowable composites are relatively high, with the risk of bond disruption on polymerisation. Such disruption may result in poor sealing of the dentine as well as microgaps. Such gaps typically become colonised with bacteria, followed by a build-up of bacterial by-products, causing irritation to the pulp, resulting in sensitivity, and possibly caries type changes in the dentine substrate.23 As such, the case for the use of a flowable composite to form an initial layer in the base of a cavity to be restored with a composite remains debatable.
With further developments in placement aids, including matrix systems, it is possible that composites may come to be viewed as no more time consuming and troublesome to place than restorations of other direct materials. Graduates who have had more experience of placing posterior composites than restorations of dental amalgam are predicted to be among the first practitioners to form such views.
Biomechanics
Opdam et al.,24 in investigating the longevity and reasons for failure of complex posterior composites placed with or without a lining, found that posterior composites placed on top of a GI lining suffered more fractures than posterior composites placed using a total-etch technique. In other words, the placement of a lining may adversely affect the biomechanical properties of a composite-restored tooth unit, specifically its resistance to fracture. Also, a long-term clinical study by van de Sande et al.25 evaluated the effect of linings on the survival of posterior composites. It was concluded that the presence of a lining neither extended nor reduced the survival of composite restorations. Additionally, it was determined that there is no evidence to support the replacement of lost dentine with a 'dentine replacement' material.25 Indeed, support was given to the findings of Opdam et al.24 that such an approach may make the restoration more liable to suffer failure by fracture.25 Such thinking is reinforced by the findings of the recent Cochrane review which concluded that 'using a liner is an unnecessary step in routine composite-based restorations in adult posterior teeth'.6
Repair
Repair rather than replacement of failing restorations is now widely taught.26,27,28,29,30,31,32,33,34 From the growing body of evidence on the benefits and efficacy of repairs, it is suggested that the repair of posterior composites which have been placed without a lining, rather than lined, will be found to be quicker and simpler with the possibility of enhanced performance in clinical service. The absence of a lining removes many of the uncertainties when assessing the suitability of a failing restoration for repair rather than replacement, making decisions in such situations easier and possibly more effective. Specifically, the absence of a lining makes the radiographic assessment of failing restorations easier, given the absence of restoration/lining interfaces and no possibility of voids subjacent to restorations, as may occur with the 'washout' of calcium hydroxide linings which remain popular in clinical practice.
Longevity
Taken together, the findings of Opdam et al.24 that posterior composites without linings may remain in clinical service longer than composites with linings, and the prospect of repairs to unlined composites being more efficacious than repairs to lined composites, it may be anticipated that the longevity of unlined composites which are well maintained in clinical service, will exceed the longevity of lined composites. Any measure which effects an increase in restoration longevity has an important impact on 'teeth for life' through a slowing down of the 'restorative cycle' and, as such, should be adopted. Available evidence favours the adoption of 'no more lining' under composites for this very reason.
Discussion
Recent in-depth reviews report very little evidence to support the use of linings under composites.5,6 Indeed, these reviews identified linings as having a number of detrimental effects on composite restorations. This assumes the adoption of a modern approach to the management of caries, the appropriate use of state of the art adhesive technologies and a knowledge of the processes involved in a 'no linings' approach to the restoration of teeth with composite.
Traditionally, it has been the norm to place a lining on the floor and, when present, axial walls of the cavity,12,13 except in preparations of minimum depth, before placing a restoration. The placement of a lining has been considered necessary for many different reasons, including protection of the pulp against thermal and electric stimuli, the protection of pulpal cells against chemical irritants, promotion of the development of reactionary and reparative dentine, the possible remineralisation of subjacent dentine, and limiting the effects of restoration leakage on the pulp.35,36 It therefore came as no surprise in a recent UK-based survey that most practitioners (83%) always placed a lining before restoring a posterior tooth with composite, except in shallow (minimum depth) cavities.20 Forty four percent of the practitioners reported using a GI for this purpose, followed by, in decreasing order, a flowable resin composite (39%), a hard-setting calcium hydroxide liner (38%), and resin-modified glass-ionomer cement (32%).20 A small minority (11%) of respondents reported, as advocated in this paper, applying no lining before the placement of posterior composites, irrespective of the depth of the cavity.20 So, what is being proposed could involve >85% of practitioners in the UK reviewing their current approach to the restoration of teeth with composite. In the meantime, it is to be hoped that those dental schools which continue to teach the placement of a GI lining in moderately deep, (cavities that extended between one third and two thirds into the dentin) and, more commonly, deep (cavities that extended into the inner one-third of the dentine) occlusal and occluso-proximal cavities to be restored with composite, will review this aspect of their teaching to bring it into line with best available evidence.
Conclusions
As concluded by Lynch et al.,4 current thinking, based on the best available evidence, may be summarised as follows: 1) the use of liners and bases is traditionally associated with amalgam, mainly because these (liner and base) materials are necessary to provide thermal insulation between amalgam and underlying vital dentine. Resin composites are insulators and do not require a lining or base for insulation purposes; 2) predictable adhesion of resin-based composite restorations to remaining tooth tissues can be achieved using modern dentine bonding systems. A lining limits the available surface area for bonding and reduces the thickness of resin composite >1.5 mm, limiting the physical and biomechanical properties of the completed restoration. Furthermore, the application of a dentine bonding agent will seal the restoration and the underlying dentine protecting the pulp from stimuli and bacterial ingress. Two-step self-etching and three-step etch-and-rinse adhesives exhibit very strong adhesion to tooth structure when placed correctly.37 It would appear, therefore, that there is no longer an indication to place a lining under a posterior resin composite. As concluded by Blum and Wilson,5 the exception is situations where a base or lining is indicated for therapeutic reasons.
The consequences of shifting to no more linings under composites offer advantages and benefits to both patients and practitioners. As a consequence, this development in the use of composites for the restoration of posterior teeth should be beneficial to oral healthcare systems. It is suggested, therefore, that much is to be gained by early action to plan a shift to no more linings under composites, as the next step in the 'coming of age' of posterior composites. Such planning may include getting up to speed on the modern management of caries and the use of state-of-the-art adhesive systems. If in any doubt, plan to attend continuing professional development programmes providing instruction in state-of-the-art approaches to the use of composites to restore posterior teeth.
References
Demarco F F, Correa M B, Cenci M S, Moraes R R, Opdam N J. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 2012; 28: 87-101.
Rasines Alcaraz M G, Veitz-Keenan A, Sahrmann P, Schmidlin P R, Davis D, Iheozor-Ejiofor Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst Rev 2014; 31: CD005620.
Lynch CD, Frazier K B, McConnell R J, Blum I R, Wilson NH. State-of-the-art techniques in operative dentistry: contemporary teaching of posterior composites in UK and Irish dental schools. Br Dent J 2010; 209: 129-136.
Lynch CD, McConnell R J, Wilson NH. Posterior composites: the future for restoring posterior teeth? Prim Dent J 2014; 3: 49-53.
Blum I R, Wilson N H F. An end to linings under posterior composites? J Am Dent Assoc 2018; 149: 209-213.
Schenkel A B, Peltz I, Veitz-Keenan A. Dental cavity liners for Class I, Class II resin-based composite restorations. Cochrane Database Syst Rev 2016; 10: CD010526.
Strober B, Veitz-Keenan A, Barna J A et al. Effectiveness of a resin-modified glass ionomer liner in reducing hypersensitivity in posterior restorations: a study from the practitioners engaged in applied research and learning network. J Am Dent Assoc 2013; 144: 886-897.
Gordan V V, Mjör I A, Veiga Filho L C, Ritter A V. Teaching of posterior resin-based composite restorations in Brazilian dental schools. Quintessence Int 2000; 31: 735-740.
Lynch CD, Frazier K B, McConnell R J, Blum I R, Wilson NH. Minimally invasive management of dental caries: contemporary teaching of posterior resin-based composite placement in U.S. and Canadian dental schools. J Am Dent Assoc 2011; 142: 612-620.
Hayashi M, Yamada T, Lynch C D, Wilson N H F. Teaching of posterior composites in dental schools in Japan - 30 years and beyond. J Dent 2018; 76: 19-23.
Wilson NH, Lynch CD. The teaching of posterior resin composites: planning for the future based on 25 years of research. J Dent 2014; 42: 503-516.
Weiner R S, Weiner L K, Kugel G. Teaching the use of liners and bases: a survey of North American dental schools. J Am Dent Assoc 1996; 127: 1640-1645.
Weiner R. Teaching the use of liners, bases, and cements: a 10-year follow-up survey of North American dental schools. Dent Today 2006; 25: 74, 76, 78-79.
Randall R C, Wilson N H F. Glass-ionomer restoratives: a systematic review of a secondary caries treatment effect. J Dent Res 1999; 78: 628-637.
Wiegand A, Buchalla W, Attin T. Review on fluoride-releasing restorative materials-fluoride release and uptake characteristics, antibacterial activity and influence on caries formation. Dent Mater 2007; 23: 343-362.
von Fraunhofer J A, Marshall K R, Holman B G. The effect of base/liner use on restoration leakage. Gen Dent 2006; 54: 106-109.
Thompson V, Craig R G, Curro F A, Green W S, Ship J A. Treatment of deep carious lesions by complete excavation or partial removal: a critical review. J Am Dent Assoc 2008; 139: 705-712.
Ricketts D, Lamont T, Innes N P, Kidd E, Clarkson J E. Operative caries management in adults and children. Cochrane Database Syst Rev 2013; 28: CD003808.
Hoefler V, Nagaoka H, Miller C S. Long-term survival and vitality outcomes of permanent teeth following deep caries treatment with step-wise and partialcariesremoval: A Systematic Review. J Dent 2016; 54: 25-32.
Blum IR, Younis N, Wilson N H. Use of lining materials under posterior resin composite restorations in the UK. J Dent 2017; 57: 66-72.
Peliz M I, Duarte S Jr, Dinnelli W. Scanning electron microscope analysis of internal adaptation of materials used for pulp protection under composite resin restorations. J Esthet Restor Dent 2005; 17: 118-128.
Yoshiyama M, Masada J, Uchida A, Ishida H. Scanning electronic microscopic characterization of sensitive vs. insensitive human radicular dentin. J Dent Res 1989; 68: 1498-1502.
Ruiz J L, Mitra S. Using cavity liners with direct posterior composite restorations. Compend Contin Educ Dent 2006; 27: 347-351.
Opdam N J, Bronkhorst E M, Roeters J M, Loomans B A. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent 2007; 9: 469-475.
van de Sande F H, Rodolpho P A, Basso G R et al. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent Mater 2015; 31: 669-675.
Blum I R, Schriever A, Heidemann D, Mjör I A, Wilson N H. The repair of direct composite restorations: an international survey of the teaching of operative techniques and materials. Eur J Dent Educ 2003; 7: 41-48.
Gordan V V, Mjör I A, Blum I R, Wilson N. Teaching students the repair of resin-based composite restorations: a survey of North American dental schools. J Am Dent Assoc 2003; 134: 317-323.
Blum I R, Lynch C D, Wilson N H. Teaching of direct composite restoration repair in undergraduate dental schools in the United Kingdom and Ireland. Eur J Dent Educ 2012; 16: e53-e58.
Blum I R, Lynch C D, Wilson N H. Teaching of the repair of defective composite restorations in Scandinavian dental schools. J Oral Rehabil 2012; 39: 210-216.
Lynch C D, Blum I R, Frazier K B, Haisch L D, Wilson N H. Repair or replacement of defective direct resin-based composite restorations: contemporary teaching in U.S. and Canadian dental schools. J Am Dent Assoc 2012; 143: 157-163.
Lynch C D, Hayashi M, Seow L L, Blum I R, Wilson N H. The management of defective resin composite restorations: current trends in dental school teaching in Japan. Oper Dent 2013; 38: 497-504.
Brunton P A, Ghazali A, Tarif Z H et al. Repair vs replacement of direct composite restorations: a survey of teaching and operative techniques in Oceania. J Dent 2017; 59: 62-67.
Kanzow P, Wiegand A, Wilson N H F, Lynch C D, Blum I R. Contemporary teaching of restoration repair at dental schools in Germany - Close to universality and consistency. J Dent 2018; 75: 121-124.
Kanzow P, Wiegand A, Göstemeyer G, Schwendicke F. Understanding the management and teaching of dental restoration repair: Systematic review and meta-analysis of surveys. J Dent 2018; 69: 1-21.
Weiner R. Liners and bases in general dentistry. Aust Dent J 2011; 56 (Spec Iss): 11-22.
Hilton T J. Cavity sealers, liners, and bases: current philosophies and indications for use. Oper Dent 1996; 21: 134-146.
Foxton R. Procedures in Operative Dentistry. In Wilson N, Dunne S (eds) Manual of Clinical Procedures in Dentistry. 1st ed. pp 229-251. Oxford: John Wiley & Sons, 2018.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blum, I., Wilson, N. Consequences of no more linings under composite restorations. Br Dent J 226, 749–752 (2019). https://doi.org/10.1038/s41415-019-0270-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0270-2
This article is cited by
-
Evidence-based fact checking for selective procedures in restorative dentistry
Clinical Oral Investigations (2023)