Abstract
Introduction There is set to be a change in the way that oral surgery will be delivered with the introduction of managed clinical networks. The changes may require general dental practitioners (GDPs) to carry out more minor oral surgery in primary care.
Aim To determine the effectiveness of courses on GDPs carrying minor oral surgery in primary care.
Method Forty general dental practitioners attending a hands-on oral surgery course were surveyed regarding their understanding, knowledge and confidence in oral surgery skills. The same survey was circulated at the start and end of the course.
Results All delegates reported an improvement post-course in their skills and knowledge. Overall, 40% of delegates felt relatively confident or very confident in tooth sectioning and bone removal, compared to 91% having little confidence before the course. Furthermore, 87% and 68% of the delegates felt relatively confident or very confident in suturing and raising a mucoperiosteal flap, respectively, by the end of the course.
Conclusion Minor oral surgery courses can lead to an increase in skills, knowledge and confidence among GDPs. These courses are likely to be better supplemented in conjunction with refresher courses and mentoring. Barriers, however, remain to increasing minor oral surgery provision in primary care, including equipment availability and patient choice.
Similar content being viewed by others
Key points
-
Suggests oral surgery courses for the general dental practitioner are likely to lead to an improvement in confidence amongst practitioners.
-
Suggests oral surgery courses are useful for promoting knowledge and enhancing basic surgical skills.
-
Highlights that maintenance of confidence, knowledge and skills acquired through oral surgery courses will likely require refresher courses and a strong oral surgery support network.
Introduction
NHS England released the Five year forward view in 2015.1 The impact of this document is particularly relevant to oral surgery, as it aims to increase the provision of primary and 'out of hospital' oral surgery services and introduce managed clinical networks (MCNs).2 MCNs have already been successfully utilised in some parts of the country, such as in Kent and Manchester. Oral surgery procedures are being categorised into three tiers based on the surgical complexity and medical modifying factors, as described in the Guide for commissioning for oral surgery and oral medicine, which have been summarised in Table 1.2
Through MCNs, referred oral surgery cases will be categorised into the appropriate level of complexity, and triaged accordingly into primary or secondary care. The impact of this is likely to result in general dental practitioners (GDPs) being expected to carry out more minor oral surgery (MOS) procedures. It is, therefore, important that they have the necessary knowledge, skills and confidence to carry out MOS procedures as well as having a support network.
Several studies have been carried out reporting on the confidence of final year dental undergraduates and newly-qualified vocational dental practitioners (VDPs) on a variety of dental procedures, but there is little in the literature regarding the impact and value of postgraduate minor oral surgery courses for GDPs. Shah et al.3 found that a cohort of 150 final year dental students felt that they had confidence levels of 5.7 out of 10, with ten being the most confident, in raising a mucoperiosteal flap and sectioning a tooth, and were highly confident in suturing with an average score of 8.0 out of 10. In contrast, Gilmour et al.4 found that of 39 dental procedures assessed, final year undergraduate dental students were least confident in surgical extractions.
Coulthard et al.5 found that 81% of GDPs carried out less than ten oral surgery procedures per month and 96% of GDPs referred up to ten oral surgery cases to a specialist each month. Patel et al.6 reported that newly-qualified dental foundation trainees were least confident in carrying out surgical extractions, compared to procedures of restorative and paediatric dentistry. Furthermore, Coulthard et al.5 found that the most common reasons for referral to specialist oral surgery services were the anticipated difficulty of surgery, a preference not to undertake surgical procedures in practice and complicated medical histories. For comparison, when looking at oral surgery referral patterns in the USA, Cottrell et al.7 found that GDPs referred 17% of cases requiring simple dentoalveolar surgery and 98% of cases requiring complex dentoalveolar surgery. In cases of complex patient medical histories, the number of cases treated in practice dropped drastically with 39% of simple dentoalveolar cases being referred. However, Absi et al.8 found that 70% of the 'medically compromised' patients had no special requirements and could be safely managed in general dental practice. In the last decade, there have been large advancements in the medical management of patients, for example, the development of monoclonal antibodies and chemotherapeutic drugs for oncology and an increase in the use of intravenous bisphosphonate therapy. Such medical management strategies may be complex and it may be desirable to treat such cases in a secondary care setting. However, there has been no literature to reflect these changes.
As a result of the proposed changes to the commissioning of oral surgery, it is imperative that minor oral surgery procedures are not disregarded in primary care. The aim of this study was to assess the effectiveness of courses on GDPs carrying MOS in primary care.
Method
In this study 40 GDPs were enrolled in the same seven-module continued professional development (CPD) MOS course, run by the Eastman Dental Hospital, which ran over the duration of seven months. The course consisted of didactic lectures on oral surgery and human disease, case-based discussions (two modules), practical pigs' heads skills (one module), and treating patients (four modules).
Two methods were used to assess the outcomes of the course. The first was a survey circulated both at the start and end of the course. A series of 15 questions were included, which assessed the knowledge gained from the course and also a rating of their confidence to carry out certain MOS procedures. The second method was an audit that all delegates were asked to complete. Delegates recorded MOS referrals that were made both throughout the duration of the seven-month course and for six months following its completion. Changes in referral patterns could therefore be assessed.
Results
Of the 40 GDPs that attended the course, 38 pre- and post-course questionnaires were collected, giving a response rate of 95%. Pre- and post-course audits were only completed by 21 of the 40 delegates, giving a response rate of 53%.
Demographic profile
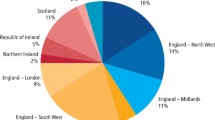
Of those that responded, 18% worked in full NHS practice, 53% in mixed NHS practice, 21% in a fully private practice, 2.6% in the armed forces, 2.6% in a community setting and 2.6% worked in a hospital setting. The majority of GDPs, 63%, saw between 11 and 20 patients a day.
Extractions
Figure 1 shows the number of extractions carried out by the cohort of GDPs attending the MOS course before and after they attended the course. Prior to the course, the mode number of extractions undertaken per week was 0-2. This rose to 3-5 extractions per week after completion of the course.
Scenarios
Table 2 illustrates the different clinical cases that were presented in the questionnaire. Table 3 summarises the pre- and post-course confidence level with managing each scenario. In all cases, except case two, less than 25% of the cohort was relatively confident or very confident in managing the scenarios illustrated in Table 1 before undertaking the course. In scenario two, 34.2% were relatively confident in managing the scenario before attending the course. However, after the course more than 60% of the cohort was relatively confident or very confident in managing all five scenarios.
Oral bisphosphonate patients
Table 4 summarises the results of treating patients on oral bisphosphonate therapy. There was a dramatic rise in confidence after GDPs had attended the course, as 76.3% stated they would be confident to extract the tooth on a patient who has been taking oral bisphosphonate therapy for two years to treat osteoporosis; compared to only 18.4% of them being happy to extract the tooth in practice before attending the course.
Suturing
Figure 2 shows that, following the course, 50% were relatively confident and 39% were very confident in suturing compared to 94% having no confidence at all or being relatively confident before the course.
Raising a mucoperiosteal flap
Figure 3 shows the confidence levels for raising a mucoperiosteal flap. Prior to the course, 47% had no confidence at all and 42% were relatively unconfident in raising a flap. After the course confidence had risen sharply, with 68% being relatively confident or very confident in raising a mucoperisoteal flap.
Surgical bone removal and tooth sectioning
Figure 4 shows the confidence levels for surgical bone removal and tooth sectioning. Compared to suturing and raising a flap, confidence did not improve as much in this category. However, before the course, 47% and 44% were not confident and relatively unconfident respectively. Following the course, 21% were relatively unconfident, 31% were neither confident nor unconfident and 24% were relatively confident in surgical bone removal and tooth sectioning.
Discussion
The value and effectiveness of CPD has been widely researched in medical literature. Bullock et al.9 indicated that the best way for a CPD course to have an impact on practice was by offering updates on common clinical practice, involving patient interaction and including a hands on component. Furthermore, Grant revealed that the performance of doctors was enhanced in specific areas after attending CPD activities.10 A review by Forsetlund et al supports this, as it is concluded that educational meetings (CPD) using mixed interactive and didactic formats, with the addition of other interventions, for example hands-on practice, and focusing on outcomes can increase the effectiveness of CPD and change practice behaviours.11 The best way to evaluate improvement in performance is by auditing if there are any changes in a clinician's practice following course attendance over a prolonged period of time. Eaton et al.12 concluded that the most effective forms of CPD should enable the retention of knowledge and skill. This includes ongoing CPD activities, interactive teaching including case-based discussions and the use of multimedia. Ongoing CPD over a prolonged period of time has also proved desirable.10
In our GDP MOS course, participants attended seven modules over a period of seven months. It incorporated the use of didactic teaching, group learning, case-based discussions and in vitro and in vivo practical sessions. The course was designed to help GDPs gain clinical experience under supervision to supplement and consolidate theoretical learning. The course was designed over a longer duration to aim to improve GDP confidence in carrying out oral surgery over a sustained period of time.
Through the use of the pre- and post-course questionnaires, this study revealed that, following the completion of the MOS course, GDPs perceived an improvement in their confidence to carry out both oral surgery cases in primary care as well as in their skills of suturing, flap raising, bone removal and sectioning of teeth. Data were also collected to assess a change in referral patterns among the delegates. All delegates were asked to keep a record of all MOS referrals that they made for six months during the duration of the course, as well as six months following completion of the course. The average number of referrals made during the duration of the course was 15 extractions. This figure increased to 16 extractions in the six months following the course. The results revealed that although confidence had improved, there had been no significant changes in MOS referrals patterns being made by GDPs. There could be several reasons for this including lack of incentive to carry out dental extractions in primary care due to remuneration, especially if multiple extractions were required and a lack of long-term investment in MOS equipment, including instruments, surgical drills and sutures by dental practices, thus disenabling GDPs from carrying out MOS. Another important factor to consider included patient preference to be treated in secondary care for dental extractions. Furthermore, upon interviewing GDPs regarding clinical decision making in general dental practice, Davies and Macfarlane readily found that dental extractions were not perceived as being a practice builder by dentists.13 This could contribute another reason for the referral of dental extractions rather than carrying them out in primary care.
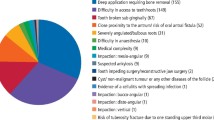
Coulthard et al.5 found that the most common reasons patients were referred to secondary care for MOS were the complexity of the procedure and the medical history of the patient. Similar findings were reported by Halai and Yates, who stated that the three most common reasons for MOS referral included surgical extractions, multiple extractions and perceived surgical complexity.14 Our study had similar findings, with results from the audit revealing surgical complexity to be the most common reason for referral (46%). Other common reasons included medical complexity (38%) and patient anxiety (8%). It should be noted that discussing referral patterns is very much speculative. Although GDP participants were asked to audit the number of patients they referred to MOS providers for dental extractions before and after the course, the response rate was low (53%) and hence results are not likely to be reflective of the full cohort.
The impact of complex medical histories can be highlighted in the results from the pre-course questionnaire. In terms of managing patients on anti-platelets and anti-coagulants, respectively, 26.3% and 36.8% of delegates reported having no confidence at all (cases four and five in Table 2). Furthermore, only 18.4% of delegates felt confident to extract a tooth on an osteoporotic patient who had been taking oral bisphosphonates for two years. The Scottish Dental Clinical Effectiveness Programme (SDCEP) guidelines categorise patients at low risk of developing medication-related osteonecrosis of the jaw (MRONJ) in those that are about to start bisphosphonate therapy for any condition or in the prevention or management of osteoporosis without additional risk factors, such as chemotherapy or immunosuppression.15 In the scenario presented, the patient was deemed at low risk of developing MRONJ and therefore could be treated in primary care.
The findings from the audit data and pre-course questionnaire are not reflective of the experience and training received by the GDPs at undergraduate level. Forceps exodontia and simple surgical exodontia are expected to be a basic clinical skill for dental graduates, with undergraduates undertaking exodontia competencies throughout their training. Cowpe et al.16 postulates that a dentist should be competent in carrying out uncomplicated extractions of erupted teeth and the surgery for the uncomplicated removal of fractured or retained roots, as well as the removal of uncomplicated partially erupted teeth. Brand et al.17 found that dental students across Europe varied considerably in their opinion of how well they were trained in exodontia. Students from Plymouth dental school felt best prepared out of all the schools involved in the study, with students from London and Leeds feeling nearly as well prepared; students from Cardiff did not feel as well prepared in comparison. On the whole, dental students felt relatively comfortable carrying out MOS at an undergraduate level, possibly because they carried it out on a more regular basis, they were supervised, and therefore possibly less fearful of complications. In comparison, qualified GDPs may feel less confident in carrying out MOS due to a number of external factors. This includes the lack of adequate equipment to carry out dental extractions, and this in turn can lead to deskilling as a GDP's dental career progresses. There may also be concerns about complications for which they are not experienced to deal with, and with no one being readily available immediately to troubleshoot, they are more likely to refer even routine dental extractions. In the future, questionnaires for participants attending CPD MOS courses at the Eastman Dental Hospital will be adapted so that more information can be gained regarding the availability of equipment to carry out MOS in their primary care settings.
The results of this study show an overall improvement in the confidence of GDPs to carry out oral surgery procedures in primary care. However, it is important to recognise that an improvement in confidence does not necessarily reflect changes in competency and behaviours. This has been well documented in healthcare, with Barnsley et al.18 concluding that there was no relationship between junior medical doctors' self-reported confidence and competence in the acquisition of procedural and cognitive clinical skills, with confidence being higher than observed competence in all of the skills that were assessed. This is corroborated by Davis et al.,19 who found that there was little, no or an inverse relationship between the relationship of a physician's self-reported confidence and external assessment. Some studies also found that those who were the least skilled were also the most confident.
Continual feedback is given out through the course in a longitudinal manner. However, it would be beneficial for this feedback to be more formalised in a written manner. Formative assessments, much like those that dental core trainees and speciality registrars carry out in the form of work-based assessments, by means of direct observation of procedural skills (DOPS), could be utilised. This would enable participants the opportunity to reflect upon their cases both in terms of a patient management perspective and their surgical skills. This will also allow for two-way feedback immediately after a MOS procedure was carried out by a participant, helping to detect strengths and weaknesses and thereby identify learning needs. These assessments would form the basis of an ongoing reflective log. Reflective clinical practice is at the forefront of education and training and is highlighted by the General Dental Council's changes in CPD requirements, which require a personal development plan as well as reflection on all CPD activities.20 There is much support for reflective practice in the literature as highlighted by Gibbs in 1988, who states that reflection on a task leads to learning as well as identifying strengths, areas for improvement, identifying educational needs and acquiring knowledge and clinical skills.21
Consideration could be given to introducing a competency-based assessment as part of the MOS course. In order to assess competence, all external factors would have to be standardised as reasonably possible. This includes standardisation of assessors carrying out DOPS as well as standardisation of the treatment that each participant undertakes. However, due to the nature of oral surgery, it is difficult to standardise each treatment as there will always be anatomical variances from one tooth to another. This is further complicated by the patient factors, such as in situations when highly anxious patients can make treatment more challenging.
One of the limitations of this study was the fact that the confidence levels of the GDP cohort was measured at the end of the course, where it would have been expected to be at its highest. The participants had completed a prolonged oral surgery course under supervision, so they may have felt that they were in a safe environment to carry out MOS, anticipating that if any complications occurred, these could have been managed by senior clinicians and specialists in oral surgery who ran the course. In the future, it would be useful to see if the GDPs maintained this level of confidence long-term, after the duration of the course. As previously mentioned, although attendance at CPD courses cannot measure improvement in performance and competence, maintaining skills that are newly acquired is vital. However, if GDPs are unable to adapt and implement the skills they have learnt, for example, due to the lack of appropriate equipment to carry out MOS, these skills may diminish over time. Refresher courses and clinical mentorship, similar to that used for dentists undergoing training for the provision of implants, may be useful for such participants along with a structured oral surgery support network which could hold the key in not only improving but leading to a sustained change in the provision of oral surgery in primary care.
Conclusion
MOS courses for GDPs are likely to improve knowledge and confidence in carrying out surgical procedures. However, used in isolation, such courses will have little impact on behaviour change. The use of refresher courses and clinical mentoring would be useful. It is important, however, to recognise that knowledge, skills and confidence make up only one possible reason that MOS is not carried out by GDPs in primary care. Other factors such as patient preference, remuneration and lack of sufficient equipment are likely to play a part in explaining referral patterns. These areas also have to be targeted to see a sustained change in the remit of a GDP and their scope of oral surgery in primary care.
References
NHS England. Five year forward view. 2014. Available at http://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed March 2019).
NHS England. Guide for commissioning for oral surgery and oral medicine. 2015. Available at https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/09/guid-comms-oral.pdf (accessed March 2019).
Shah S, Halai T, Patel J, Sproat C. Perceived confidence and experience in oral surgery among final year undergraduate students in a UK dental school. Br Dent J 2018; 224: 177-182.
Gilmour A S, Welply A, Cowpe J G, Bullock A D, Jones R J. The undergraduate preparation of dentists: Confidence levels of final year dental students at the School of Dentistry in Cardiff. Br Dent J 2016; 221: 349-354.
Coulthard P, Kazakou I, Koron R, Worthington H V. Referral patterns and the referral system for oral surgery care. Part 1: general dental practitioner referral patters. Br Dent J 2000; 188: 142-145.
Patel J, Fox K, Grieveson B, Youngson C C. Undergradutate training as preparation for vocational training in England: a survey of vocational dental practitioners' and their trainers' views. Br Dent J 2006; 201 (Spec Iss): 9-15.
Cottrell D A, Reebye U N, Blyer S M, Hunter M J, Mehtra N. Referral patterns of general dental practitioners for oral surgical procedures. J Oral Maxillofac Surg 2007; 65: 686-690.
Absi E G, Satterthwaite J, Shepherd J P, Thomas D W. The appropriateness of referral of medically compromised dental patients to hospital. Br J Oral Maxillofac Surg 1997; 35: 133-136.
Bullock A D, Belfield C R, Butterfield S, Ribbins P M, Frame J W. Continuing education courses in dentistry: assessing impact on practice. Med Educ 1999; 33: 484-488.
Grant J. The good CPD guide. A practical guide to managed continuing professional development in medicine. 2nd ed. Abingdon: Taylor & Francis, 2011.
Forsetlund L, Bjørndal A, Rashidian A et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009; CD003030. DOI: 10.1002/14651858.
The Faculty of General Dental Practice (UK). The impact of continuing professional development in dentistry. 2011. Available at https://www.fgdp.org.uk/sites/fgdp.org.uk/files/docs/in-practice/amps-online/final%20impact%20of%20cpd%20on%20dentistry%20november%202011.pdf (accessed March 2019).
Davies B J, Macfarlane F. Clinical decision making by dentists working in the NHS General Dental Services since April 2006. Br Dent J 2010; 209: E17.
Halai T, Yates J M. Assessment of oral surgery referrals from primary care to a regional dental hospital. Oral Surg 2014; 7: 168-176.
Scottish Dental Clinical Effectiveness Programme. Oral health management of patients prescribed bisphosphonates. 2011. Available at http://www.sdcep.org.uk/published-guidance/bisphosphonates/ (accessed March 2019).
Cowpe J, Plasschaert A, Harzer W, Vinkka-Puhakka H, Walmsley A D. Profile and competences for the graduating European dentist - update 2009. Eur J Dent Educ 2010; 14: 193-202.
Brand H S, van der Cammen C C J, Roorda S M E, Baart J A. Tooth extraction education at dental schools across Europe. BDJ Open 2015; 1: 15002.
Barnsley L, Lyon P M, Ralston S J et al. Clinical skills in junior medical officers: a comparison of self-reported confidence and observed competence. Med Educ 2004; 38: 358-367.
Davis D A, Mazmanian P E, Fordis M, Van Harrison R, Thorpe K E, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 2006; 296: 1094-1102.
General Dental Council. Enhanced CPD guidance for dental professionals. 2018. Available at https://www.gdc-uk.org/professionals/cpd/enhanced-cpd (accessed March 2019).
Gibbs G. Learning by doing: a guide to teaching and learning methods. Oxford: FEE, 1988.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Savla, A., Sanalla, A. & Tanna, N. How do minor oral surgery courses impact the confidence levels of general dental practitioners?. Br Dent J 226, 512–517 (2019). https://doi.org/10.1038/s41415-019-0151-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0151-8