Abstract
Case report A case of a 59-year-old female patient who attended with a history of periodontitis, who had been successfully treated and maintained for several years, is described. Following a full periodontal assessment, the patient was diagnosed with 'generalised periodontitis; stage IV; grade C; currently stable'.
Conclusion The present case report exemplifies the use of the 2017 classification system in a successfully treated and well-maintained patient whose treatment need is supportive periodontal treatment. It recognises the fact that, by staging and grading, the patient is a high-risk periodontitis patient due to historical disease experience, but also that following successful therapy and maintenance she is currently 'stable' with no need for active periodontal therapy.
Similar content being viewed by others
Key points
-
Illustrates the application of the BSP implementation plan for the 2017 world workshop classification of periodontal and peri-implant diseases and conditions.
-
Exemplifies the use of the 2017 classification system in a successfully treated and well-maintained patient whose treatment need is supportive periodontal treatment.
-
Demonstrates the diagnostic approach for a patient with generalised periodontitis, stage IV, grade C, who had been successfully treated and maintained for several years.
Introduction
Periodontitis is a chronic inflammatory disease characterised clinically by the presence of periodontal pockets and loss of periodontal attachment. Radiological bone loss is evident, as measured from a reference point 1-2 mm apical to the cementoenamel junction (CEJ) or an alternative reference point such as the margin of a restoration, and/or as clinical attachment loss (CAL) measured by probing from the CEJ or an alternative reference point. There are several considerations for the clinician when assessing a patient with periodontitis in order to be able to manage both the patient and their disease effectively. Managing the patient requires knowledge of their historical disease experience and its rate of progression before periodontal therapy. This is obtained by 'staging' and 'grading'. Managing a patient's disease also requires knowledge of their current periodontal status as determined by probing pocket depth charting and measuring bleeding on probing. In summary, the following require assessment:
-
1.
The amount of periodontal tissue loss that has already occurred
-
2.
The risk of future attachment loss and the identification of possible risk factors that may determine that risk, through a medical, dental and social history
-
3.
Current levels of periodontal inflammation, which may be minimal in a patient who has been successfully treated.
In the new 2017 classification, the first two domains are captured by the new staging and grading procedure.1,2 Furthermore, the new classification, for the first time, provides formal definitions of periodontal health and recognises that periodontal health and limited amounts of gingival inflammation can exist on a reduced but currently healthy periodontium (disease stability) following periodontal therapy.1,3
In this case presentation, we report on a patient with severe periodontitis who was successfully treated and maintained for several years. We demonstrate step-by-step how the BSP recommendations for implementation of the 2017 classification system can be applied in practice to reach an appropriate periodontal diagnosis and a diagnostic statement that also embraces disease extent, activity status and associated risk factors.
Case report
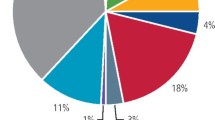
A 59-year-old female patient who had recently moved from abroad presented at her dentist seeking periodontal care. She had received periodontal treatment and maintenance at a university dental clinic for the previous eight years. She was a former smoker, who had smoked approximately 20-30 cigarettes per day before successfully quitting 12 years previously. There were no other documented periodontal risk factors and she was medically fit and well. Clinical examination revealed clear and obvious interproximal recession/clinical attachment loss (Fig. 1). Given the history of periodontitis reported by the patient and the evidence of interproximal clinical attachment loss due to periodontitis, a BPE was not appropriate and a full periodontal assessment, including a detailed pocket chart (DPC) was indicated (Fig. 2).
The presence of interproximal attachment and bone loss consistent with periodontitis led to this patient being classified as a periodontitis patient, but this alone was insufficient to determine her current periodontal status and therefore her treatment needs.
There was bleeding on probing (BoP) in only 13 from a total of 144 sites (<10%). None of the sites with probing pocket depth (PPD) of 4 mm bled on probing, indicating they were likely to be stable 4 mm sites ('closed pockets'). Therefore, a diagnosis of 'periodontitis, currently stable' could be made (PPD ≤4mm, no BoP at 4 mm sites and <10% BoP).
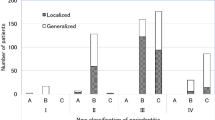
The patient also provided periapical radiographs, which were taken 13 months previously (Fig. 3). The periapical radiographs showed bone loss due to periodontitis on virtually all teeth (>30% of teeth affected). Maximum bone loss extended to the apical third of the root, showing 70% bone loss on tooth 14. Staging was therefore at stage IV (maximum bone loss extending into apical third) and grading at grade C (70% bone loss in a 59-year-old patient, that is, bone loss/age ratio >1).
The definitive diagnostic statement was: generalised periodontitis; stage IV, grade C; currentlystable.Risk factors: ex-smoker. The patient will always be a periodontitis patient, with evidence of high disease susceptibility (as indicated by grade C), requiring careful and intensive periodontal maintenance, risk factor control and monitoring.
Discussion/summary
This report concludes a series of case reports4,5,6,7 illustrating how to diagnose a patient with a history of periodontitis according to the 2017 classification of periodontal and peri-implant diseases and conditions by following the BSP implementation plan.1 It is important to note that in all of these case reports we do not present or discuss all aspects of patient assessment, but rather focus on those diagnostic aspects that are directly relevant for disease classification according to the BSP implementation plan.1
One of the main features of the new 2017 classification system is that periodontal health and gingival diseases are clearly defined for the first time, both on an intact and reduced periodontium.3 For example, a diagnosis of gingivitis requires a minimum amount of inflamed gingival sites (at least 10%). Gingivitis can exist both on an intact periodontium (that is, no clinical attachment loss/alveolar bone loss) and on a reduced periodontium. In the latter case, where the attachment loss/bone loss has occurred for reasons unrelated to periodontitis (such as surgical crown lengthening) it is called gingivitis, but where the clinical attachment and bone loss was due to periodontitis, the term 'gingival inflammation' is employed, because a single patient cannot represent a case of periodontitis and simultaneously also a case of gingivitis. Hence, such a patient would be a periodontitis patient with gingival inflammation.
In a patient with periodontitis, successful treatment and maintenance will result in resolution of periodontal pockets and inflammation. In such patients, probing depths of up to and including 4 mm may be consistent with (current) periodontal stability, if <10% of sites with PPD up to 3 mm are BoP and no sites with PPD 4 mm are BoP. If 10% or more of sites with PPD up to 3 mm exhibit BoP but no sites with PPD 4 mm bleed, then this is 'gingival inflammation in a patient with a history of periodontitis' and they are said to be 'in remission'. At first glance, these thresholds may appear confusing; however, the basic concept is that in a treated periodontitis patient, PPDs of 4 mm are consistent with a stable situation as long as there is no BoP at those 4 mm sites. The 4 mm non-bleeding site is referred to as a 'closed pocket' as its risk of future breakdown is significantly reduced relative to sites with PPD of 5 mm or greater; the closed pocket is the desired endpoint of therapy.8 In the BSP implementation plan, this situation is therefore identified as either:
-
1.
'Currently stable' periodontitis (<10% BoP at sites with PPD ≤3mm and no BoP at 4 mm sites)
-
2.
Periodontitis 'currently in remission' (at least 10% of sites with PPD ≤3mm bleed on probing and no BoP at 4 mm sites).
As soon as there is BoP at a site with 4 mm PPD or there are PPD ≥5 mm, the patient is classified as 'currently unstable'.
While a discussion of the therapeutic implications of the above diagnoses is beyond the scope of this paper, it is recognised that these criteria are quite stringent. In particular, it should be noted that following initial periodontal treatment, resolution of increased probing depths takes time, and PPD ≥5 mm at re-evaluation do not necessarily imply incomplete treatment. Even in the longer term, patients with 5-6 mm PPD without BoP may, in individual cases, be considered stable. This should be a matter of clinical judgement. However, as evident from retrospective studies in large Swiss cohorts, residual probing depths ≥6 mm are associated with a markedly increased risk of further attachment loss and tooth loss.9
In the presented patient, periodontal treatment and maintenance had resulted in resolution of periodontal inflammation. There were no probing depths 5 mm or more, and BoP was limited to fewer than 10% of sites with PPD of 3 mm or less. Hence, the patient was classified as a periodontitis patient, who was 'currently stable'. However, designation as 'currently stable' does not mean that the proverbial foot can be taken off the pedal. Classification as stage IV, grade C indicates severe periodontitis with high disease susceptibility. Smoking will likely have contributed to the periodontal tissue loss in this patient, but conversely, the fact that this risk factor has been successfully managed for many years bodes well for continued maintenance.10
References
Dietrich T, Ower P, Tank M et al. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions - implementation in clinical practice. Br Dent J 2019; 226: 16-22.
Papapanou P N, Sanz M, Buduneli Net al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 2018; 45 (Spec Iss): S162-S170.
Chapple I L C, Mealey B L, Van Dyke T E et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 2018; 45: S68-S77.
Walter C, Chapple I L C, Ower P et al. Periodontal diagnosis in the context of the BSP implementation plan for the 2017 classification system of periodontal diseases and conditions: presentation of a pair of young siblings with periodontitis. Br Dent J 2019; 226: 23-26.
Walter C, Ower P, Tank M et al. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions: Presentation of a middle-aged patient with localised periodontitis. Br Dent J 2019; 226: 98-100.
Wadia R, Walter C, Chapple I L Cet al. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions: presentation of a patient with periodontitis localised to the molar teeth. Br Dent J 2019; 226: 180-182.
Walter C, Chapple I L C, Ower P et al. Periodontal diagnosis in the context of the BSP implementation plan for the 2017 classification system of periodontal diseases and conditions: Presentation of a patient with a history of periodontal treatment. Br Dent J 2019; 226: 265-267.
Wennstrom J L, Tomasi C, Bertelle A, Dellasega E. Full-mouth ultrasonic debridement versus quadrant scaling and root planing as an initial approach in the treatment of chronic periodontitis. J Clin Periodontol 2005; 32: 851-859.
Matuliene G, Pjetursson B E, Salvi G E et al. Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 2008; 35: 685-695.
Warnakulasuriya S, Dietrich T, Bornstein M M et al. Oral health risks of tobacco use and effects of cessation. Int Dent J 2010; 60: 7-30.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, C., Chapple, I., Ower, P. et al. Periodontal diagnosis in the context of the BSP implementation plan for the 2017 classification system of periodontal diseases and conditions: presentation of a patient with severe periodontitis following successful periodontal therapy and supportive periodontal treatment. Br Dent J 226, 411–413 (2019). https://doi.org/10.1038/s41415-019-0143-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0143-8
This article is cited by
-
Implementing the 2017 Classification of Periodontal and Peri-Implant Diseases - how are we doing in the South West region of the UK?
British Dental Journal (2021)
-
Evidence-based, personalised and minimally invasive treatment for periodontitis patients - the new EFP S3-level clinical treatment guidelines
British Dental Journal (2020)