Abstract
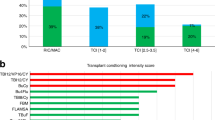
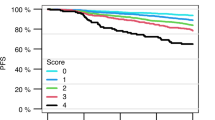
A conditioning regimen is an essential prerequisite of allogeneic hematopoietic stem cell transplantation for patients with myelodysplastic syndrome (MDS). However, the optimal conditioning intensity for a patient may be difficult to establish. This study aimed to identify optimal conditioning intensity (reduced-intensity conditioning regimen [RIC] or myeloablative conditioning regimen [MAC]) for patients with MDS. Overall, 2567 patients with MDS who received their first HCT between 2009 and 2019 were retrospectively analyzed. They were divided into a training cohort and a validation cohort. Using a machine learning-based model, we developed a benefit score for RIC in the training cohort. The validation cohort was divided into a high-score and a low-score group, based on the median benefit score. The endpoint was progression-free survival (PFS). The benefit score for RIC was developed from nine baseline variables in the training cohort. In the validation cohort, the hazard ratios of the PFS in the RIC group compared to the MAC group were 0.65 (95% confidence interval [CI]: 0.48–0.90, P = 0.009) in the high-score group and 1.36 (95% CI: 1.06–1.75, P = 0.017) in the low-score group (P for interaction < 0.001). Machine-learning-based scoring can be useful for the identification of optimal conditioning regimens for patients with MDS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data used in this study are available from the corresponding author upon reasonable request.
References
Cazzola M. Myelodysplastic syndromes. N Engl J Med. 2020;383:1358–74.
Platzbecker U. Treatment of MDS. Blood. 2019;133:1096–107.
de Witte T, Bowen D, Robin M, Malcovati L, Niederwieser D, Yakoub-Agha I, et al. Allogeneic hematopoietic stem cell transplantation for MDS and CMML: recommendations from an international expert panel. Blood. 2017;129:1753–62.
Gagelmann N, Kröger N. Dose intensity for conditioning in allogeneic hematopoietic cell transplantation: can we recommend “when and for whom” in 2021? Haematologica. 2021;106:1794–804.
McDonald GB, Sandmaier BM, Mielcarek M, Sorror M, Pergam SA, Cheng G-S, et al. Survival, nonrelapse mortality, and relapse-related mortality after allogeneic hematopoietic cell transplantation: comparing 2003–2007 versus 2013–2017 cohorts. Ann Intern Med. 2020;172:229.
Sengsayadeth S, Savani BN, Blaise D, Malard F, Nagler A, Mohty M. Reduced intensity conditioning allogeneic hematopoietic cell transplantation for adult acute myeloid leukemia in complete remission – a review from the Acute Leukemia Working Party of the EBMT. Haematologica. 2015;100:859–69.
Kröger N, Iacobelli S, Franke G-N, Platzbecker U, Uddin R, Hübel K, et al. Dose-reduced versus standard conditioning followed by allogeneic stem-cell transplantation for patients with myelodysplastic syndrome: a prospective Randomized Phase III Study of the EBMT (RICMAC Trial). J Clin Oncol. 2017;35:2157–64.
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. J Clin Oncol. 2017;35:1154–61.
Rashidi A, Meybodi MA, Cao W, Chu H, Warlick ED, Devine S, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation in myelodysplastic syndromes: systematic review and meta-analysis. Biol Blood Marrow Transplant. 2020;26:e138–41.
Shimoni A, Robin M, Iacobelli S, Beelen D, Mufti GJ, Ciceri F, et al. Allogeneic hematopoietic cell transplantation in patients with myelodysplastic syndrome using treosulfan based compared to other reduced‐intensity or myeloablative conditioning regimens. A report of the chronic malignancies working party of the EBMT. Br J Haematol. 2021;195:417–28.
Aoki K, Ishikawa T, Ishiyama K, Aoki J, Itonaga H, Fukuda T, et al. Allogeneic haematopoietic cell transplantation with reduced-intensity conditioning for elderly patients with advanced myelodysplastic syndromes: a nationwide study. Br J Haematol. 2015;168:463–6.
Shimomura Y, Hara M, Konuma T, Itonaga H, Doki N, Ozawa Y. et al. Allogeneic hematopoietic stem cell transplantation for myelodysplastic syndrome in adolescent and young adult patients. Bone Marrow Transplant. 2021;56:2510–7. https://doi.org/10.1038/s41409-021-01324-8.
Basu S, Sussman JB, Hayward RA. Detecting heterogeneous treatment effects to guide personalized blood pressure treatment: a modeling study of randomized clinical trials. Ann Intern Med. 2017;166:354–60.
Chen S, Tian L, Cai T, Yu M. A general statistical framework for subgroup identification and comparative treatment scoring. Biometrics. 2017;73:1199–209.
VanderWeele TJ, Knol MJ. Interpretation of subgroup analyses in randomized trials: heterogeneity versus secondary interventions. Ann Intern Med. 2011;154:680–3.
Baum A, Scarpa J, Bruzelius E, Tamler R, Basu S, Faghmous J. Targeting weight loss interventions to reduce cardiovascular complications of type 2 diabetes: a machine learning-based post-hoc analysis of heterogeneous treatment effects in the Look AHEAD trial. Lancet Diabetes Endocrinol. 2017;5:808–15.
Huling JD, Yu M. Subgroup identification using the personalized package. J Stat Softw. 2021;98:1–60. https://doi.org/10.18637/jss.v098.i05.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-Intensity Conditioning Regimen Workshop: defining the dose spectrum. Report of a workshop convened by the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2009;15:367–9.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Stekhoven DJ, Bühlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinforma Oxf Engl. 2012;28:112–8.
Waljee AK, Mukherjee A, Singal AG, Zhang Y, Warren J, Balis U, et al. Comparison of imputation methods for missing laboratory data in medicine. BMJ Open. 2013;3:e002847.
Shah AD, Bartlett JW, Carpenter J, Nicholas O, Hemingway H. Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol. 2014;179:764–74.
Slade E, Naylor MG. A fair comparison of tree-based and parametric methods in multiple imputation by chained equations. Stat Med. 2020;39:1156–66.
Atallah E, Logan B, Chen M, Cutler C, Deeg J, Jacoby M. et al. Comparison of patient age groups in transplantation for myelodysplastic syndrome: the medicare coverage with evidence development study. JAMA Oncol. 2020;6:486–93. https://doi.org/10.1001/jamaoncol.2019.5140.
Gilleece MH, Labopin M, Yakoub-Agha I, Volin L, Socié G, Ljungman P, et al. Measurable residual disease, conditioning regimen intensity, and age predict outcome of allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first remission: a registry analysis of 2292 patients by the Acute Leukemia Working Party E. Am J Hematol. 2018;93:1142–52.
Gilleece MH, Labopin M, Savani BN, Yakoub-Agha I, Socié G, Gedde-Dahl T, et al. Allogeneic haemopoietic transplantation for acute myeloid leukaemia in second complete remission: a registry report by the Acute Leukaemia Working Party of the EBMT. Leukemia. 2020;34:87–99.
Saraceni F, Labopin M, Forcade E, Kröger N, Socié G, Niittyvuopio R, et al. Allogeneic stem cell transplant in patients with acute myeloid leukemia and karnofsky performance status score less than or equal to 80%: a study from the acute leukemia working party of the European Society for Blood and Marrow Transplantation (EBMT). Cancer Med. 2021;10:23–33.
Rambaldi A, Grassi A, Masciulli A, Boschini C, Micò MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16:1525–36.
Konuma T, Kondo T, Mizuno S, Doki N, Aoki J, Fukuda T, et al. Conditioning intensity for allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients with poor-prognosis cytogenetics in first complete remission. Biol Blood Marrow Transplant. 2020;26:463–71.
Fein JA, Shimoni A, Labopin M, Shem-Tov N, Yerushalmi R, Magen H, et al. The impact of individual comorbidities on non-relapse mortality following allogeneic hematopoietic stem cell transplantation. Leukemia. 2018;32:1787–94.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of allogeneic transplantation for acute myeloid leukemia with genomic evidence of residual disease. J Clin Oncol. 2020;38:1273–83.
Passweg JR, Labopin M, Cornelissen J, Volin L, Socié G, Huynh A, et al. Conditioning intensity in middle-aged patients with AML in first CR: no advantage for myeloablative regimens irrespective of the risk group–an observational analysis by the Acute Leukemia Working Party of the EBMT. Bone Marrow Transplant. 2015;50:1063–8.
Lindsley RC, Saber W, Mar BG, Redd R, Wang T, Haagenson MD, et al. Prognostic mutations in myelodysplastic syndrome after stem-cell transplantation. N Engl J Med. 2017;376:536–47.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transplant. 2020;55:1114–25.
Acknowledgements
The authors thank all the physicians and data managers at the centers who contributed to the collection of data on transplantation for the Japanese Data Center for Hematopoietic Cell Transplantation and Transplant Registry Unified Management Program 2. We express our gratitude to the Japan Society of Clinical Research for their support.
Author information
Authors and Affiliations
Contributions
YS designed the study, developed the models, performed the statistical analysis, and wrote the first draft of the manuscript. Sho Komukai and TK contributed to the development of the model and data analysis. Sho Komukai, TK, TS, Shuhei Kurosawa, and KI critically reviewed the data analysis and manuscript. All the other authors contributed to data collection. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shimomura, Y., Komukai, S., Kitamura, T. et al. Identifying the optimal conditioning intensity for stem cell transplantation in patients with myelodysplastic syndrome: a machine learning analysis. Bone Marrow Transplant 58, 186–194 (2023). https://doi.org/10.1038/s41409-022-01871-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01871-8