Abstract
Acute lung injury (ALI) is a sudden onset systemic inflammatory response. ALI causes severe morbidity and death and currently no effective pharmacological therapies exist. Natural products represent an excellent resource for discovering new drugs. Screening anti-inflammatory compounds from the natural product bank may offer viable candidates for molecular-based therapies for ALI. In this study, 165 natural compounds were screened for anti-inflammatory activity in lipopolysaccharide (LPS)-challenged macrophages. Among the screened compounds, flavokawain B (FKB) significantly reduced LPS-induced pro-inflammatory IL-6 secretion in macrophages. FKB also reduced the formation of LPS/TLR4/MD2 complex by competitively binding to MD2, suppressing downstream MAPK and NF-κB signaling activation. Finally, FKB treatment of mice reduced LPS-induced lung injury, systemic and local inflammatory cytokine production, and macrophage infiltration in lungs. These protective activities manifested as increased survival in the ALI model, and reduced mortality upon bacterial infection. In summary, we demonstrate that the natural product FKB protects against LPS-induced lung injury and sepsis by interacting with MD2 and inhibiting inflammatory responses. FKB may potentially serve as a therapeutic option for the treatment of ALI.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) is a common critical illness that seriously injures the respiratory system. Recently, ALI was reclassified as mild to moderate acute respiratory distress syndrome [1]. Histopathological features of ALI include recruitment of neutrophils, interstitial edema, destruction of epithelial integrity, and excessive production of inflammatory cytokines. Although ALI causes significant morbidity and mortality in the critically ill patient population, there are no FDA approved treatments for ALI [2]. Thus, there is an urgent need to identify new pharmacological targets and develop novel and effective drugs for ALI.
One of the key pathophysiological features of ALI is uncontrolled or excessive inflammatory response, which can be triggered by damage-associated molecular patterns (such as histones, HMGB1, etc.) or pathogen-associated molecular patterns (such as lipopolysaccharide (LPS), lipoteichoic acid, etc.) [3]. LPS, an important component of Gram-negative bacteria cytoderm, is commonly administered to mice to produce a clinically relevant model of ALI [4]. Toll-like receptor 4 (TLR4) is the main receptor of LPS. LPS activates TLR4 by first binding to a TLR4 co-receptor called myeloid differentiation protein-2 (MD2). This binding then initiates LPS-MD2-TLR4 complex formation, which is necessary for signal propagation inside the cell. Intracellular adaptor molecules are recruited to the complex and convey downstream signal transduction involving mitogen-activated protein kinases (MAPKs) and nuclear factor-κB (NF-κB), leading to a transcription of inflammatory cytokines [5]. In this signaling pathway, LPS/TLR4/MD2 may represent an important node for therapeutic intervention of ALI.
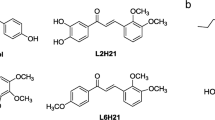
Natural products represent an excellent resource for new drug discovery. In the present study, 165 natural products from different origins (Supplementary Table 1) were evaluated for anti-inflammatory effects in LPS-challenged mouse primary macrophages (MPMs). Of the screened compounds, flavokawain B (FKB; Fig. 1b), a natural chalcone isolated from the root extracts of kava-kava plants (Piper methysticum), displayed robust anti-inflammatory activity without MPM cytotoxicity (Fig. 1a). Previous studies have shown that FKB may reduce turmor burdon [6,7,8] and initiate anti-inflammatory responses [9]. The anti-inflammatory activity of FKB is attributed to inhibition of the NF-κB signaling pathway [9]. However, the detailed mechanisms underlying the observed effects remain elusive. Here, we demonstrated that FKB protected against LPS-induced ALI by physically interacting with TLR4 co-receptor MD2. This interaction reduced LPS/TLR4/MD2 complex-mediated inflammatory responses in vivo and in vitro. Our findings also indicate that FKB is a novel MD2 inhibitor and could be a potential therapeutic candidate for ALI.
a Anti-inflammatory effects and toxicity of 165 natural compounds were evaluated in LPS-challenged MPMs. Results are shown as IL-6 inhibition rate compared to LPS (Y-axis). Cytotoxicity of the tested compounds was determined in MPMs by MTT. Results were presented as viable cell number compared to vehicle-control (X-axis). b The chemical structure of flavokawain B (FKB). Levels of IL-6 (c) and TNF-α (d) protein in cell culture media of LPS-challenged MPMs. Data were normalized to total protein concentration from the same plate and presented as % LPS. mRNA levels of inflammatory cytokines IL-6 (e), TNF-α (f), IL-1β (g), and adhesion molecules ICAM-1 (h) and VCAM-1 (i). Data were normalized to β-actin and control groups. Results were presented as Mean ± SEM, n = 3, *P < 0.05 compared to LPS-treated group.
Materials and methods
Reagents and antibodies
A 165 natural product library was purchased from Topscience (Shanghai, China). The detailed information of the natural compounds is listed in Supplementary Table 1. FKB (Cat. No. 19309-14-9) was purchased from Zhongke Quality Inspection (Beijing, China). LPS (Cat. No. L6386-100MG) was obtained from Sigma-Aldrich (St. Louis, MO). Antibodies against p38 (Cat. No. 9212S), phosphorylated (p-) p38 (Cat. No. 9211S), c-Jun N-terminal kinase (JNK; Cat. No. 9252S), p-JNK (Cat. No. 4668S), extracellular signal-regulated kinase (ERK; Cat. No. 4695S), p-ERK (Cat. No. 4695S), p-p65 (Cat. No. 3033S) and inhibitor of κB-α (IκB-α; Cat. No. 4812S) were from Cell Signaling Technology (Danvers, MA). Antibody against GAPDH (Cat. No. AB-P-R001) was obtained from Goodhere (Hangzhou, China). Antibodies against NF-κB P65 (Cat. No.sc-8008), TLR4 (Cat. No. sc-293072), MD2 (Cat. No. sc-80183), and macrophage markers CD68 (Cat. No. sc-20060) and F4/80 (Cat. No. sc-377009) were purchased from Santa Cruz Biotechnology (Dallas, TX). IL-6 antibody (Cat. No. 66146-1-lg) was obtained from Proteintech (Wuhan, China). Recombinant human MD2 (rhMD2, Cat. No. 1787-MD-050/CF) protein was obtained from R&D Systems (Minneapolis, MN). Human recombinant TLR4 ectodomain (ECD) protein (Cat.No.10146-H08B, His Tag) was purchased from Sinobiological Inc. (Beijing, China). Mouse TNF-α (Cat. No. 85-88-7324-76) and IL-6 ELISA kits (Cat. No. 85-88-7064-76) were obtained from eBioscience (San Diego, CA).
Cell isolation and culture
Mouse primary peritoneal macrophages (MPMs) were prepared from C57BL/6 mice as described in our previous study [10]. MPMs were cultured and expanded in RPMI-1640 medium with 10% FBS. Mouse macrophage line RAW264.7 stably expressing NF-κB-RE-EGFP reporter (RAW264.7-NF-κB-RE-EGFP) was constructed, as described in our previous study [11]. RAW264.7-NFkB-RE-EGFP cells were cultured and expanded in MEM-α medium containing 10% FBS and 0.1 μg/mL puromycin.
ELISA
TNF-α and IL-6 proteins in cell culture media were measured by ELISA, according to the manufacture’s recommendations. Data were normalized to total proteins in the respective cell lysates, and expressed as a percentage of the LPS-challenged condition. In addition, levels of TNF-α and IL-6 in serum and bronchoalveolar lavage fluid (BALF) of mice were determined by ELISA.
MTT assay
MPM cells were seeded into 96-well plates at 10 000 cells/well and cultured overnight. Cells were then treated with the 165 natural products at 10 μM for 24 h. MTT reagent (Cat. No. M8180-250, Solarbio, Beijing, China) was added to each well and cells were incubated for 4 h. The media was then removed and the purple crystals were dissolved by adding DMSO. Finally, absorbance was detected at 490 nm using SpectraMax M5 Multi-Mode Microplate Reader (Molecular Devices, San Jose, CA). Cell viability was expressed as the percentage of the untreated controls.
Surface plasmon resonance analysis
The binding affinity of FKB to rhMD2 and rhTLR4 protein was determined by Surface Plasmon Resonance (SPR), using a Biacore T200 instrument (GE Healthcare Inc., Piscataway, NJ) with a CM7 sensor chip (Cat. No. 29-1470-20, GE Healthcare Inc., Piscataway, NJ). Briefly, rhMD2 or rhTLR4 proteins were loaded to the sensors using Amine coupling kit (Cat. No. BR-1000-50s, GE Healthcare Inc., Piscataway, NJ). FKB samples (0, 0.203, 1.625, 6.25, 12.5, 25 or 50 μM) were prepared in running buffer (PBS, 0.5% P20 and 5% DMSO) and injected at a flow rate of 30 μL/min for a 180 s association phase, followed by a 270 s dissociation phase at 25 °C. Data were analyzed using Biacore™ T200 software EV. Kd values were calculated using global fitting of the kinetic data from various concentrations of FKB by the 1:1 Langmuir binding model.
LPS displacement assay
The ability of FKB to interfere with LPS binding to MD2 was determined using a cell-free assay. 96-well Clear Polystyrene Microplates (Cat. No. 9018, Coring) were blocked with 3% BSA at 4 °C overnight. After washing with PBST, 500 μg/mL LPS was added and plates were incubated for 1 h at room temperature. After an additional PBST wash, samples were added, including: (1) a vehicle control (10 mM Tris-HCl buffer, pH 7.5); (2) rhMD2 (1 μg/mL in 10 mM Tris-HCl buffer, pH 7.5); (3) a rhMD2-FKB mixture prepared by incubating rhMD2 (1 μg/mL in 10 mM Tris-HCl buffer, pH 7.5) with FKB (10, 20, 50 and 100 μM) at room temperature on a shaker for 1 h. Samples were incubated in LPS-coated plates at room temperature for 2 h. Plates were washed with PBST and anti-MD2 primary antibody was added for 2 h at room temperature. Horseradish peroxidase (HRP)-labeled secondary antibody was then added for 1 h at room temperature. HRP activity was determined using SpectraMax M5 at 450 nm after the addition of TMB substrate (Cat. No. 34022, Thermo Scientific, Waltham, MA).
Molecular docking of flavokawain B to MD2
The molecular docking simulation was performed using AutoDock version 4.2.6. The crystal structure of human MD2 lipid IVa complex (PDB code 2E59) was obtained from Protein Data Bank. The AutoDock Tools version 1.5.6 package was applied to generate the docking input files and analyze the docking results. A 60 × 60 × 60-point grid box with a spacing of 0.375 Å between the grid points was implemented. The affinity maps of MD2 were calculated by AutoGrid. One hundred Lamarckian genetic algorithm runs with default parameter settings were processed. The hydrogen bonds and bond lengths within the interactions of complex protein–ligand conformations were also analyzed.
Bis-ANS fluorescence displacement assays
Fluorescence displacement assays were also performed to study the interaction between FKB and MD2. Briefly, 5 μM 4,4′-bis(phenylamino)-[1,1′-binaphthalene]-5,5′-disulfonic acid (bis-ANS, Cat. No. 5908/10, Tocris, Carlsbad, CA) and 5 nM rhMD2 were mixed in PBS (pH 7.4) and allowed to reach stable fluorescence under excitation at 385 nm. FKB, at 2.5, 5, 10, 20, and 30 μM, was then added for 5 min. The relative fluorescence unit emitted at 440–570 nm was measured using SpectraMax M5 at 25 °C in 5 nm path-length quartz cuvettes.
BALF preparation and analysis
A tracheal cannula was inserted into the primary bronchus, and BALF was collected through the cannula by using Ca2+/Mg2+-free PBS. Approximately 0.8 mL BALF was acquired and centrifuged at 1000 × g for 15 min at 4 °C. The supernatant was immediately stored at −80 °C for protein concentration and cytokine determination. The sediment was resuspended in 50 μL 0.9% saline for determination of the total cell number and neutrophil counts. Total cell number was acquired using Countstar (ALIT Life Science, shanghai China). Neutrophil count was determined by counting 200 cells on a smear prepared by Wright–Giemsa stain (Nanjing Jiancheng Bioengineering Institute, Nanjing, China).
Western blotting
Samples were lysed using radioimmunoprecipitation assay buffer. Total protein levels were measured by the Bradford assay (Cat. No. 5000205, Bio-Rad, Hercules, CA). Protein samples were boiled in loading buffer (cat. No. FD006, Hangzhou FUDE biological Technology, Hangzhou, China) for 10 min and then separated by 10% SDS-PAGE and transferred onto a PVDF membrane (Cat. No. 1620177, Bio-Rad, Hercules, CA). Membranes were blocked with 5% nonfat-milk in Tris-buffered saline containing 0.05% Tween 20 (TBST) for 1.5 h at room temperature. The membranes were incubated with primary antibodies at 4 °C overnight. The membranes were then washed with TBST and incubated with HRP-conjugated secondary antibodies (1:10000) for 1 h at room temperature. Blots were then visualized using an enhanced chemiluminescence reagent (Cat. No. P10300, NCM Biotech, Suzhou, China). The density of the immunoreactive bands was analyzed using ImageJ software (NIH, Bethesda, MD).
Immunoprecipitation assay for MD2–TLR4 complexes determination
Samples were lysed with an extraction buffer containing Mammalian Protein Extraction reagent (Cat. No. 78501; Thermo Fisher) and protease and phosphatase inhibitor cocktail (Cat. No. P8340; Sigma-Aldrich). Samples were centrifuged at 15 000 × g for 10 min at 4 °C. MD2 antibody was added to 500 μg protein, and samples were gently rotated at 4 °C overnight. The immune complexes were precipitated with protein A + G agarose (Cat. No. P2012, Beyotime, Shanghai, China), and the precipitates were washed four times with ice-cold PBS. Finally, the proteins were released by boiling in sample buffer, followed by Western blotting analysis as described above.
Myeloperoxidase activity assay
To quantify neutrophil infiltration, myeloperoxidase (MPO) activity in homogenized lung tissues was measured using a MPO Detection Kit (Cat. No. A044, Nanjing Jiancheng Bioengineering Institute, Nanjing, China). Lung tissues were homogenized in 1 mL of 50 mM potassium PBS (pH 6.0) containing 0.5% hexadecyltrimethylammonium hydroxide. Samples were centrifuged at 12 000 × g at 4 °C for 20 min. Then, 10 μL of the supernatant was transferred to PBS containing 0.17 mg/mL 3,3′-dimethoxybenzidine and 0.0005% hydrogen peroxide (H2O2). MPO activity in the supernatant was determined by measuring absorbance at 460 nm and presented as U/g protein.
Assay of cellular NF-κB p65 translocation
NF-κB activation was assessed by Cellular NF-κB p65 Translocation Kit (cat. No. SN368, Beyotime Biotech, Shanghai, China) following manufacturer’s protocol.
RNA extraction and RT-qPCR assay
Cultured cells and lung tissues were homogenized using TRIZOL (Invitrogen, Carlsbad, CA). Total RNA concentration and purity was measured using an nanodrop 2000 (Thermo Scientific, San Diego, CA). Samples with OD ratio of A260/A280 within 1.8–2.2 were used. RT-qPCR was performed using the M-MLV Platinum RT-qPCR Kit (Invitrogen, Carlsbad, CA) in an Eppendorf Realplex4 instrument (Eppendorf, Hamburg, Germany). Primers for genes encoding TNF-α, IL-6, IL-1β, intercellular cell adhesion molecule 1 (ICAM-1), and vascular cell adhesion molecule 1 (VCAM-1) were obtained from Invitrogen (Carlsbad, CA). Transcript levels were normalized to β-actin reference gene.
Mouse model of ALI
All animal care and experimental procedures were approved by Wenzhou Medical University Animal Policy and Welfare Committee (Approval Document No. wydw2016-0124). Studies were performed in full conformity with the NIH Guide for the Care and Use of Laboratory Animals.
Forty male C57BL/6 mice, weighing 18–22 g, were obtained from GemPharmatech Co., Ltd. (Nanjing, China). All animals were housed at a constant room temperature with a 12:12 h light/dark cycle and given food and water freely. Mice were acclimatized to the laboratory for 7 days, and were randomly assigned to one of five groups (n = 8): vehicle control (CON), LPS-induced ALI (LPS; 5 mg/kg, iv.), FKB-treated mice (FKB; 20 mg/kg), LPS-induced ALI mice treated with 10 mg/kg of FKB (LPS + FKB 10), LPS-induced ALI mice treated with 20 mg/kg of FKB (LPS + FKB 10). FKB was dissolved in 0.5% sodium carboxymethyl cellulose (CMC-Na). All FKB treatments were carried out for 3 consecutive days prior to intratracheal LPS instillation. Mice in the vehicle control and LPS groups received the same volume of 0.5% CMC-Na during this period. Six hours after LPS challenge, mice were sacrificed with 0.2 mL sodium pentobarbital (100 mg/mL, i.p.). Serum, BALF, and lung tissue samples were collected and stored at −80 °C.
Serum was used for measurement of TNF-α and IL-6. BALF samples were collected from left lungs and used for cytokine and cell measurements. Unirrigated right lungs from the superior lobes were collected and weighed (wet weight). Lung tissues were then dried at 60 °C for more than 48 h and weighed again (dry weight). The ratio of wet: dry lung weight was calculated to assess edema. Portions of unirrigated lung sections were fixed in formalin and embedded in paraffin for histological analysis. The remaining unirrigated lung tissues were used for RNA isolation and protein lysate preparation.
Lung histopathology
Lung tissues were sectioned at 5-μm thickness. Sections were stained with hematoxylin and eosin to evaluate the degree of lung injury using light microscopy. The degree of injury was scored essentially as described previously [12] on the following variables: hemorrhage, edema, exudation, necrosis, congestion, neutrophil infiltration and atelectasis. The severity of injury was judged according to the following criteria: no injury = 0; injury to 25% of the field = 1; injury to 50% of the field = 2; injury to 75% of the field = 3 and diffuse injury = 4. Lung injury score was calculated as the sum of scores from 4 different views of the lung tissue section of each mouse (6 mice/group).
For immunohistochemical staining, dewaxed and rehydrated sections were subjected to heat-induced antigen retrieval in 0.01 mol/L citrate buffer (pH 6.0) for 3 min at 98 °C. Endogenous peroxidase activity was blocked with 3% hydrogen peroxide in methanol for 30 min at room temperature. Slides were then blocked with 5% BSA for 30 min. Primary antibodies against IL-6 or macrophage markers CD68 and F4/80 (1:200) were applied and slides were kept overnight at 4 °C. HRP-conjugated secondary antibody (1:200, 1 h) and DAB were used for detection. Immunoreactivity was measured by Image J software (NIH, Bethesda, MD).
For immunofluorescence staining, dewaxed and rehydrated sections were subjected to heat-induced antigen retrieval as described above. Slides were blocked in 5% BSA for 30 min. Primary antibody against NF-κB p65 (1:200) was applied and slides were incubated overnight at 4 °C. After washing the slides, TRITC-conjugated secondary antibody (1:500) was applied for 1 h at 37 °C. Slides were counterstained with DAPI. Images were obtained using an epi-fluorescence microscope (Nikon, Japan).
Bacterial infection
Bacterial infection was performed in mice as previously described [13, 14]. Briefly, Escherichia coli strain DH5α was grown in Luria Broth (LB) media and the density was determined at 600 nm (OD600) using NanoDrop2000. The corresponding colony-forming units (CFUs) were determined on LB agar plates. Mice were administered intragastrically FKB (10 or 20 mg/kg) or vehicle (10% DMSO in corn oil) once a day for 3 consecutive days. Viable E. coli DH5α (2 × 109 CFU/mouse) in 0.5 mL PBS was injected into the peritoneal cavity (i.p.). Survival of the mice was monitored every 6 h for 2 days.
Statistical analysis
All experiments were randomized and blinded. Data were expressed as Mean ± SEM. Statistical analysis was performed using GraphPad Prism 6.0 software (San Diego, CA). One-way ANOVA followed by Dunnett’s post hoc test was used when comparing more than two groups of data, and a one-way ANOVA, non-parametric Kruskal–Wallis test, followed by Dunn’s post hoc test when comparing multiple independent groups. P values < 0.05 were considered to be statistically significant. Post-tests were run only if F achieved P < 0.05 and there was no significant variance in homogeneity.
Results
Flavokawain B inhibits LPS-induced production of IL-6 and TNF-α in MPMs
We first evaluated 165 natural compounds for anti-inflammatory activity in LPS-treated MPMs. Potential cytotoxicity of the compounds was also determined in MPMs. As shown in Fig. 1a, a compound known as FKB exhibited significant anti-inflammatory effect in MPMs with low toxicity. Structurally, FKB is a naturally occurring chalcone compound (Fig. 1b). The effective dose of FKB in LPS-challenged MPMs was further evaluated. As shown in Fig. 1c, d, FKB pretreatment suppressed the production of IL-6 and TNF-α by LPS-challenged MPMs in a dose-dependent manner. Similarly, RT-qPCR showed that FKB pretreatment reduced LPS-induced mRNA levels of IL-6, TNF-α, IL-1β, and adhesion molecules VCAM-1 and ICAM-1 (Fig. 1e–i). These data demonstrate that FKB pretreatment reduces inflammatory responses in MPMs.
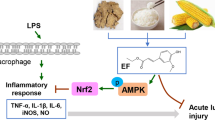
Flavokawain B exhibits anti-inflammatory effect by targeting MD2
In order to explore the mechanisms underlying the anti-inflammatory activity of FKB, a PCR array of 120 inflammation-related genes was utilized. As shown in Fig. 2a, FKB pretreatment altered the expression of 62 inflammation-related genes compared to LPS-challenged only group. LPS is known to induce inflammation by promoting the formation of MD2/TLR4 complex, leading to the activation of both TIR-domain-containing adapter-inducing interferon (TRIF) and myeloid differentiation factor 88 (MyD88) cascades (Fig. 2b). Based on our PCR array data, FKB pretreatment significantly inhibited both TRIF-dependent (i.e., type I interferons) and MyD88-dependent (i.e., interleukins and TNFs) inflammatory cytokines in LPS-challenged MPMs (Fig. 1a). These data suggest that upstream molecules such as MD2 and TLR4 may be targeted by FKB. To confirm this hypothesis, we evaluated the effect of FKB on MD2/TLR4 complex formation. Our data show that FKB pretreatment effectively inhibited LPS-induced TLR4/MD2 complex formation (Fig. 2c). Next, the physical interaction between FKB and MD2 or TLR4 was determined using SPR. The results show that FKB could directly bind to both MD2 and TLR4. However, the interaction between FKB and MD2 (KD value = 6.53 × 10−8) was much stronger than that of FKB-TLR4 (KD value = 2.10 × 10−4), suggesting that FKB mainly targets MD2 (Fig. 2d, e). This FKB-MD2 interaction was further confirmed by LPS displacement and Bis-ANS fluorescence displacement assays. Our data show that FKB reduced LPS-MD2 binding in a dose-dependent fashion (Fig. 2f, g). Finally, molecular docking was used to predict the potential binding site of FKB-MD2. Our data reveal that Arg90, Phe151, and Phe121 may be the important amino acid residues in FKB-MD2 interaction (Fig. 2h).
a mRNA levels of 62 inflammation-related genes in MPMs. b Schematic showing LPS-induced inflammatory response mechanisms. c The effect of FKB on MD2–TLR4 complex formation, as assessed by co-immunoprecipitation. d, e The binding affinity of FKB to rhMD2 and rhTLR4, as determined by the SPR assay. f Inhibitory effect of FKB in reducing LPS binding to MD2. g Binding of FKB to MD2 was detected by bis-ANS fluorescence displacement assay. h Molecular docking analysis of FKB binding to MD-2. Data presented as Mean ± SEM of three separate experiments, performed in duplicate; *P < 0.05 compared to LPS group.
Flavokawain B prevents LPS-induced MAPK phosphorylation and NF-κB activation in MPMs
LPS/MD2/TLR4 complex-induced inflammatory cytokine production involves the activation of MAPK and NF-κB pathways. Immunoblotting revealed that LPS significantly induced the phosphorylation of JNK, ERK, and P38, while FKB pretreatment reduced this activation in a dose-dependent manner (Fig. 3a). Furthermore, LPS-mediated IκB degradation and p65 phosphorylation were both inhibited in FKB-pretreated MPMs (Fig. 3b). In addition, FKB prevented P65 nuclear translocation in LPS-treated MPMs (Fig. 3c, d). Finally, RAW264.7 cells, stably expressing NF-κB-RE-EGFP reporter gene (RAW264.7-NF-κB-RE-EGFP), were used to confirm the effect of FKB on LPS-induced NF-κB activation. As shown in Fig. 3e, f, LPS increased nuclear EGFP fluorescence intensity indicating nuclear P65 translocation, while FKB pretreatment significantly reversed this effect in a dose-dependent manner. Taken together, these findings indicate that FKB inhibits the activation of MAPK and NF-κB pathways induced by LPS.
a Protein levels of p-JNK, JNK, p-p38, and p38 in LPS-challenged MPMs were examined by Western blotting. b NF-κB activation was determined by measuring the levels of IκBα and p-p65. GAPDH was used as the loading control. c p65-positive cells (Green) were determined using immunofluorescence. Cells were counterstained with DAPI (blue) (scale bar = 100 μm). d Quantification of nucleocyte count (nuclear signal) for c. e RAW264.7 cells stably expressing NF-κB-RE-EGFP reporter (RAW264.7-NFκB-RE-EGFP) were pretreated with FKB and then exposed to LPS. EGFP signal was detected by fluorescence microscopy (scale bar = 100 μm). f Average fluorescence intensity of EGFP expressing cells shown in e. Data were presented as Mean ± SEM of three separate experiments, performed in duplicate; *P < 0.05 compared to LPS group.
Flavokawain B treatment prevents LPS-induced acute lung injury in mice
We next used the well-established LPS-induced mouse model of ALI to evaluate the therapeutic effect of FKB. Histological analysis shows that LPS triggered inflammatory cell infiltration, thickened the alveolar walls, and destroyed the normal lung tissue structure (Fig. 4a). Further evidence of LPS-induced lung structural defects is illustrated by the lung injury score (Fig. 4b), the dry-to-wet lung weight ratio (Fig. 4c), and the total protein concentration in BALF (Fig. 4d). Mice treated with FKB prior to LPS challenge showed significantly reduced injuries (Fig. 4a–d).
a Representative histological images of lung tissues showing H&E-stained sections (scale bar = 50 μm). b Lung injury score as assessed by histological analysis of lung tissues. Panels showing lung wet/dry ratio (c), amount of protein in BALF (d), numbers of total cells (e) and neutrophils (f) in BALF, and MPO activity in lung tissues (g). Data were presented as Mean ± SEM of three separate experiments, performed in duplicate; *P < 0.05 compared to LPS group.
In ALI, a large number of inflammatory cells leak out into the lung interstitium and alveoli due to damaged air-blood barrier and increased alveolar-capillary permeability. Therefore, changes in the cellular composition of BALF can be used as an indicator of ALI. As shown in Fig. 4e, f, total cells and neutrophil counts were significantly increased in the BALF of LPS-challenged mice. In addition, MPO (a heme protein rich in neutrophils) activity was increased in lung lysates of LPS mice (Fig. 4g). In contrast, mice treated with FKB showed lower total cells and neutrophil counts in the BALF, and reduced MPO activity in the lungs (Fig. 4e–g). These findings confirm the protective role of FKB against LPS-induced ALI and support the anti-inflammatory responses seen in our in vitro study.
Flavokawain B inhibits MD2–TLR4 complex formation and inflammatory responses in lungs of ALI mice
Next, we used co-immunoprecipitation to determine whether FKB treatment of mice altered LPS-induced MD2/TLR4 complex formation. Consistent with our in vitro results, FKB treatment significantly inhibited LPS-induced MD2-TLR4 complex formation in the lung tissues of mice (Fig. 5a, b). In addition, immunofluorescence staining of tissues indicated that LPS-induced p65 nuclear translocation in the lung tissues of mice was inhibited upon FKB treatment (Fig. 5c, d). In the early stages of ALI, pro-inflammatory IL-6 and TNF-α play a key role in driving lung inflammation. As shown in Fig. 5e–h, LPS caused significantly increased levels of IL-6 and TNF-α in both BALF and serum. However, these increases were not seen in mice treated with FKB (Fig. 5e–h). We also show that FKB treatment reduced immunoreactivity to IL-6 in the lung tissues of mice (Fig. 5I, j). This anti-inflammatory effect of FKB was confirmed by measuring mRNA levels of IL-6, TNF-α, and IL-1β (Fig. 5k–m).
a Formation of MD2/TLR4 complex in lung tissues of mice was detected by co-immunoprecipitation. b Densitometric quantification of MD2/TLR4 complex levels. Representative blots are shown in a. c Immunofluorescence staining of lung tissues for p65 (scale bar = 50 μm). Representative images are shown from each group (n = 5 per group). d Quantification of p65-positive nuclei in lung tissues. Representative stained images are shown in c. p65-positive cells were calculated as ratio of p65-positive nuclei per total nuclei. Quantitative data were normalized to LPS group. Inflammatory cytokines in BALF and serum samples of mice. Panels showing IL-6 (e) and TNF-α (f) in BALF, and IL-6 (g) and TNF-α (h) in serum. i Immunohistochemical staining of lung tissues for IL-6 (scale bar = 50 μm). All images are representative of five mice per group. IOD integral optical density). j Quantification of IL-6 immunoreactivity. Data were shown as ratio of positive staining area to total area. mRNA levels of inflammatory cytokines IL-6 (k), TNF-α (l), and IL-1β (m) in lung tissues of mice. Transcript levels were normalized to β-actin. Data were presented as Mean ± SEM of three separate experiments, performed in duplicate; *P < 0.05 compared to LPS group.
Immunohistochemical staining were used to assess macrophage infiltration in lung tissues. For this, we stained the sections for CD68 and F4/80. As shown in Fig. 6a–d, a significant increase in macrophage infiltration was observed in LPS-treated mice. FKB treatment, however, reduced LPS-induced macrophage infiltration. Additionally, our data show increased levels of ICAM-1 and VCAM-1 in the lungs of LPS-treated mice but not in mice treated with FKB (Fig. 6e, f). In summary, our in vivo data prove that FKB prevents LPS-induced MD2/TLR4 complex formation, and subsequently reduces inflammatory responses and injuries in the lungs of mice.
Immunohistochemical staining for macrophage markers F4/80 (a) and CD68 (b) in lung tissues (scale bar = 50 μm). Quantification of F4/80 (c) and CD68 (d) immunoreactivity. Data were shown as ratio of positive staining area to total area. mRNA levels of adhesion molecules ICAM-1 (e) and VCAM-1 (f) in lung tissues of mice. Transcript levels were normalized to β-actin. Data were presented as Mean ± SEM of three separate experiments, performed in duplicate; *P < 0.05 compared to LPS group.
Flavokawain B promotes survival in sepsis mice model
Live E. coli DH5α infection produces a series of events in the lungs that are similar to LPS challenge. Thus, we finally evaluated the effect of FKB on mouse mortality upon bacterial infection. As shown in Fig. 7, all mice in the E. coli DH5α group died within 48 h after infection. However, this mortality was markedly reduced in mice treated with FKB such that both 10 and 20 mg/kg doses of FKB produced greater than 50% and 70% survival following infection, respectively (Fig. 7).
C57BL/6 mice were treated with FKB (10 and 20 mg/kg; i.g.) or vehicle (10% DMSO and 90% Corn oil) twice in 1 day prior to infection with viable E. coli DH5α (2 × 109 CFU/mouse; i.p.). Mouse survival was monitored every 6 h for 2 days. Kaplan–Meier survival curves were used to analyze the data (10 mice per group). The significance was evaluated by the log rank (Mantel–Cox) test. *P < 0.05 compared to the DH5α-challenged group.
Discussion
The overall aim of this study was to identify potential anti-inflammatory natural products using a high throughput screening platform, and to explore the underlying mechanisms in established culture and a clinically relevant animal model. To achieve this aim, we tested 165 natural compounds and identified FKB. FKB showed a strong anti-inflammatory effect in LPS-challenged MPMs with no significant toxicity (Fig. 1a). The two key findings of our study are as follows: (1) studies of cell surface binding and cell-free protein-protein interactions indicate that FKB directly binds to MD2 to inhibit TLR4/MD2 complex formation and TLR4 activation. This direct targeting manifested as reduced NF-κB and MAPK activation and suppression of pro-inflammatory cytokine production, both in vitro and in vivo. (2) FKB treatment of mice prevented the production of pro-inflammatory molecules, reduced lung injury in mice challenged with LPS, and prolonged survival of mice infected with E. coli DH5α. To the best of our knowledge, this is the first study to demonstrate that MD2 is a direct target of FKB, and that FKB may be a potential therapeutic candidate for ALI.
Kava extracts can be classified into chalcone and kavalactone. Chalcones are an important group of natural compounds and serve as precursors of flavonoid and isoflavonoids. Chalcones have gained attention due to the many reported beneficial properties such as, redox balancing [15], preventing tumor growth and progression [16], reducing inflammatory responses [17], preventing microbial infections [18], reducing obesity and associated dysfunction [19], and correcting diabetes [20]. Flavokawain A, B, and C (FKA, FKB, and FKC) are the three different types of naturally occurring chalcones in Kava extracts [21]. In particular, FKB has shown promising activities in cancers through the induction of reactive oxygen species-mediated or endoplasmic reticulum stress-mediated cell apoptosis [7, 8, 22, 23]. In addition, FKB was reported to exhibit anti-inflammatory property, mainly through its ability to inhibit NF-κB [9]. However, how FKB modulates NF-κB pathway is still unknown.
We utilized an inflammatory cytokine and receptor PCR array to identify the mechanisms by which FKB mediates anti-inflammatory activities. As shown in Fig. 2a, b, FKB pretreatment of MPMs regulated the expression of 62 inflammation-related genes. Most, if not all, genes may be regulated by LPS/MD2/TLR4 signaling pathway, suggesting that FKB might target and inhibit LPS/MD2/TLR4 axis. Previously studies have shown that various chalcones and chalcone derivatives including Xanthohumol [24], L6H21 [25], L2H17 [26], and L6H9 [27] interact with MD2. Based on these studies, we hypothesized that FKB may also target MD2. To test our hypothesis, we investigated MD2 as a target of FKB using co-immunoprecipitation, SPR, displacement assays, and computer molecular docking (Fig. 2c–h). Our data show that FKB physically binds to both MD2 and TLR4, with a much higher affinity for MD2 (6.53 × 10−8 M) compared to TLR4 (2.10 × 10−4 M). The binding of FKB to MD2 inhibited the formation of LPS/MD2/TLR4 complex (Fig. 2c), and prevented the subsequent activation of MAPK and NF-κB pathways and inflammatory cytokine expression in mice. The direct binding between FKB and MD2 is a new observation in this field. In addition, our study is also the first documented mechanism by which FKB may modulate NF-κB pathway.
It is now well established that TLR4, along with its co-receptor MD2, mediates LPS-induced lung injury [28, 29]. MD2 is a central and necessary protein in TLR4-mediated host responses to pathogens. For example, MD2−/− mice show remarkable increase in survival rate following an endotoxic shock [30]. Administration of LPS from Neisseria meningitides in MD2−/− mice also resulted in markedly lower neutrophil counts in BALF [31]. Clinically, soluble MD2 in the plasma of patients with severe sepsis can promote LPS-induced inflammatory responses through TLR4-expressing epithelial cells of lungs [32]. Compounds that target MD2, unsurprisingly, show therapeutic benefit in ALI [33,34,35,36]. Furthermore, MD2 is reported to facilitate both innate and allergic airway inflammation [37]. These studies suggest that targeting MD2 to block the binding of LPS to TLR4 may be effective in treating ALI and other inflammatory lung diseases. Confirming the hypothesis, our data show that blockage of MD2 by FKB protected against LPS-induced lung injury, reduced systemic and local inflammatory cytokine production and macrophage infiltration in lungs, and prolonged the survival of infected mice. Since both monocyte-derived macrophages and alveolar macrophages have been shown to play important roles in the development of ALI [38], further studies are needed to confirm the activity of FKB in these macrophage populations in the LPS-challenged mice.
Conclusion
In conclusion, this study shows that FKB, a natural chalcone compound, can effectively inhibit pro-inflammatory responses induced by LPS both in vitro and in vivo. This anti-inflammatory activity is mediated by the direct interaction between MD2 and FKB and inhibition of downstream MyD88 and/or TRIF-mediated activation of NF-κB and MAPK. Therefore, FKB is a potential compound for future drug development for the ALI therapy.
References
Mowery NT, Terzian WTH, Nelson AC. Acute lung injury. Curr Probl Surg. 2020;57:100777.
Standiford TJ, Ward PA. Therapeutic targeting of acute lung injury and acute respiratory distress syndrome. Transl Res. 2016;167:183–91.
Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Prim. 2019;5:18.
Chen H, Bai C, Wang X. The value of the lipopolysaccharide-induced acute lung injury model in respiratory medicine. Expert Rev Respir Med. 2010;4:773–83.
Park BS, Lee JO. Recognition of lipopolysaccharide pattern by TLR4 complexes. Exp Mol Med. 2013;45:e66.
Hseu YC, Chiang YC, Vudhya Gowrisankar Y, Lin KY, Huang ST, Shrestha S, et al. The in vitro and in vivo anticancer properties of chalcone flavokawain B through induction of ROS-mediated apoptotic and autophagic cell death in human melanoma cells. Cancers 2020;12:2936.
Hseu YC, Lin RW, Shen YC, Lin KY, Liao JW, Thiyagarajan V, et al. Flavokawain B and doxorubicin work synergistically to impede the propagation of gastric cancer cells via ROS-mediated apoptosis and autophagy pathways. Cancers. 2020;12:2475.
Wang J, Qi Q, Zhou W, Feng Z, Huang B, Chen A, et al. Inhibition of glioma growth by flavokawain B is mediated through endoplasmic reticulum stress induced autophagy. Autophagy. 2018;14:2007–22.
Lin CT, Senthil Kumar KJ, Tseng YH, Wang ZJ, Pan MY, Xiao JH, et al. Anti-inflammatory activity of flavokawain B from Alpinia pricei Hayata. J Agric Food Chem. 2009;57:6060–5.
Wang Y, Luo W, Han J, Khan ZA, Fang Q, Jin Y, et al. MD2 activation by direct AGE interaction drives inflammatory diabetic cardiomyopathy. Nat Commun. 2020;11:2148.
Chen L, Chen H, Chen P, Zhang W, Wu C, Sun C, et al. Development of 2-amino-4-phenylthiazole analogues to disrupt myeloid differentiation factor 88 and prevent inflammatory responses in acute lung injury. Eur J Med Chem. 2019;161:22–38.
Su X, Wang L, Song Y, Bai C. Inhibition of inflammatory responses by ambroxol, a mucolytic agent, in a murine model of acute lung injury induced by lipopolysaccharide. Intensive Care Med. 2004;30:133–40.
Wegiel B, Larsen R, Gallo D, Chin BY, Harris C, Mannam P, et al. Macrophages sense and kill bacteria through carbon monoxide-dependent inflammasome activation. J Clin Invest. 2014;124:4926–40.
Pan H, Xu LH, Huang MY, Zha QB, Zhao GX, Hou XF, et al. Piperine metabolically regulates peritoneal resident macrophages to potentiate their functions against bacterial infection. Oncotarget. 2015;6:32468–83.
Adelusi TI, Akinbolaji GR, Yin X, Ayinde KS, Olaoba OT. Neurotrophic, anti-neuroinflammatory, and redox balance mechanisms of chalcones. Eur J Pharmacol. 2021;891:173695.
Kode J, Kovvuri J, Nagaraju B, Jadhav S, Barkume M, Sen S, et al. Synthesis, biological evaluation, and molecular docking analysis of phenstatin based indole linked chalcones as anticancer agents and tubulin polymerization inhibitors. Bioorg Chem. 2020;105:104447.
Zhang C, Yue H, Sun P, Hua L, Liang S, Ou Y, et al. Discovery of chalcone analogues as novel NLRP3 inflammasome inhibitors with potent anti-inflammation activities. Eur J Med Chem. 2021;219:113417.
Elkhalifa D, Al-Hashimi I, Al Moustafa AE, Khalil A. A comprehensive review on the antiviral activities of chalcones. J Drug Target. 2021;29:403–19.
Karimi-Sales E, Mohaddes G, Alipour MR. Chalcones as putative hepatoprotective agents: Preclinical evidence and molecular mechanisms. Pharmacol Res. 2018;129:177–87.
Rocha S, Ribeiro D, Fernandes E, Freitas M. A systematic review on anti-diabetic properties of chalcones. Curr Med Chem. 2020;27:2257–321.
Lebot V, Do TK, Legendre L. Detection of flavokavins (A, B, C) in cultivars of kava (Piper methysticum) using high performance thin layer chromatography (HPTLC). Food Chem. 2014;151:554–60.
Hseu YC, Huang YC, Thiyagarajan V, Mathew DC, Lin KY, Chen SC, et al. Anticancer activities of chalcone flavokawain B from Alpinia pricei Hayata in human lung adenocarcinoma (A549) cells via induction of reactive oxygen species-mediated apoptotic and autophagic cell death. J Cell Physiol. 2019;234:17514–26.
Chang CT, Hseu YC, Thiyagarajan V, Lin KY, Way TD, Korivi M, et al. Chalcone flavokawain B induces autophagic-cell death via reactive oxygen species-mediated signaling pathways in human gastric carcinoma and suppresses tumor growth in nude mice. Arch Toxicol. 2017;91:3341–64.
Peluso MR, Miranda CL, Hobbs DJ, Proteau RR, Stevens JF. Xanthohumol and related prenylated flavonoids inhibit inflammatory cytokine production in LPS-activated THP-1 monocytes: structure-activity relationships and in silico binding to myeloid differentiation protein-2 (MD-2). Planta Med. 2010;76:1536–43.
Wang Y, Shan X, Chen G, Jiang L, Wang Z, Fang Q, et al. MD-2 as the target of a novel small molecule, L6H21, in the attenuation of LPS-induced inflammatory response and sepsis. Br J Pharmacol. 2015;172:4391–405.
Chen H, Yan T, Song Z, Ying S, Wu B, Ju X, et al. MD2 blockade prevents modified LDL-induced retinal injury in diabetes by suppressing NADPH oxidase-4 interaction with Toll-like receptor-4. Exp Mol Med. 2021;53:681–94.
Wang Y, Fang Q, Jin Y, Liu Z, Zou C, Yu W, et al. Blockade of myeloid differentiation 2 attenuates diabetic nephropathy by reducing activation of the renin-angiotensin system in mouse kidneys. Br J Pharmacol. 2019;176:2642–57.
Liu Z, Chen L, Yu P, Zhang Y, Fang B, Wu C, et al. Discovery of 3-(Indol-5-yl)-indazole derivatives as novel myeloid differentiation protein 2/toll-like receptor 4 antagonists for treatment of acute lung injury. J Med Chem. 2019;62:5453–69.
Ouyang W, Zhou H, Liu C, Wang S, Han Y, Xia J, et al. 25-Hydroxycholesterol protects against acute lung injury via targeting MD-2. J Cell Mol Med. 2018;22:5494–503.
Nagai Y, Akashi S, Nagafuku M, Ogata M, Iwakura Y, Akira S, et al. Essential role of MD-2 in LPS responsiveness and TLR4 distribution. Nat Immunol. 2002;3:667–72.
Hadina S, Weiss JP, McCray PB Jr, Kulhankova K, Thorne PS. MD-2-dependent pulmonary immune responses to inhaled lipooligosaccharides: effect of acylation state. Am J Respir Cell Mol Biol. 2008;38:647–54.
Pugin J, Stern-Voeffray S, Daubeuf B, Matthay MA, Elson G, Dunn-Siegrist I. Soluble MD-2 activity in plasma from patients with severe sepsis and septic shock. Blood. 2004;104:4071–9.
Yang Y, Han C, Sheng Y, Wang J, Zhou X, Li W, et al. The mechanism of aureusidin in suppressing inflammatory response in acute liver injury by regulating MD2. Front Pharmacol. 2020;11:570776.
Wu P, Yan H, Qi J, Jia W, Zhang W, Yao D, et al. L6H9 attenuates LPS-induced acute lung injury in rats through targeting MD2. Drug Dev Res. 2020;81:85–92.
Chen H, Zhang Y, Zhang W, Liu H, Sun C, Zhang B, et al. Inhibition of myeloid differentiation factor 2 by baicalein protects against acute lung injury. Phytomedicine. 2019;63:152997.
Zhang Y, Xu T, Pan Z, Ge X, Sun C, Lu C, et al. Shikonin inhibits myeloid differentiation protein 2 to prevent LPS-induced acute lung injury. Br J Pharmacol. 2018;175:840–54.
Hosoki K, Boldogh I, Aguilera-Aguirre L, Sun Q, Itazawa T, Hazra T, et al. Myeloid differentiation protein 2 facilitates pollen- and cat dander-induced innate and allergic airway inflammation. J Allergy Clin Immunol. 2016;137:1506–13.
Cheng P, Li S, Chen H. Macrophages in lung injury, repair, and fibrosis. Cells. 2021;10:436.
Acknowledgements
Financial support was provided by the National Natural Science Foundation of China (81970338 to YW, 82070833 to CZ, and 82000793 to WL), Natural Science Foundation of Zhejiang Province (LR18H160003 to YW), and Zhejiang Provincial Key Research and Development Program (2021C03070 to CZ).
Author information
Authors and Affiliations
Contributions
WL, LBY, CCQ, BM, GMM, XMM, JW, CHH, BJ, and LXZ: collection, analysis, and interpretation of data; YW, CZ, and GL: conception and design, interpretation of data, manuscript writing, and manuscript revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Luo, W., Yang, Lb., Qian, Cc. et al. Flavokawain B alleviates LPS-induced acute lung injury via targeting myeloid differentiation factor 2. Acta Pharmacol Sin 43, 1758–1768 (2022). https://doi.org/10.1038/s41401-021-00792-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-021-00792-4
Keywords
This article is cited by
-
Bisdemethoxycurcumin alleviates LPS-induced acute lung injury via activating AMPKα pathway
BMC Pharmacology and Toxicology (2023)