Abstract
For follicular lymphoma (FL) with grade 1/2, the complete response (CR) rate of the first-line R-CHOP treatment was significantly low. In this study, we assessed the rationality of the administration of rituximab for FL patients with grade 1/2 based on concentration–response relationship analyses. Thus, we conducted a prospective pharmacokinetic (PK) study in 68 FL patients with grades 1–3 treated with R-CHOP at 21-day intervals. Plasma rituximab concentrations were quantified using ELISA and the population PK modeling was established with Phoenix® NLMETM. The first cycle trough concentration (C1-trough) of rituximab was a significant independent risk factor for achieving CR in matched-pair logistic regression analysis, rather than the concentrations in later cycles; the recommendatory minimum optimal C1-trough was 13.60 μg/mL. Patients with grade 1/2 had significantly lower C1-trough compared with grade 3 (12.21 μg/mL vs. 23.45 μg/mL, P < 0.001), only 30% patients with grade 1/2 could reach 13.60 μg/mL, compared with 91.67% in patients with grade 3, which was in accord with its unsatisfactory CR rates (43.33% vs. 76.32%). The stage indicating the tumor burden (the target) was a crucial influence factor for C1-trough, accounting for 40.70% of its variability, 70% patients with grade 1/2 were stage IV in this study, since the systemic therapy only started at the disseminated disease stage. The initial dose of 1800 mg was recommended by Monte Carlo simulation for patients with grade 1/2. In summary, low C1-trough accounted for low-grade FL’s unsatisfactory CR rate, designing the first dosage of rituximab should be a very important component of individualized therapy for FL.
Similar content being viewed by others
Introduction
Follicular lymphoma (FL) is one of the most common subtypes of non-Hodgkin lymphoma [1]; histopathologically, FL is stratified into grades 1–3 according to the proportion of centroblasts. Low-grade FL (grade 1/2), which includes cases with few centroblasts, is characterized by slow disease progression and a relatively good prognosis, but it is usually incurable [2, 3]. Grade 3b FL is composed entirely of centroblasts and is more closely related to diffuse large B-cell lymphoma at the molecular level [4,5,6]. In addition, according to the National Comprehensive Cancer Network (NCCN) Guideline, staging for FL was determined by Lugano modification of Ann Arbor Staging System, which refers to the severity and extent of the spread of the disease. For patients with grade 1/2 disease, the asymptomatic stage is best managed with watchful waiting, and only patients who present with a disseminated disease (i.e., advanced stage) require systemic therapy. Guidelines from the NCCN recommend that in patients with either advanced low-grade or grade 3 FL, rituximab plus chemotherapy, most often CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) repeated every 2 or 3 weeks, is the first-line standard treatment. However, the response to the first-line R-CHOP regimen varied greatly for different grades of FL. Based on clinical trials, the complete response (CR) rates ranged from 25% to 30% for patients with grade 1/2 FL [7, 8] but could reach as high as 54%–86% for grade 3 [9, 10].
Rituximab (MabThera®, Rituxan®) is a chimeric human–mouse anti-CD20 monoclonal antibody that dramatically improves the survival of patients with non-Hodgkin’s lymphomas [11]. For patients with FL, rituximab was initially administered as a single agent at a weekly dose of 375 mg/m2, and a large amount of pharmacokinetic (PK) data [12] from 166 recurrent or refractory low-grade non-Hodgkin’s lymphoma patients suggested that at 3 months post treatment, median serum levels in 62 responders were 25.40 μg/mL compared with 5.90 μg/mL in 42 nonresponders, and then 25.40 μg/mL is recommended as the minimum effective concentration for the next 2 years of maintenance therapy. In a prospective phase II trial (AGMT-NHL9), 17 patients with previously untreated FL received R-FC repeated every 28 days, and the trough concentration of rituximab was also significantly correlated with remission quality (complete vs. partial remission; P = 0.005) [13]. All these studies suggested a positive exposure–response relationship for rituximab, but PK data are limited in FL patients who received R-CHOP at 21-day intervals, and the optimal concentration of rituximab in induction therapy still needs to be identified.
Several studies [11, 14, 15] have suggested that tumor burden affects the interindividual PK variability of rituximab—those with greater tumor burdens have lower levels of exposure to rituximab. In Tout et al.’s study [14], for patients with diffuse large B-cell lymphoma, rituximab exposure decreased as metabolic tumor volume increased, and a high area under the curve (AUC) in cycle 1 (≥9400 mg·h·L−1) was associated with a better response. The authors also indicated that the 375 mg/m2 classical dose was suitable for patients with baseline tumor volume < 281 cm3. We hypothesized that when systemic therapy begins for FL patients with low-grade FL, the disease is usually at an advanced stage, and the prevalent high level of tumor burden may lead to insufficient drug concentration, which may account for the lower CR rate in patients with low-grade FL than that in patients with grade 3 FL.
This study was initiated to assess the rationale of the administration of rituximab for FL patients with grade 1/2 FL based on concentration–response relationship analyses. We aimed to provide an optimal dosage regimen of this anti-CD20 antibody for patients with FL.
Materials and methods
Patients and therapy
Patients older than 18 years with newly diagnosed FL were eligible to participate. Patients received rituximab at a dose of 375 mg/m2 on day 1 of each 3-week cycle in combination with CHOP chemotherapy, according to the national guidelines for the treatment of non-Hodgkin lymphoma. The chemotherapy schedules for CHOP are as follows: day 1: cyclophosphamide 750 mg/m2 IV, doxorubicin 50 mg/m2 IV, and vincristine 1.4 mg/m2 IV (maximum 2 mg) and days 1–5: prednisone 100 mg po. Whole-body PET/CT scans are recommended for diagnostic and treatment workups. Clinical response was evaluated according to the revised response criteria for malignant lymphoma proposed by the International Harmonization Project [16]. CR indicated complete resolution of all measurable and nonmeasurable diseases, including normalization of previously abnormal bone marrow biopsies. Bilateral bone marrow aspirations and biopsies were performed at initial work-up and upon confirmation of response. The treatment responses were evaluated after the second, fourth, and sixth courses.
The study was conducted in accordance with Good Clinical Practice guidelines and the principles of the Declaration of Helsinki. Ethical approval for this study was obtained from the ethics committee of the Sun Yat-Sen University Cancer Center (No. GZR2018–077), and informed consent was obtained from all subjects before participation. This study is registered with the Chinese Clinical Trial Registry, number ChiCTR1800017001 (http://www.chictr.org.cn/index.aspx).
Determination of rituximab concentration
Two samples per cycle were obtained, samples for peak concentration were collected in the time frame from 15 min up to 3 h after rituximab infusion, and samples for trough concentration were collected immediately before rituximab infusion in the next cycle. Plasma concentrations of rituximab were determined by the Matriks Biotek rituximab (SHIKARI® Q-RITUX) solid phase enzyme-linked immunosorbent assay. The lowest detectable level that can be specifically distinguished from the zero standard was 30 ng/mL.
The proportions of CD19+ B cells in peripheral blood were assessed as a surrogate marker for CD20+ B cells, since their expression mirrors CD20 expression. Blood samples for CD19+ B-cell counts were collected before the first treatment infusion. Blood samples were analyzed using a flow cytometry procedure.
Population PK (PPK) model building
PPK analysis was performed using Phoenix NLME (version 1.3; Certara L.P., St. Louis, MO, USA) Phoenix® WinNonlin 6.4. The individual PK parameters were simulated using a Bayesian approach with the PPK model [17,18,19]. The basic PK parameters used in this study were volume of distribution for the central compartment (V, L), clearance of the central compartment (CL, mL/h) for the one-compartment model or for the two-compartment model with additional parameters defined as volume of distribution for the peripheral compartment (V2, L), and intercompartmental clearance (CL2, mL/h). The criterion for the estimation of statistical significance was a reduction or increase in the value of the objective function (OFV; −2log likelihood). Goodness of fit was evaluated by using diagnostic scatter plots and two complementary methods: a nonparametric bootstrap [20] and a visual predictive check (VPC) [19].
Statistical analysis
Statistical analyses were performed using SPSS 22.0 (IBM, Armonk, NY, USA) and Stata 15.0 (StataCorp LP, College Station, TX, USA), and the significance level was set at P < 0.05. Comparisons between groups were analyzed using T tests and χ2 tests. The influence of a single rituximab concentration on the treatment response was evaluated using conditional logistic regression, which has the same philosophy as logistic regression, with the exception that the estimates are conditional in the matched groups [21]. The minimum optimal concentration was assessed by receiver operating characteristic (ROC) analysis and validated using bootstrap analysis (1000 replicates).
Results
Patient characteristics
A total of 68 FL patients were included in this study, and patient characteristics at baseline are shown in Table 1. According to the regimen, each patient was administered 375 mg/m2 rituximab, and the median dose of rituximab for the patients was 700 mg (range from 500 to 800 mg) per cycle. Dose reductions for adverse reactions were most common for cyclophosphamide (22.06% of patients) and doxorubicin (17.65% of patients) in the R-CHOP treatment. The most common reason for dose reductions was neutropenia. Mean relative dose intensities for individual drugs were relatively close for patients with grade 1/2, grade 3a, and grade 3b FL. The CR rates after the second, fourth, and sixth cycles were 38.24%, 55.88%, and 61.76%, respectively (Table 1).
Rituximab concentrations correlated with response
The plasma concentrations of rituximab quantified before infusions (Ctrough) in each cycle are reported in Table 2. Large individual variability existed at each time point and could reach more than 30-fold. The treatment responses were evaluated after 2, 4, and 6 cycles. For CR patients in each evaluation cycle, their Ctrough in the first cycle (C1-trough) was significantly higher than that in the non-CR patients (response after cycle 2: 24.61 μg/mL vs. 14.69 μg/mL; cycle 4: 23.81 μg/mL vs. 11.74 μg/mL; cycle 6: 23.13 μg/mL vs. 10.98 μg/mL, all P < 0.001), and the Ctrough in 2–3 cycles was marginally higher in CR patients than in non-CR patients but was not different in the subsequent cycles. No difference in peak concentration between the CR and non-CR groups was observed in any cycles.
Matched-pair logistic analysis for concentration and response
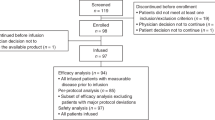
Tumor stage and grade are known risk factors for treatment response, and conditional logistic regression (matched-pair) analyses were used to determine the relative risk of C1-trough rituximab for response. The dataset was stratified into four subsets: low-grade (grade 1/2) patients with stage I/II/III, low-grade patients with stage IV, 3 grade patients with stage I/II/III, and 3 grade patients with stage IV. The C1-trough was significantly associated with achieving CR for both response evaluations after cycle 4 (odds ratio, 0.93; 95% CI, 0.87–0.99; P = 0.027) and after cycle 6 (odds ratio, 0.91; 95% CI, 0.85–0.98; P = 0.012) for this dataset. The distributions of the C1-trough in the matched-pair groups for CR vs. non-CR patients are shown in Fig. 1.
In the matched-pair logistic analysis, the matching variables included stage (stage I–III and stage IV) and grade (grade 1/2 and grade 3), so the dataset was stratified into four subsets: low-grade patients with stage I–III FL, low-grade patients with stage IV FL, 3 grade patients with stage I–III FL, and 3 grade patients with stage IV FL. The rituximab trough concentration in the first cycle was significantly associated with achieving CR for this dataset (odds ratio, 0.91; 95% CI, 0.85–0.98; P = 0.012).
The optimal rituximab concentration
ROC analysis was performed to determine the minimum optimal rituximab trough concentrations. For cycle 1, the highest cut-off value of 13.60 μg/mL was recommended with sensitivity and specificity of 90.50% and 80.80%, respectively, and the area under the ROC curves was 0.88 (95% CI, 0.79–0.97, P < 0.001). The highest cut-off values of C1-trough were also calculated for patients with grade 1/2 and grade 3 FL. For FL patients with grade 1/2 FL, the highest cut-off value was also 13.60 μg/mL (sensitivity, 69.20%; specificity, 100%; AUC, 0.85; P = 0.001). Therefore, 13.60 μg/mL was recommended as the minimum optimal concentration. For trough concentration in cycle 2, the areas under the ROC curves were unsatisfactory at 0.56 (P = 0.380).
The threshold value of 13.60 μg/mL was also significantly associated with achieving CR after cycle 6 in matched-pair logistic regression analysis (odds ratio, 0.14; 95% CI, 0.04–0.50; P = 0.002), indicating that if the drug levels exceed 13.60 μg/mL, the risk of treatment failure would be reduced by 86%.
In this study, the percentage of patients with concentrations above 13.60 μg/mL was 63.24%, and the CR rates after the second, fourth, and sixth cycles for those patients were 58.14%, 81.40% and 88.37%, respectively. The percentages of patients with concentrations below 13.60 μg/mL was 36.76%, and the CR rates after the second, fourth, and sixth cycles for those patients were 4.00%, 12.00% and 16.00%, respectively.
Influencing factors of rituximab C 1-trough
The correlations between C1-trough and sex, age, BSA, BMI, stage, initial bone marrow infiltration, beta 2-microglobulin, lactate dehydrogenase, baseline circulating CD19+ cell proportion, and hemoglobin were analyzed by linear regression. Only tumor stage was significantly associated with C1-trough in multiple linear regressions: C1-trough = 13.07 + 14.20 (Stage I/II) + 9.12 (Stage III), and the adjusted R2 was 40.70% (F = 22.30, P < 0.001).
The percentages of patients with concentrations below 13.60 μg/mL in stages I/II, III, and IV were 0%, 17.65% and 61.11%, respectively.
FL grades and rituximab concentration
For FL patients with grade 3a and grade 3b FL, the peak and trough concentrations in each cycle were similar.
For patients with grade 1/2 FL, the trough concentrations in cycle 1 were significantly lower than those in patients with grade 3 FL (12.21 μg/mL vs. 23.45 μg/mL, P < 0.001) (Table 2) but were not different in the subsequent cycles. In the first cycle, only 30% of patients with low-grade FL could reach the cut-off value of C1-trough (13.60 μg/mL), compared with 91.67% in patients with grade 3 FL.
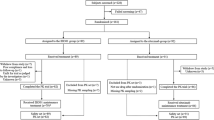
The influence of stage on the C1-trough in patients with different grades was further analyzed, and the proportions of stage IV patients with grade 1/2, grade 3a and grade 3b FL were 70%, 37.50% and 42.86%, respectively. For all stage IV patients, the C1-trough in patients with low-grade disease was significantly lower than that in patients with grade 3 disease (8.91 μg/mL vs. 18.91 μg/mL, P < 0.001) (Fig. 2).
The recommended dosage calculated by Monte Carlo simulation
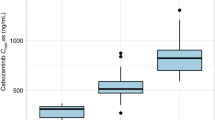
Preliminary analysis for the base PPK model showed that the OFVs for exploration of the one- and two-compartment models were 4702.58 and 4556.29, respectively. The two-compartment model resulted in a better fit for describing rituximab concentrations, while an additive + multiplicative error model best described the residual variability. The tumor stage was associated with V2, and inclusion of stage in the final model was associated with a decrease in OFV to 4532.38. The VPC of the final model demonstrated that the DV concentration data were approximately distributed within the 5th–95th prediction interval. The parameters of the final model and 1000 bootstrap replicates are listed in Table 3.
Different initial dosages of rituximab were simulated using this PPK model with 1000 replications. For patients with grade 1/2 FL, the percentages of patients with concentrations greater than 13.60 μg/mL were 46.67%, 56.67%, 66.67%, 80%, 90%, and 96.67% for 900, 1000, 1200, 1500, 1800, and 2000 mg, respectively.
Discussion
To our knowledge, this is the first prospective observational study that explored the PK characteristics of rituximab in FL with different grades. The significantly low initial concentrations in patients with low-grade FL could partly account for its unsatisfactory CR rate. Moreover, we found that higher rituximab concentrations in the first cycle rather than in the subsequent cycles were significantly associated with achieving CR, suggesting the importance of giving the sufficient rituximab dose at the beginning of the treatment, and the minimum optimal concentration values 13.60 μg/mL and initial dose of 1800 mg (for grade 1/2) were recommended. Herein, increasing the initial dose of rituximab should be a very important component of individualized therapy.
Several studies have suggested that the trough concentration of rituximab was a good predictor of response. For example, Tobinai et al. [22] detected higher mean values of trough levels and AUC of rituximab in responders with aggressive B-cell lymphoma. Accordingly, Li et al. [23] found higher median trough levels of rituximab and AUC in chronic lymphocytic leukemia responders. In line with these findings, our study reported that the trough concentrations in patients with CR were significantly higher than those in non-CR patients in the first cycle (23.13 μg/mL vs. 10.98 μg/mL, P < 0.001). Herein, the detection of trough concentration of rituximab was strongly recommended as an early indicator for clinical response, which was also very convenient.
The key role of the trough rituximab concentration in the first cycle on treatment response was first suggested in this study, but this conclusion was not contrary to the results of previous studies. In a large rituximab PK study [12], 166 recurrent or refractory low-grade non-Hodgkin lymphoma treated with rituximab at 375 mg/m2 once weekly for four doses, concentrations before the second infusion (corresponding to C1-trough in this study) of the responders were significantly higher than nonresponders (71.30 μg/mL vs. 57.90 μg/mL, P = 0.006), and the difference did not reach significance in the subsequent cycles until the end of treatment, even though the administration interval was very different from that in this study, the remarkable ability of the initial trough concentrations to predict response was the same. In Jager et al.’s study [13], 17 previously untreated advanced FL with grade 1 or 2 received R-FC every 28 days, trough concentrations of rituximab before cycles 2 (corresponding to C1-trough in this study), 4 and 6 were also detected, and the difference in the trough concentrations between the CR and PR groups was large before cycle 2, but this distance disappeared in the subsequent treatment (before cycle 2: 19.18 μg/mL vs. 2.88 μg/mL; before cycle 4: 65.70 μg/mL vs. 32.93 μg/mL; before cycle 6: 65.87 μg/mL vs. 57.35 μg/mL). This phenomenon was also very similar to our result. The authors also advocated that, since Ctrough levels in CR versus PR patients differed as early as after the first cycle of therapy, an increase in rituximab dosage in the initial induction treatment seems necessary.
In this study, rituximab was administered every 21 days, and the differences in trough concentrations between the CR and non-CR groups reached statistical significance in 1–3 cycles, but logistic regression analysis suggested that only trough concentration in cycle 1 was significantly associated with achieving CR. The recommended minimum optimal C1-trough was 13.60 μg/mL, which was also consistent with the previous study that whole blood complement-dependent cytotoxicity occurred at optimal levels equal to or greater than 10 μg/mL [24, 25].
The explanation for the key role of C1-trough may be that the concentration measured only reflects free antibody, not bound antibody. It is therefore unlikely that sustained high levels will confer a superior therapeutic benefit because the mechanism of action of rituximab is mediated by binding to the target. Another possible explanation was that 21 days after the first infusion, the amount of the remaining free rituximab (the C1-trough) may depend on many factors, including the true level of tumor burden in the body; the sensitivity of the tumor to the therapeutic drugs, which is expected to decrease tumor burden (the target); the clearance rate of the antibody, which reflects the endogenous metabolic capability; and even something beyond current knowledge. These factors may determine the treatment response; in addition to inducing pharmacological action at a necessary level, the C1-trough also reflects the individual differences of these factors, and the subsequent accumulation of concentrations resulting from continuous administration may mask the changes in these factors. Herein, the rituximab C1-trough would thus be expected to vary substantially between different kinds of patients and could then be used as a distinctive outcome predictor.
The initial rituximab trough concentration was significantly lower in patients with grade 1/2 FL than in those with grade 3 FL (12.21 μg/mL vs. 23.45 μg/mL, P < 0.001). For grades 1 and 2, watching and waiting or involved site radiation therapy for all involved tumor sites is the preferred option, and only patients who present with a disseminated disease (i.e., advanced stage) require systemic therapy [1, 26]. Tumor burden explained a large part of the variability in rituximab concentration, which may be explained by increased rituximab clearance related to its elimination by the target antigen. In our multiple linear regression analysis, 40.7% of C1-trough variability could be explained by the different stages, which were classified mainly based on tumor burden and location. Tout et al.’s study [14] reported similar results, with baseline total metabolic tumor volume accounting for 41% of AUC1 variability. In this study, 70% of patients with grade 1/2 FL were stage IV, and among them, only 30% of patients could reach 13.60 μg/mL in cycle 1, which was in accordance with its unsatisfactory CR rates compared with grade 3 (43.33% vs. 76.32%); 91.67% of patients with grade 3 FL reached this threshold. Although there may be other unknown factors accounting for the lower rituximab C1-trough for low-grade FL, the conventional dosage of 375 mg/m2 is not sufficient for low-grade patients, and a higher loading dose of rituximab should be considered for neutralizing the higher tumor burden.
Although the sampling scheme was limited to two concentrations per cycle per patient in this study, a two-compartment PK model described the data well, and the final PK parameters were consistent with the results of previous studies for rituximab [14, 19, 27]. For patients with grade 1/2 FL, 1800 mg could induce ~90% of patients to obtain sufficient initial levels based on our model. Since a dose-escalation trial of rituximab from 500 to 2250 mg/m2 has been designed in chronic lymphocytic leukemia, toxicity was minimal until a dose of 2250 mg/m2 was achieved, so our recommended initial dosage of rituximab is acceptable [28].
This study has several limitations. A modest sample size of 68 patients was used in this study. Low-grade FL is characterized by a chronic relapsing remitting disease course, which might lead to difficulty in reaching CR. However, the matched-pair logistic regression analysis controlling for the effect of tumor stage and grade confirmed the independent role of the C1-trough on the clinical response. It is more likely that the higher C1-trough may actually mediate more effective tumor regression. Therefore, further studies are needed to verify the benefit of increasing the dosage of rituximab for low-grade patients.
Conclusion
In general, this study first suggested that the majority of low-grade FL patients could not reach the minimum effective concentration under the conventional dosage of 375 mg/m2 of rituximab, and an insufficient initial concentration was a significant risk factor for an unsatisfactory first-line R-CHOP treatment response. The prevalent advanced stage at the beginning of systemic treatment was confirmed as a factor for the insufficient concentration. Therefore, designing the first dosage of rituximab should be a very important component of individualized therapy for FL.
References
Dada R. Diagnosis and management of follicular lymphoma: a comprehensive review. Eur J Haematol. 2019;103:152–63.
Martin AR, Weisenburger DD, Chan WC, Ruby EI, Anderson JR, Vose JM, et al. Prognostic value of cellular proliferation and histologic grade in follicular lymphoma. Blood. 1995;85:3671–8.
Relander T, Johnson NA, Farinha P, Connors JM, Sehn LH, Gascoyne RD. Prognostic factors in follicular lymphoma. J Clin Oncol. 2010;28:2902–13.
Jaffe ES. The 2008 WHO classification of lymphomas: implications for clinical practice and translational research. Eur. J. Haematol. 2008;80:523–31.
Katzenberger T, Ott G, Klein T, Kalla J, Muller-Hermelink HK, Ott MM. Cytogenetic alterations affecting BCL6 are predominantly found in follicular lymphomas grade 3B with a diffuse large B-cell component. Am J Pathol. 2004;165:481–90.
Horn H, Schmelter C, Leich E, Salaverria I, Katzenberger T, Ott MM, et al. Follicular lymphoma grade 3B is a distinct neoplasm according to cytogenetic and immunohistochemical profiles. Haematologica. 2011;96:1327–34.
Flinn IW, van der Jagt R, Kahl BS, Wood P, Hawkins TE, Macdonald D, et al. Randomized trial of bendamustine-rituximab or R-CHOP/R-CVP in first-line treatment of indolent NHL or MCL: the BRIGHT study. Blood. 2014;123:2944–52.
Rummel MJ, Niederle N, Maschmeyer G, Banat GA, von Grunhagen U, Losem C, et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet. 2013;381:1203–10.
Huttmann A, Rekowski J, Muller SP, Hertenstein B, Franzius C, Mesters R, et al. Six versus eight doses of rituximab in patients with aggressive B cell lymphoma receiving six cycles of CHOP: results from the “Positron Emission Tomography-Guided Therapy of Aggressive Non-Hodgkin Lymphomas” (PETAL) trial. Ann Hematol. 2019;98:897–907.
Wahlin BE, Sundstrom C, Sander B, Christensson B, Jeppsson-Ahlberg A, Hjalmarsson E, et al. Higher world health organization grades of follicular lymphoma correlate with better outcome in two Nordic Lymphoma Group trials of rituximab without chemotherapy. Leuk Lymphoma. 2014;55:288–95.
Golay J, Semenzato G, Rambaldi A, Foa R, Gaidano G, Gamba E, et al. Lessons for the clinic from rituximab pharmacokinetics and pharmacodynamics. MAbs. 2013;5:826–37.
Berinstein NL, Grillo-Lopez AJ, White CA, Bence-Bruckler I, Maloney D, Czuczman M, et al. Association of serum Rituximab (IDEC-C2B8) concentration and anti-tumor response in the treatment of recurrent low-grade or follicular non-Hodgkin’s lymphoma. Ann Oncol. 1998;9:995–1001.
Jager U, Fridrik M, Zeitlinger M, Heintel D, Hopfinger G, Burgstaller S, et al. Rituximab serum concentrations during immuno-chemotherapy of follicular lymphoma correlate with patient gender, bone marrow infiltration and clinical response. Haematologica. 2012;97:1431–8.
Tout M, Casasnovas O, Meignan M, Lamy T, Morschhauser F, Salles G, et al. Rituximab exposure is influenced by baseline metabolic tumor volume and predicts outcome of DLBCL patients: a Lymphoma Study Association report. Blood. 2017;129:2616–23.
Tran L, Baars JW, Aarden L, Beijnen JH, Huitema AD. Pharmacokinetics of rituximab in patients with CD20 positive B-cell malignancies. Hum Antib. 2010;19:7–13.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Munekage M, Ichikawa K, Kitagawa H, Ishihara K, Uehara H, Watanabe J, et al. Population pharmacokinetic analysis of daikenchuto, a traditional Japanese medicine (Kampo) in Japanese and US health volunteers. Drug Metab Dispos. 2013;41:1256–63.
Song L, He CY, Yin NG, Liu F, Jia YT, Liu Y. A population pharmacokinetic model for individualised dosage regimens of vancomycin in Chinese neonates and young infants. Oncotarget. 2017;8:105211–21.
Candelaria M, Gonzalez D, Fernandez Gomez FJ, Paravisini A, Del Campo Garcia A, Perez L, et al. Comparative assessment of pharmacokinetics, and pharmacodynamics between RTXM83, a rituximab biosimilar, and rituximab in diffuse large B-cell lymphoma patients: a population PK model approach. Cancer Chemother Pharmacol. 2018;81:515–27.
Brendel K, Comets E, Laffont C, Laveille C, Mentre F. Metrics for external model evaluation with an application to the population pharmacokinetics of gliclazide. Pharmacol Res. 2006;23:2036–49.
Koletsi D, Pandis N. Conditional logistic regression. Am J Orthod Dentofac Orthop. 2017;151:1191–2.
Tobinai K, Igarashi T, Itoh K, Kobayashi Y, Taniwaki M, Ogura M, et al. Japanese multicenter phase II and pharmacokinetic study of rituximab in relapsed or refractory patients with aggressive B-cell lymphoma. Ann Oncol. 2004;15:821–30.
Li J, Zhi J, Wenger M, Valente N, Dmoszynska A, Robak T, et al. Population pharmacokinetics of rituximab in patients with chronic lymphocytic leukemia. J Clin Pharmacol. 2012;52:1918–26.
Bologna L, Gotti E, Da Roit F, Intermesoli T, Rambaldi A, Introna M, et al. Ofatumumab is more efficient than rituximab in lysing B chronic lymphocytic leukemia cells in whole blood and in combination with chemotherapy. J Immunol. 2013;190:231–9.
Bologna L, Gotti E, Manganini M, Rambaldi A, Intermesoli T, Introna M, et al. Mechanism of action of type II, glycoengineered, anti-CD20 monoclonal antibody GA101 in B-chronic lymphocytic leukemia whole blood assays in comparison with rituximab and alemtuzumab. J Immunol. 2011;186:3762–9.
Cheah CY, Chihara D, Ahmed M, Davis RE, Nastoupil LJ, Phansalkar K, et al. Factors influencing outcome in advanced stage, low-grade follicular lymphoma treated at MD Anderson Cancer Center in the rituximab era. Ann Oncol. 2016;27:895–901.
Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–59.
O’Brien SM, Kantarjian H, Thomas DA, Giles FJ, Freireich EJ, Cortes J, et al. Rituximab dose-escalation trial in chronic lymphocytic leukemia. J Clin Oncol. 2001;19:2165–70.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81730103, 81473283, 81973398, 81573507); Higher Education Discipline Innovation Project (the 111 Project, No. B16047); the Natural Science Foundation of Guangdong Province (No. 2019A1515010742); and Wu Jie-ping Medical Foundation of Clinical Pharmacy (No. 320.6750.19090-14).
Author information
Authors and Affiliations
Contributions
TYL, XDW, MH, and SL designed the research, analyzed data, and wrote the manuscript; TYL, HH, CP, ZW, XJF, QGR, and YYY contributed study materials/patients and collected, analyzed, and interpreted data; SL, RXC, YPG, ZJC, SXG, and XZ performed experiments; SL, YPG, and RXC performed PK and statistical analyses; and RXC, HH, HBH, and MH reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Liu, S., Huang, H., Chen, Rx. et al. Low initial trough concentration of rituximab is associated with unsatisfactory response of first-line R-CHOP treatment in patients with follicular lymphoma with grade 1/2. Acta Pharmacol Sin 42, 641–647 (2021). https://doi.org/10.1038/s41401-020-0479-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-020-0479-2
Keywords
This article is cited by
-
The Influence of Underlying Disease on Rituximab Pharmacokinetics May be Explained by Target-Mediated Drug Disposition
Clinical Pharmacokinetics (2022)