Abstract
Study design
A retrospective cross-sectional study.
Objective
To identify who prescribes outpatient antibiotics among a primary care spinal cord injury (SCI) cohort.
Setting
ICES databases in Ontario, Canada.
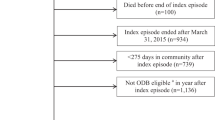
Methods
A cohort of individuals with SCI were retrospectively identified using a tested-algorithm and chart reviews in a primary care electronic medical records database. The cohort was linked to a drug dispensing database to obtain outpatient antibiotic prescribing information, and prescriber details were obtained from a physician database.
Results
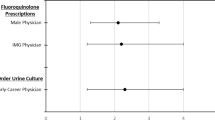
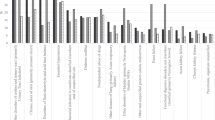
Final cohort included three hundred and twenty individuals with SCI. The average annual number of antibiotic courses dispensed for the SCI cohort was 2.0 ± 6.2. For dispensed antibiotics, 58.9% were prescribed by rostered-primary care practice physicians, compared to 17.9% by emergency and non-rostered primary care physicians, 17.4% by specialists and 6.1% by non-physician prescribers. Those who lived in urban areas and rural areas, compared to those who lived in suburban areas, were more likely to receive antibiotics from emergency and non-rostered primary care physicians than from rostered-primary care practice physicians.
Conclusion
Although individuals with SCI received outpatient antibiotic prescriptions from multiple sources, physicians from an individual’s rostered-primary care practice were the main antibiotic prescribers. As such, interventions to optimize antibiotics use in the SCI population should target the primary care practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
References
Suda KJ, Patel UC, Sabzwari R, Cao L, Ramanathan S, Hill JN, et al. Bacterial susceptibility patterns in patients with spinal cord injury and disorder (SCI/D): an opportunity for customized stewardship tools. Spinal Cord. 2016;54:1001–9.
Salameh A, Mohajer MA, Daroucihe RO. Prevention of urinary tract infections in patients with spinal cord injury. Can Med Assoc J. 2015;187:807–11.
Abbasi F, Korooni S Infectious Complications after Spinal Cord Injury. In: Dionyssiotis Y (ed). Essentials of Spinal Cord Injury Medicine. InTech, 2018 https://doi.org/10.5772/intechopen.72783.
Evans C, Weaver F, Rogers T, Rapacki L, Miskevics S, Hahm B, et al. Guideline-recommended management of community-acquired pneumonia in veterans with spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18:300–5.
Heym B, Rimareix F, Lortat-Jacob A, Nicolas-Chanoine M-H. Bacteriological investigation of infected pressure ulcers in spinal cord-injured patients and impact on antibiotic therapy. Spinal Cord. 2004;42:230–4.
Fitzpatrick MA, Suda KJ, Safdar N, Burns SP, Jones MM, Poggensee L, et al. Changes in bacterial epidemiology and antibiotic resistance among veterans with spinal cord injury/disorder over the past 9 years. J Spinal Cord Med. 2018;41:199–207.
Evans CT, Fitzpatrick MA, Jones MM, Burns SP, Poggensee L, Ramanathan S, et al. Prevalence and Factors Associated With Multidrug-Resistant Gram-Negative Organisms in Patients With Spinal Cord Injury. Infect Control Hosp Epidemiol. 2017;38:1464–71.
Yoon SB, Lee BS, Lee KD, Hwang SI, Lee HJ, Han ZA. Comparison of bacterial strains and antibiotic susceptibilities in urinary isolates of spinal cord injury patients from the community and hospital. Spinal Cord. 2014;52:298–301.
Garcia-Arguello LY, O’Horo JC, Farrell A, Blakney R, Sohail MR, Evans CT, et al. Infections in the spinal cord-injured population: a systematic review. Spinal Cord. 2017;55:526–34.
Wong S, Santullo P, O’Driscoll J, Jamous A, Hirani SP, Saif M. Use of antibiotic and prevalence of antibiotic-associated diarrhoea in-patients with spinal cord injuries: a UK national spinal injury centre experience. Spinal Cord. 2017;55:583–7.
Bayoumi I, Dolovich L, Hutchison B, Holbrook A. Medication-related emergency department visits and hospitalizations among older adults. Can Fam Physician. 2014;60:e217–22.
McColl MA, Aiken A, McColl A, Sakakibara B, Smith K. Primary care of people with spinal cord injury: scoping review. Can Fam Physician. 2012;58:1207–16.
Donnelly C, McColl MA, Charlifue S, Glass C, O’Brien P, Savic G, et al. Utilization, access and satisfaction with primary care among people with spinal cord injuries: a comparison of three countries. Spinal Cord. 2007;45:25–36.
Lofters A, Chaudhry M, Slater M, Schuler A, Milligan J, Lee J, et al. Preventive care among primary care patients living with spinal cord injury. J Spinal Cord Med. 2019;42:702–8.
Milligan J, Lee J, Hillier LM, Slonim K, Craven C. Improving primary care for persons with spinal cord injury: development of a toolkit to guide care. J Spinal Cord Med. 2020;43:364–73.
Munce SEP, Guilcher SJT, Couris CM, Fung K, Craven BC, Verrier M, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord. 2009;47:470–6.
Guilcher SJT, Craven BC, Calzavara A, McColl MA, Jaglal SB. Is the emergency department an appropriate substitute for primary care for persons with traumatic spinal cord injury? Spinal Cord. 2013;51:202–8.
Evans CT, Rogers TJ, Chin A, Johnson S, Smith B, Weaver FM, et al. Antibiotic prescribing trends in the emergency department for veterans with spinal cord injury and disorder 2002-2007. J Spinal Cord Med. 2013;36:492–8.
Fan VS, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20:226–33.
Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8:e021161.
McIsaac WJ, Fuller-Thomson CE, Talbot Y. Does having regular care by a family physician improve preventive care? Can Fam Phys.47:70–76.
Saultz JW. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3:159–66.
Baker R, Freeman GK, Haggerty JL, Bankart MJ, Nockels KH. Primary medical care continuity and patient mortality: a systematic review. Br J Gen Pr. 2020;70:e600–e611.
Van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review: Association between continuity of care and outcomes. J Eval Clin Pr. 2010;16:947–56.
Senthinathan A, Craven BC, Morris AM, Penner M, Tu K, Jaglal SB. Examining antibiotic prescribing and urine culture testing for urinary tract infections (UTIs) in a primary care spinal cord injury (SCI) cohort. Spinal Cord. 2023. https://doi.org/10.1038/s41393-023-00899-x.
ICES Data Dictionary online.
Singh J, Dahrouge S, Green ME. The impact of the adoption of a patient rostering model on primary care access and continuity of care in urban family practices in Ontario, Canada. BMC Fam Pract. 2019;20:52.
Kralji B. Measuring Rurality – RIO2008BASIC: Methodology and Results. [Toronto: Ontario Medical Association; 2008.]. https://www.oma.org/uploadedfiles/oma/media/pagetree/expert--advice/2008rio-fulltechnicalpaper.pdf. Accessed 20 Jan 2024. Toronto: OMA Department of Economics; 2009.
Senthinathan A, Tu K, Penner M, Morris AM, Craven BC, Jaglal SB Identifying Patterns of Antibiotic Prescribing for a Primary Care Spinal Cord Injury (SCI) Cohort using an Electronic Medical Records (EMR) Database [Manuscript submitted for publication]. Inst Health Policy Manag Eval Univ Tor 2022.
Senthinathan A Using Clinical Vignettes and a Modified Expert Delphi Panel to Determine Parameters for Identifying Non-Traumatic Spinal Cord Injury in Health Administrative and Electronic Medical Record Databases. https://doi.org/10.1016/j.apmr.2022.08.002.
Schwartz KL, Wilton AS, Langford BJ, Brown KA, Daneman N, Garber G, et al. Comparing prescribing and dispensing databases to study antibiotic use: a validation study of the Electronic Medical Record Administrative data Linked Database (EMRALD). J Antimicrob Chemother. 2019;74:2091–7.
O’Malley AS, Cunningham PJ. Patient experiences with coordination of care: the benefit of continuity and primary care physician as referral source. J Gen Intern Med. 2009;24:170–7.
Anderson LH, Flottemesch TJ, Fontaine P, Solberg LI, Asche SE. Patient medical group continuity and healthcare utilization. Am J Manag Care. 2012;18:450–7. https://www.ajmc.com/view/patient-medical-group-continuity-and-healthcare-utilization.
Haggerty JL, Roberge D, Lévesque J-F, Gauthier J, Loignon C. An exploration of rural–urban differences in healthcare-seeking trajectories: Implications for measures of accessibility. Health Place. 2014;28:92–98.
Khoong EC, Gibbert WS, Garbutt JM, Sumner W, Brownson RC. Rural, suburban, and urban differences in factors that impact physician adherence to clinical preventive service guidelines: rural-urban impact on guideline adherence. J Rural Health. 2014;30:7–16.
Peterson LE, Dodoo M, Bennett KJ, Bazemore A, Phillips RL. Nonemergency medicine-trained physician coverage in rural emergency departments. J Rural Health. 2008;24:183–8.
Acknowledgements
This study was supported by the ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). We thank IQVIA Solutions Canada Inc. for use of their Drug Information File. Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed in the material are those of the authors, and not necessarily those of CIHI. Thank you to Jun Guan, Zhiyin Li, and staff at ICES for their contributions to this paper.
Author information
Authors and Affiliations
Contributions
All authors contributed to the development of this paper, its study design and interpretation of results. AS conceptualized the study, analyzed the data, interpreted results, and wrote the manuscript. SBJ guided the data analyses and development of manuscript. SBJ, KT, MP, AMM, and BCC helped with the overall interpretation of findings, as well as reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require further review by a Research Ethics Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Senthinathan, A., Penner, M., Tu, K. et al. Identifying prescribers of antibiotics in a primary care spinal cord injury cohort. Spinal Cord Ser Cases 10, 3 (2024). https://doi.org/10.1038/s41394-024-00615-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-024-00615-8