Abstract
Objective
To determine whether duration of detrusor overactivity (DO) during a cystometric study is an independent predictive factor of upper urinary tract deterioration (UUTD) in patients with traumatic spinal cord injury (TSCI).
Study design
Retrospective cohort study.
Setting
A rehabilitation facility in Chiang Mai, Thailand.
Methods
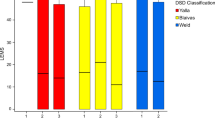
Data were obtained from medical records of patients who underwent cystometric evaluation at 6–12 months after TSCI. The independent predictor of interest is the duration of DO, which was evaluated by the DO/cystometry ratio (DOratio). Other conventional urodynamic parameters (maximum detrusor pressure, cystometric capacity, bladder compliance, and detrusor-sphincter dyssynergia) and clinical parameters (age, sex, level and severity of injury, comorbidities, bladder emptying method, and history of urinary tract infection) were determined. The outcome was UUTD, which is indicated by chronic kidney disease (GFR < 60 ml/min/1.73 m2), hydronephrosis, and/or vesicoureteral reflux. Multivariable Cox regression analysis was used to determine the independent associations between DOratio and UUTD by adjusting with all other parameters.
Results
Medical records of 194 patients with TSCI were included in the study. During a combined total of 1260 follow-up years of those patients, 34 UUTD events were identified, indicating an incidence rate of 27.0 cases per 1000 person-years. After adjusting for all other parameters, a high DOratio (≥0.33) was significantly associated with UUTD (hazard ratio = 3.00 [95% CI: 1.12–7.99], p = 0.025).
Conclusion
DOratio may be an independent cystometric predictor of UUTD in patients with TSCI. However, further prospective study is needed prior to applying DOratio as a predictor of UUTD in clinical settings.
Clinical trial registration
There was no clinical trial registration since this study is not a clinical trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during this study are available from the corresponding author upon reasonable request.
References
Myers JB, Lenherr SM, Stoffel JT, Elliott SP, Presson AP, Zhang C, et al. Patient reported bladder related symptoms and quality of life after spinal cord injury with different bladder management strategies. J Urol. 2019;202:574–84.
DeVivo MJ, Chen Y, Wen H. Cause of death trends among persons with spinal cord injury in the United States: 1960-2017. Arch Phys Med Rehabil. 2022;103:634–41.
Drake MJ, Apostolidis A, Cocci A, Emmanuel A, Gajewski JB, Harrison SC, et al. Neurogenic lower urinary tract dysfunction: clinical management recommendations of the Neurologic Incontinence committee of the fifth International Consultation on Incontinence 2013. Neurourol Urodyn. 2016;35:657–65.
Pavese C, Schneider MP, Schubert M, Curt A, Scivoletto G, Finazzi-Agrò E, et al. Prediction of bladder outcomes after traumatic spinal cord injury: a longitudinal cohort study. PLoS Med. 2016;13:e1002041.
Birkhäuser V, Anderson CE, Kozomara M, Bywater M, Gross O, Kiss S, et al. Urodynamics are essential to predict the risk for upper urinary tract damage after acute spinal cord injury. Biomedicines. 2023;11:1748.
Gerridzen RG, Thijssen AM, Dehoux E. Risk factors for upper tract deterioration in chronic spinal cord injury patients. J Urol. 1992;147:416–8.
Shin JC, Lee Y, Yang H, Kim DH. Clinical significance of urodynamic study parameters in maintenance of renal function in spinal cord injury patients. Ann Rehabil Med. 2014;38:353–9.
Pavese C, Kessler TM. Prediction of lower urinary tract, sexual, and bowel function, and autonomic dysreflexia after spinal cord injury. Biomedicines. 2023;11:1644.
Çetinel B, Önal B, Can G, Talat Z, Erhan B, Gündüz B. Risk factors predicting upper urinary tract deterioration in patients with spinal cord injury: a retrospective study. Neurourol Urodyn. 2017;36:653–8.
Weld KJ, Graney MJ, Dmochowski RR. Differences in bladder compliance with time and associations of bladder management with compliance in spinal cord injured patients. J Urol. 2000;163:1228–33.
Stoffel JT. Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies. Transl Androl Urol. 2016;5:127–35.
Elmelund M, Klarskov N, Bagi P, Oturai PS, Biering-Sørensen F. Renal deterioration after spinal cord injury is associated with length of detrusor contractions during cystometry-a study with a median of 41 years follow-up. Neurourol Urodyn. 2017;36:1607–15.
Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745.
Gajewski JB, Schurch B, Hamid R, Averbeck M, Sakakibara R, Agrò EF, et al. An International Continence Society (ICS) report on the terminology for adult neurogenic lower urinary tract dysfunction (ANLUTD). Neurourol Urodyn. 2018;37:1152–61.
Romagnani P, Remuzzi G, Glassock R, Levin A, Jager KJ, Tonelli M, et al. Chronic kidney disease. Nat Rev Dis Prim. 2017;3:17088.
Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
Zhang Z, Liao L. Risk factors predicting upper urinary tract deterioration in patients with spinal cord injury: a prospective study. Spinal Cord. 2014;52:468–71.
Weiss DJ, Fried GW, Chancellor MB, Herbison GJ, Ditunno JF Jr, Staas WE Jr. Spinal cord injury and bladder recovery. Arch Phys Med Rehabil. 1996;77:1133–5.
Sirasaporn P, Saengsuwan J. Incidence and predictive factors for developing vesicoureteric reflux in individuals with suprasarcral spinal cord injury: a historical cohort study. Spinal Cord. 2021;59:753–60.
Gormley EA. Urologic complications of the neurogenic bladder. Urol Clin North Am. 2010;37:601–7.
Pannek J, Kennelly M, Kessler TM, Linsenmeyer T, Wyndaele JJ, Biering-Sørensen F. International spinal cord injury urodynamic basic data set (version 2.0). Spinal Cord Ser Cases. 2018;4:98.
Liao L, Zhang F, Chen G. New grading system for upper urinary tract dilation using magnetic resonance urography in patients with neurogenic bladder. BMC Urol. 2014;14:38.
Sung BM, Oh DJ, Choi MH, Choi HM. Chronic kidney disease in neurogenic bladder. Nephrology. 2018;23:231–6.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–23.
Jenkins DG, Quintana-Ascencio PF. A solution to minimum sample size for regressions. PLoS ONE. 2020;15:e0229345.
Wu SY, Jhang JF, Liu HH, Chen JT, Li JR, Chiu B, et al. Long-term surveillance and management of urological complications in chronic spinal cord-injured patients. J Clin Med. 2022;11:7307.
Singh R, Rohilla RK, Sangwan K, Siwach R, Magu NK, Sangwan SS. Bladder management methods and urological complications in spinal cord injury patients. Indian J Orthop. 2011;45:141–7.
Higgins J, Morgan R, Rooney A, Taylor K, Thayer K, Silva R, et al. Risk of bias in non-randomized studies - of exposure (ROBINS-E). Launch version, 20 June 2023. Available from: https://www.riskofbias.info/welcome/robins-e-tool.
Acknowledgements
We would like to thank Professor Dr. Lamar Robert for English language editing assistance. We would like to extend our thanks to Ms. Chanapat Pateekhum from Faculty of Medicine, Chiang Mai University, for providing statistical advice. SP would also like to acknowledge the Swiss Government Excellence Scholarship 2022 postdoctoral fellowship.
Author information
Authors and Affiliations
Contributions
PK and MS designed the research question, collected and analyzed the data, and wrote the preliminary version of the manuscript. SP designed the research question, analyzed the data, wrote the preliminary version, and revised the final version of the manuscript. CA designed the research question, analyzed the data, and revised the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The authors certify that the protocol of this analysis was approved by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University, Thailand (Study No. REH-2562_06228). This study used deidentified retrospectively recorded data, therefore, informed consent is not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kammuang-lue, P., Pattanakuhar, S., Sermsuk, M. et al. Duration of detrusor overactivity as an independent predictive factor of upper urinary tract deterioration in patients with traumatic spinal cord injury: results of a retrospective cohort study. Spinal Cord (2024). https://doi.org/10.1038/s41393-024-00988-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41393-024-00988-5